8 Signs Of High Cortisol & How To Reverse “Cortisol Face”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Shereene Idriss has insights about the facial features that might indicate chronically elevated cortisol levels, and what to do about same:
At face value
Dr. Idriss notes that for most people, this should not be cause for undue concern, although hypercortisolism can also be associated with genetic disorders such as Cushing’s syndrome, as well as prolonged use of certain medication, or the presence of certain tumors. As well as facial swelling, hypercortisolism can also result in other physical changes like acne, weight gain, skin thinning, stretch marks, infections, and hair loss.
As for what to do about it, she recommends addressing lifestyle factors like poor sleep, unhealthy diet, alcohol consumption, and lack of hydration to reduce facial puffiness related to stress. Diet suggestions include incorporating foods rich in magnesium, vitamin C, and omega-3s, such as leafy greens, fatty fish, nuts and seeds, and berries.
She also suggests some supplements to consider, such as ashwagandha, magnesium, omega-3s, and/or l-theanine, but you might want to speak to your doctor/pharmacist to check in case of contraindications per any other conditions you may have, or medications you may be on.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Lower Your Cortisol! (Here’s Why & How)
- Ashwagandha: The Root of All Even-Mindedness?
- L-Theanine: What’s The Tea?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Power Foods Diet – by Dr. Neal Barnard
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: it’s not a cookbook. There are recipes, more than a hundred if we consider such things as “barbecue sauce” as a standalone recipe, and if we overlook such things as how “perfect hot oatmeal” is followed on the next page by a recipe for “perfect hot oatmeal with berries”.
However, as we say, it’s not a cookbook; it’s first and foremost an educational text on the topic of nutrition.
Here we will learn about good eating for general health, which foods are natural appetite-suppressants, which foods reduce our body’s absorption of sugars from foods (not merely slowing, but flushing them away so they cannot be absorbed at all), and which foods actually boost metabolism for a few hours after the meal.
Dr. Barnard also talks about some foods that are more healthy, or less healthy, than popularly believed, and how to use all this information to craft a good, optimized, dietary plan for you.
Bottom line: there’s a lot of good information here, and the recipes are simply a bonus.
Click here to check out The Power Foods Diet, and optimize yours!
Share This Post
-
Antihistamines for Runny Nose?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Do you have any articles about using Anti-Histamines? My nose seems to be running a lot. I don’t have a cold or any allergies that I know of. I tried a Nasal spray Astepro, but it doesn’t do much.?❞
Just for you, we wrote such an article yesterday in response to this question!
The Astepro that you tried, by the way, is a brand name of the azelastine we mentioned near the end, before we got to talking about systemic corticosteroids such as beclometasone dipropionate—this latter might help you if antihistamines haven’t, and if your doctor advises there’s no contraindication (for most people it is safe for there are exceptions, such as if you are immunocompromised and/or currently fighting some infection).
You can find more details on all this in yesterday’s article, which in case you missed it, can be found at:
Antihistamines’ Generation Gap: Are You Ready For Allergy Season?
Enjoy!
Share This Post
-
Do We Need Sunscreen In Winter, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I keep seeing advice that we shoudl wear sunscreen out in winter even if it’s not hot or sunny, but is there actually any real benefit to this?❞
Short answer: yes (but it’s indeed not as critical as it is during summer’s hot/sunny days)
Longer answer: first, let’s examine the physics of summer vs winter when it comes to the sun…
In summer (assuming we live far enough from the equator to have this kind of seasonal variation), the part of the planet where we live is tilted more towards the sun. This makes it closer, and more importantly, it’s more directly overhead during the day. The difference in distance through space isn’t as big a deal as the difference in distance through the atmosphere. When the sun is more directly overhead, its rays have a shorter path through our atmosphere, and thus less chance of being blocked by cloud cover / refracted elsewhere / bounced back off into space before it even gets that far.
In winter, the opposite of all that is true.
Morning/evening also somewhat replicate this compared to midday, because the sun being lower in the sky has a similar effect to seasonal variation causing it to be less directly overhead.
For this reason, even though visually the sun may be just as bright on a winter morning as it is on a summer midday, the rays have been filtered very differently by the time they get to us.
This is one reason why you’re much less likely to get sunburned in the winter, compared to the summer (others include the actual temperature difference, your likely better hydration, and your likely more modest attire protecting you).
However…
The reason it is advisable to wear sunscreen in winter is not generally about sunburn, and is rather more about long-term cumulative skin damage (ranging from accelerated aging to cancer) caused by the UV rays—specifically, mostly UVA rays, since UVB rays (with their higher energy but shorter wavelength) have nearly all been blocked by the atmosphere.
Here’s a good explainer of that from the American Cancer Society:
UV (Ultraviolet) Radiation and Cancer Risk
👆 this may seem like a no-brainer, but there’s a lot explained here that demystifies a lot of things, covering ionizing vs non-ionizing radiation, x-rays and gamma-rays, the very different kinds of cancer caused by different things, and what things are dangerous vs which there’s no need to worry about (so far as best current science can say, at least).
Consequently: yes, if you value your skin health and avoidance of cancer, wearing sunscreen when out even in the winter is a good idea. Especially if your phone’s weather app says the UV index is “moderate” or above, but even if it’s “low”, it doesn’t hurt to include it as part of your skincare routine.
But what if sunscreens are dangerous?
Firstly, not all sunscreens are created equal:
Learn more: Who Screens The Sunscreens?
Secondly: consider putting on a protective layer of moisturizer first, and then the sunscreen on top. Bear in mind, this is winter we’re talking about, so you’re probably not going out in a bikini, so this is likely a face-neck-hands job and you’re done.
What about vitamin D?
Humans evolved to have more or less melanin in our skin depending on where we lived, and white people evolved to wring the most vitamin D possible out of the meagre sun far from the equator. Black people’s greater melanin, on the other hand, offers some initial protection against the sun (but any resultant skin cancer is then more dangerous than it would be for white people if it does occur, so please do use sunscreen whatever your skintone).
Nowadays many people live in many places which may or may not be the places we evolved for, and so we have to take that into account when it comes to sun exposure.
Here’s a deeper dive into that, for those who want to learn:
Take care!
Share This Post
Related Posts
-
Flossing Without Flossing?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Flossing Without Flossing?
You almost certainly brush your teeth. You might use mouthwash. A lot of people floss for three weeks at a time, often in January.
There are a lot of options for oral hygiene; variations of the above, and many alternatives too. This is a big topic, so rather than try to squeeze it all in one, this will be a several-part series.
The first part was: Toothpastes & Mouthwashes: Which Help And Which Harm?
How important is flossing?
Interdental cleaning is indeed pretty important, even though it may not have the heart health benefits that have been widely advertised:
However! The health of our gums is very important in and of itself, especially as we get older:
Flossing Is Associated with Improved Oral Health in Older Adults
But! It helps to avoid periodontal (e.g. gum) disease, not dental caries:
Flossing for the management of periodontal diseases and dental caries in adults
And! Most certainly it can help avoid a stack of other diseases:
Interdental Cleaning Is Associated with Decreased Oral Disease Prevalence
…so in short, if you’d like to have happy healthy teeth and gums, flossing is an important adjunct, and/but not a one-stop panacea.
Is it better to floss before or after brushing?
As you prefer. A team of scientists led by Dr. Claudia Silva studied this, and found that there was “no statistical difference between brush-floss and floss-brush”:
Flossing is tedious. How do we floss without flossing?
This is (mostly) about water-flossing! Which does for old-style floss what sonic toothbrushes to for old-style manual toothbrushes.
If you’re unfamiliar, it means using a device that basically power-washes your teeth, but with a very narrow high-pressure jet of water.
Do they work? Yes:
As for how it stacks up against traditional flossing, Liang et al. found:
❝In our previous single-outcome analysis, we concluded that interdental brushes and water jet devices rank highest for reducing gingival inflammation while toothpick and flossing rank last.
In this multioutcome Bayesian network meta-analysis with equal weight on gingival inflammation and bleeding-on-probing, the surface under the cumulative ranking curve was 0.87 for water jet devices and 0.85 for interdental brushes.
Water jet devices and interdental brushes remained the two best devices across different sets of weightings for the gingival inflammation and bleeding-on-probing. ❞
~ Journal of Evidence-Based Dental Practice
You may be wondering how safe it is if you have had dental work done, and, it appears to be quite safe, for example:
BDJ | Water-jet flossing: effect on composites
Want to try water-flossing?
Here are some examples on Amazon:
- Waterpik Complete Care 9.0 ← example of a top-end water-flossing device
- Philips Sonicare Power Flosser 3000 ← top-tier not-Waterpik-brand device
- INSMART Cordless Water Dental Flosser ← very low price and still average 4.5 star reviews, so in our opinion, a fine first choice
Bonus: if you haven’t tried interdental brushes, here’s an example for that
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
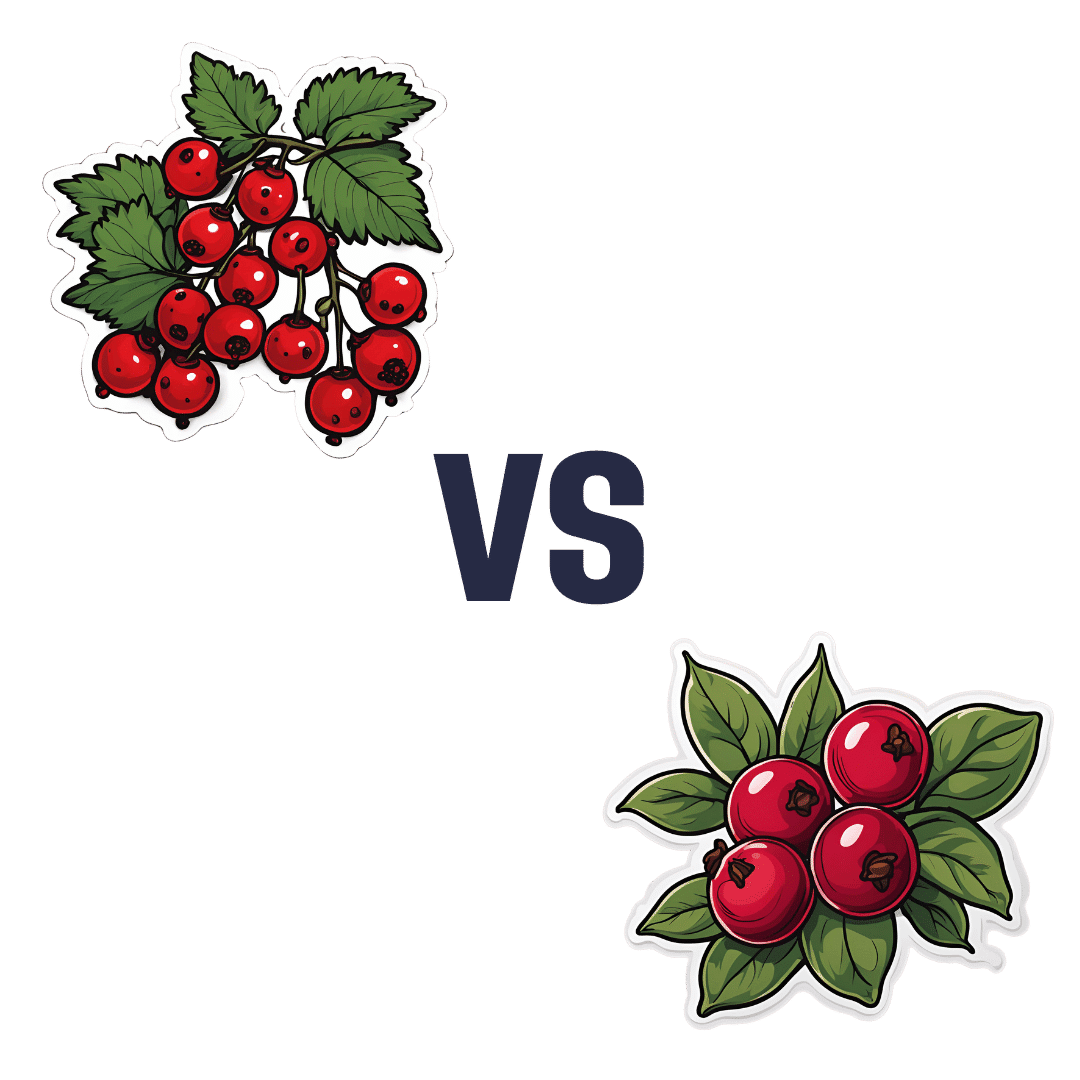
Redcurrants vs Cranberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing redcurrants to cranberries, we picked the redcurrants.
Why?
First know: here we’re comparing raw redcurrants to raw cranberries, with no additives in either case. If you buy jelly made from either, or if you buy dried fruits but the ingredients list has a lot of added sugar and often some vegetable oil, then that’s going to be very different. But for now… Let’s look at just the fruits:
In terms of macros, redcurrants are higher in carbs, but also higher in fiber, and have the lower glycemic index as cranberries have nearly 2x the GI.
When it comes to vitamins, redcurrants have more of vitamins B1, B2, B6, B9, C, K, and choline, while cranberries have more of vitamins A, B5, and E. In other words, a clear win for redcurrants.
In the category of minerals, redcurrants sweep even more convincingly with a lot more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc. On the other hand, cranberries boast a little more manganese; they also have about 2x the sodium.
Both berries have generous amounts of assorted phytochemicals (flavonoids and others), and/but nothing to set one ahead of the other.
As per any berries that aren’t poisonous, both of these are fine choices for most people most of the time, but redcurrants win with room to spare in most categories.
Want to learn more?
You might like to read:
Health Benefits Of Cranberries (But: You’d Better Watch Out)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
HIIT, But Make It HIRT
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This May HIRT A Bit
This is Ingrid Clay. She’s a professional athlete, personal trainer, chef*, and science writer.
*A vegan bodybuilding chef, no less:
Click Here If The Embedded Video Doesn’t Load Automatically!
For those who prefer reading…
This writer does too 😉
We’ve previously reviewed her book, “Science of HIIT”, and we’re going to be talking a bit about High Intensity Interval Training today.
If you’d like to know a little more about the woman herself first, then…
Centr | Meet Ingrid: Your HIIT HIRT trainer
Yes, that is Centr, as in Chris Hemsworth’s personal training app, where Clay is the resident HIIT & HIRT expert & trainer.
What’s this HIIT & HIRT?
“HIIT” is High Intensity Interval Training, which we’ve written about before:
How To Do HIIT (Without Wrecking Your Body)
Basically, it’s a super-efficient way of working out, that gets better results than working out for longer with other methods, especially because of how it raises the metabolism for a couple of hours after training (this effect is called EPOC, by the way—Excessive Post-exercise Oxygen Consumption), and is a good thing.
You can read more about the science of it, in the above-linked main feature.
And HIRT?
“HIRT” is High Intensity Resistance Training, and is resistance training performed with HIIT principles.
See also: Chris Hemsworth’s Trainer Ingrid Clay Explains HIRT
An example is doing 10 reps of a resistance exercise (e.g., a dumbbell press) every minute on odd-numbered minutes, and 10 reps of a different resistance exercise (e.g. dumbbell squats) on even-numbered minutes.
If dumbbells aren’t your thing, it could be resistance bands, or even the floor (press-ups are a resistance exercise!)
For HIRT that’s not also a cardio exercise, gaps between different exercises can be quite minimal, as we only need to confuse the muscles, not the heart. So, effectively, it becomes a specially focused kind of circuit training!
If doing planks though, you might want to check out Clay’s troubleshooting guide:
Want more from Clay?
Here she gives a full 20-minute full-body HIIT HIRT workout:
Click Here If The Embedded Video Doesn’t Load Automatically!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: