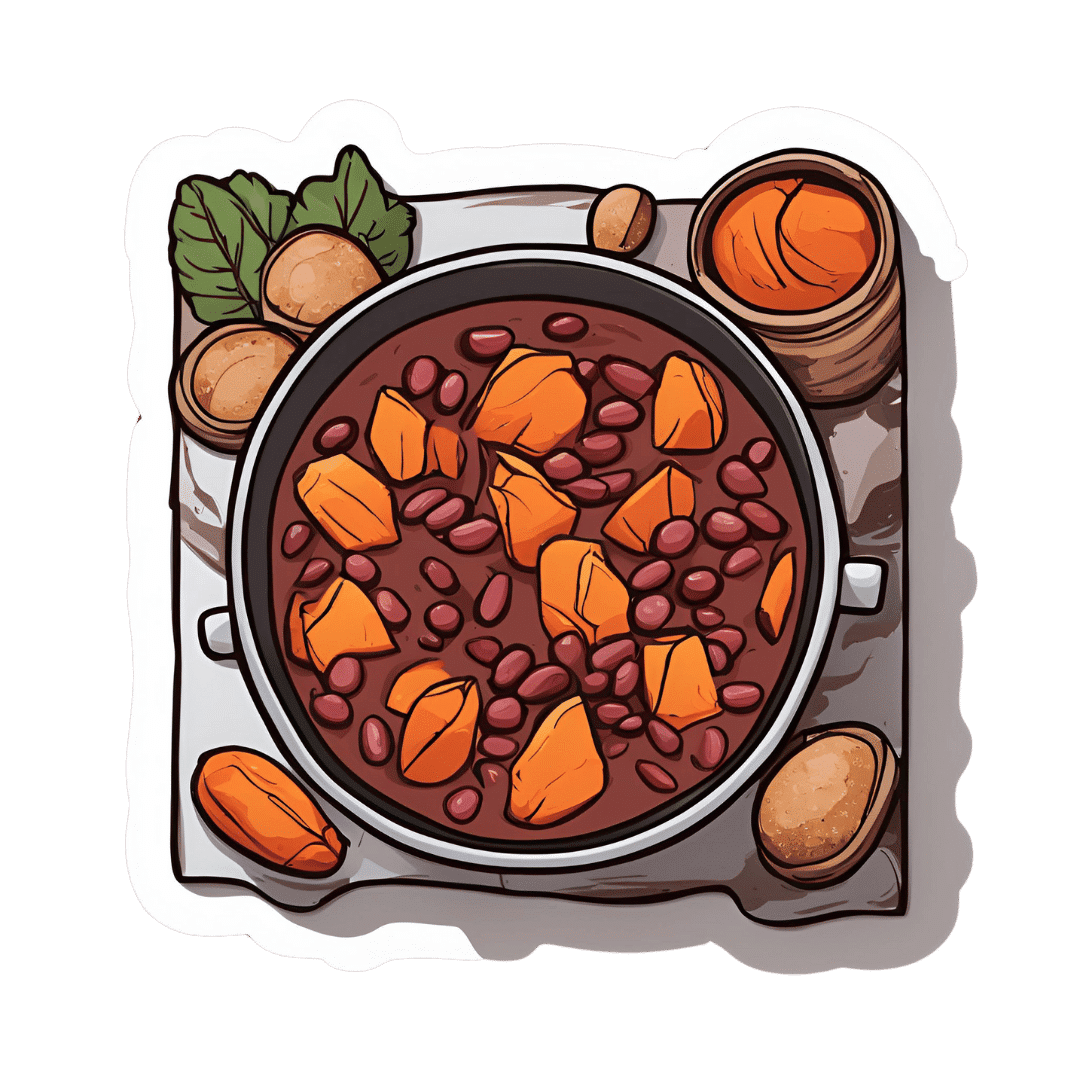
Ghanaian Red Bean & Sweet Potato Groundnut Stew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a dish popular in principle throughout West Africa. We say “in principle” because that’s a big place, and there is a lot of regional variation. The archetypal peanut stew is from Senegal (as maafe) or Mali (as tigadèguèna), but for its more balanced nutritional profile we’ve chosen one from Ghana—and since there are regional variations within Ghana too, we should specify that this one is from the south.
If you are allergic to nuts, you can substitute a seed butter (or tahini) for the nut butter, and omit the nuts—this will work in culinary terms and be fine healthwise, but we can’t claim it would be the same dish, having lost its defining ingredient. If your allergy is solely to peanuts, then substituting with any oily nut would work. So, not almonds for example, but cashews or even walnuts would be fine.
You will need
- 1½ lbs sweet potatoes, peeled and cut into ½” cubes
- 2 cups low-sodium vegetable stock
- 2 cans kidney beans, drained, cooked, and rinsed (or 2 cups same; cooked, drained, and rinsed)
- 1 can chopped tomatoes
- ½ cup unsalted dry-roasted peanuts
- 1 onion, chopped
- 1 red bell pepper, deseeded and chopped
- ¼ bulb garlic, finely chopped
- 2 heaped tbsp unsalted peanut butter, minimal (ideally: no) additives
- 2 tsp white miso paste
- 2 tsp grated fresh ginger
- 1 tsp ground cumin
- 1 tsp cayenne pepper
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- ½ tsp coarsely ground nigella seeds
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, or other pan suitable for both frying and fitting the entire stew in. Fry the onions until softened, turn the heat down low, and add the garlic, ginger, red bell pepper, cumin, cayenne, black pepper, and MSG/salt.
2) Add ¼ cup of the vegetable stock, and the sweet potato, and turn the heat back up, on high for about 30 seconds to get it to temperature, and then take it down to a simmer.
3) Stir in the miso paste and chopped tomatoes.
4) Add most of the rest of the vegetable stock, keeping ¼ cup aside. Simmer for about 20 minutes.
5) Stir in the kidney beans, and simmer for about 30 minutes more—the sweet potato should be soft now; if it isn’t, let it simmer a while longer until it is.
6) Combine the peanut butter with the remaining ¼ cup vegetable stock, and blend until smooth. Stir it into the stew.
7) If the stew is looking more like a soup than a stew, take out 1 cup and blend this 1 cup to a purée, adding it back in.
8) Add half the peanuts unto the stew. Taste, and adjust the seasonings if necessary.
9) Crush the remaining peanuts using a pestle and mortar; not too much though; you want them broken into bits, not pulverised.
10) Garnish with the crushed nuts and nigella seeds, and serve.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we used 4/5 today!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can I Eat That? – by Jenefer Roberts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The answer to the question in the title is: you can eat pretty much anything, if you’re prepared for the consequences!
This book looks to give you the information to make your own decisions in that regard. There’s a large section on the science of glucose metabolism in the context of food (other aspects of glucose metabolism aren’t covered), so you will not simply be told “raw carrots are good; mashed potatoes are bad”, you’ll understand many factors that affect it, e.g:
- Macronutrient profiles of food and resultant base glycemic indices
- How the glycemic index changes if you cut something, crush it, mash it, juice it, etc
- How the glycemic index changes if you chill something, heat it, fry it, boil it, etc
- The many “this food works differently in the presence of this other food” factors
- How your relative level of insulin resistance affects things itself
…and much more.
The style is simple and explanatory, without deep science, but with good science and comprehensive advice.
There are also the promised recipes; they’re in an appendix at the back and aren’t the main meat of the book, though.
Bottom line: if you’ve ever found it confusing working out what works how in the mysterious world of diabetes nutrition, this book is a top tier demystifier.
Click here to check out Can I Eat That?, and gain confidence in your food choices!
Share This Post
-
Metabolic Health Roadmap – by Brenda Wollenberg
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The term “roadmap” is often used in informative books, but in this case, Wollenberg (a nutritionist with decades of experience) really does deliver what can very reasonably be described as a roadmap:
She provides chapters in the form of legs of a journey [to better metabolic health], and those legs are broadly divided into an “information center” to deliver new information, a “rest stop” for reflection, “roadwork” to guide the reader through implementing the information we just learned, in a practical fashion, and finally “traveller assistance” to give additional support / resources, as well as any potential troubleshooting, etc.
The information and guidance within are all based on very good science; a lot is what you will have read already about blood sugar management (generally the lynchpin of metabolic health in general), but there’s also a lot about leveraging epigenetics for our benefit, rather than being sabotaged by such.
There’s a little guidance that falls outside of nutrition (sleep, exercise, etc), but for the most part, Wollenberg stays within her own field of expertise, nutrition.
The style is idiosyncratic; it’s very clear that her goal is providing the promised roadmap, and not living up to any editor’s wish or publisher’s hope of living up to industry standard norms of book formatting. However, this pays off, because her delivery is clear and helpful while remaining personable and yet still bringing just as much actual science, and this makes for a very pleasant and informative read.
Bottom line: if you’d like to improve your metabolic health, as well as get held-by-the-hand through your health-improvement journey by a charming guide, this is very much the book for you!
Click here to check out the Metabolic Health Roadmap, and start taking steps!
Share This Post
-
Yes, blue light from your phone can harm your skin. A dermatologist explains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Social media is full of claims that everyday habits can harm your skin. It’s also full of recommendations or advertisements for products that can protect you.
Now social media has blue light from our devices in its sights.
So can scrolling on our phones really damage your skin? And will applying creams or lotions help?
Here’s what the evidence says and what we should really be focusing on.
Max kegfire/Shutterstock Remind me, what actually is blue light?
Blue light is part of the visible light spectrum. Sunlight is the strongest source. But our electronic devices – such as our phones, laptops and TVs – also emit it, albeit at levels 100-1,000 times lower.
Seeing as we spend so much time using these devices, there has been some concern about the impact of blue light on our health, including on our eyes and sleep.
Now, we’re learning more about the impact of blue light on our skin.
How does blue light affect the skin?
The evidence for blue light’s impact on skin is still emerging. But there are some interesting findings.
1. Blue light can increase pigmentation
Studies suggest exposure to blue light can stimulate production of melanin, the natural skin pigment that gives skin its colour.
So too much blue light can potentially worsen hyperpigmentation – overproduction of melanin leading to dark spots on the skin – especially in people with darker skin.
Blue light can worsen dark spots on the skin caused by overproduction of melanin. DUANGJAN J/Shutterstock 2. Blue light can give you wrinkles
Some research suggests blue light might damage collagen, a protein essential for skin structure, potentially accelerating the formation of wrinkles.
A laboratory study suggests this can happen if you hold your device one centimetre from your skin for as little as an hour.
However, for most people, if you hold your device more than 10cm away from your skin, that would reduce your exposure 100-fold. So this is much less likely to be significant.
3. Blue light can disrupt your sleep, affecting your skin
If the skin around your eyes looks dull or puffy, it’s easy to blame this directly on blue light. But as we know blue light affects sleep, what you’re probably seeing are some of the visible signs of sleep deprivation.
We know blue light is particularly good at suppressing production of melatonin. This natural hormone normally signals to our bodies when it’s time for sleep and helps regulate our sleep-wake cycle.
By suppressing melatonin, blue light exposure before bed disrupts this natural process, making it harder to fall asleep and potentially reducing the quality of your sleep.
The stimulating nature of screen content further disrupts sleep. Social media feeds, news articles, video games, or even work emails can keep our brains active and alert, hindering the transition into a sleep state.
Long-term sleep problems can also worsen existing skin conditions, such as acne, eczema and rosacea.
Sleep deprivation can elevate cortisol levels, a stress hormone that breaks down collagen, the protein responsible for skin’s firmness. Lack of sleep can also weaken the skin’s natural barrier, making it more susceptible to environmental damage and dryness.
Can skincare protect me?
The beauty industry has capitalised on concerns about blue light and offers a range of protective products such as mists, serums and lip glosses.
From a practical perspective, probably only those with the more troublesome hyperpigmentation known as melasma need to be concerned about blue light from devices.
This condition requires the skin to be well protected from all visible light at all times. The only products that are totally effective are those that block all light, namely mineral-based suncreens or some cosmetics. If you can’t see the skin through them they are going to be effective.
But there is a lack of rigorous testing for non-opaque products outside laboratories. This makes it difficult to assess if they work and if it’s worth adding them to your skincare routine.
What can I do to minimise blue light then?
Here are some simple steps you can take to minimise your exposure to blue light, especially at night when it can disrupt your sleep:
- use the “night mode” setting on your device or use a blue-light filter app to reduce your exposure to blue light in the evening
- minimise screen time before bed and create a relaxing bedtime routine to avoid the types of sleep disturbances that can affect the health of your skin
- hold your phone or device away from your skin to minimise exposure to blue light
- use sunscreen. Mineral and physical sunscreens containing titanium dioxide and iron oxides offer broad protection, including from blue light.
In a nutshell
Blue light exposure has been linked with some skin concerns, particularly pigmentation for people with darker skin. However, research is ongoing.
While skincare to protect against blue light shows promise, more testing is needed to determine if it works.
For now, prioritise good sun protection with a broad-spectrum sunscreen, which not only protects against UV, but also light.
Michael Freeman, Associate Professor of Dermatology, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Codependency Isn’t What Most People Think It Is
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Codependency isn’t what most people think it is
In popular parlance, people are often described as “codependent” when they rely on each other to function normally. That’s interdependent mutualism, and while it too can become a problem if a person is deprived of their “other half” and has no idea how to do laundry and does not remember to take their meds, it’s not codependency.
Codependency finds its origins in the treatment and management of alcoholism, and has been expanded to encompass other forms of relationships with dependence on substances and/or self-destructive behaviors—which can be many things, including the non-physical, for example a pattern of irresponsible impulse-spending, or sabotaging one’s own relationship(s).
We’ll use the simplest example, though:
- Person A is (for example) an alcoholic. They have a dependency.
- Person B, married to A, is not an alcoholic. However, their spouse’s dependency affects them greatly, and they do what they can to manage that, and experience tension between wanting to “save” their spouse, and wanting their spouse to be ok, which latter, superficially, often means them having their alcohol.
Person B is thus said to be “codependent”.
The problem with codependency
The problems of codependency are mainly twofold:
- The dependent partner’s dependency is enabled and thus perpetuated by the codependent partner—they might actually have to address their dependency, if it weren’t for their partner keeping them from too great a harm (be it financially, socially, psychologically, medically, whatever)
- The codependent partner is not having a good time of it either. They have the stress of two lives with the resources (e.g. time) of one. They are stressing about something they cannot control, understandably worrying about their loved one, and, worse: every action they might take to “save” their loved one by reducing the substance use, is an action that makes their partner unhappy, and causes conflict too.
Note: codependency is often a thing in romantic relationships, but it can appear in other relationships too, e.g. parent-child, or even between friends.
See also: Development and validation of a revised measure of codependency
How to deal with this
If you find yourself in a codependent position, or are advising someone who is, there are some key things that can help:
- Be a nurturer, not a rescuer. It is natural to want to “rescue” someone we care about, but there are some things we cannot do for them. Instead, we must look for ways to build their strength so that they can take the steps that only they can take to fix the problem.
- Establish boundaries. Practise saying “no”, and also be clear over what things you can and cannot control—and let go of the latter. Communicate this, though. An “I’m not the boss of you” angle can prompt a lot of people to take more personal responsibility.
- Schedule time for yourself. You might take some ideas from our previous tangentially-related article:
How To Avoid Carer Burnout (Without Dropping Care)
Want to read more?
That’s all we have space for today, but here’s a very useful page with a lot of great resources (including questionnaires and checklist and things, in case you’re thinking “is it, or…?”)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chocolate & Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chocolate & Health: Fact or Fiction?
“Chocolate Is Good For The Heart”
“When making chocolate chip cookies, you don’t measure using cups, you measure by heart”
…but how good is chocolate when it comes to heart health?
First, what is heart health?
A healthy heart typically has a low resting pulse rate and a strong, steady beat. This is affected strongly by exercise habits, and diet plays only a support role (can’t exercise without energy from food!).
It is also important to have blood pressure within a healthy range (with high blood pressure being a more common problem than low, so things that lower blood pressure are generally considered good).
- Flavanols, flavonoids, and polyphenols in chocolate contribute to lower blood pressure
- Dark chocolate is best for these, as milk chocolate contains much less cocoa solids and more unhelpful fats
- White chocolate contains no cocoa solids and is useless for this
- Some of the fats in most commercial chocolate can contribute to atherosclerosis which raises blood pressure and ultimately can cause heart attacks.
- If you’re diabetic, you will probably not get the usual heart-related benefits from chocolate (sorry)
The Verdict: dark chocolate, in moderation, can support good heart health.
“Chocolate Is Good For The Brain”
Chocolate has been considered a “brain food”… why?
- The brain uses more calories than any other organ (chocolate has many calories)
- The heart benefits we listed above mean improved blood flow—including to your brain
- Chocolate contains phenylethylamine, a powerful chemical that has a similar effect to amphetamines… But it’s metabolized in digestion and never makes it to the central nervous system (so basically, this one’s a miss; we had a good run with the other two, though!)
The Verdict: dark chocolate, in moderation, can support good brain health
“Chocolate Is An Aphrodisiac”
“If chocolate be the food of love, pass me that cocoa; I’m starving”
Most excitingly, chocolate contains phenylethylamine, the “molecule of love” or, more accurately, lust. It has an effect similar to amphetamines, and while we can synthesize it in the body, we can also get it from certain foods. But…
Our body is so keen to get it that most of it is metabolized directly during digestion and doesn’t make it to the brain. Also, chocolate is not as good a source as cabbage—do with that information what you will!
However!
Chocolate contains theobromine and small amounts of caffeine, both stimulants and both generally likely to improve mood; it also contains flavonoids which in turn stimulate production of nitric oxide, which is a relaxant. All in all, things that are convivial to having a good time.
On the other hand…
That relaxation comes specifically with a reduction in blood pressure—something typically considered good for the health for most people most of the time… but that means lowering blood pressure in all parts of your body, which could be the opposite of what you want in intimate moments.
Chocolate also contains zinc, which is essential for hormonal health for most people—the body uses it to produce testosterone and estrogen, respectively. Zinc supplements are popularly sold to those wishing to have more energy in general and good hormonal health in particular, and rightly so. However…
This approach requires long-term supplementation—you can’t just pop a zinc tablet / bar of chocolate / almond before bed and expect immediate results. And if your daily zinc supplementation takes the form of a 3.5oz (100g) bar of chocolate, then you may find it has more effects on your health, and not all of them good!
The Verdict: dark chocolate, in moderation, may promote “the mood”, but could be a double-edged sword when it comes to “the ability”.
“Chocolate Is Good During Menstruation”
The popular wisdom goes that chocolate is rich in iron (of which more is needed during menstruation), and indeed, if you eat 7oz (150g) of dark chocolate made with 85% cocoa, you’ll get a daily a dose of iron (…and nearly 1,000 calories).
More bang-for-buck dietary sources of iron include chickpeas and broccoli, but for some mysterious reason, these are not as commonly reported as popular cravings.
The real explanation for chocolate cravings is more likely that eating chocolate—a food high in sugar and fat along with a chemical bombardment of more specialized “hey, it’s OK, you can relax now” molecules (flavanols/flavonoids, polyphenols, phenylamines, even phenylethylamine, etc) gives a simultaneous dopamine kick (the body’s main “reward” chemical) with a whole-body physiological relaxation… so, little wonder we might crave it in times of stress and discomfort!
The Verdict: it helps, not because it serves a special nutritional purpose, but rather, because the experience of eating chocolate makes us feel good.
Fun fact: Tiramisu (this writer’s favorite dessert) is literally Italian for “pick-me-up”
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
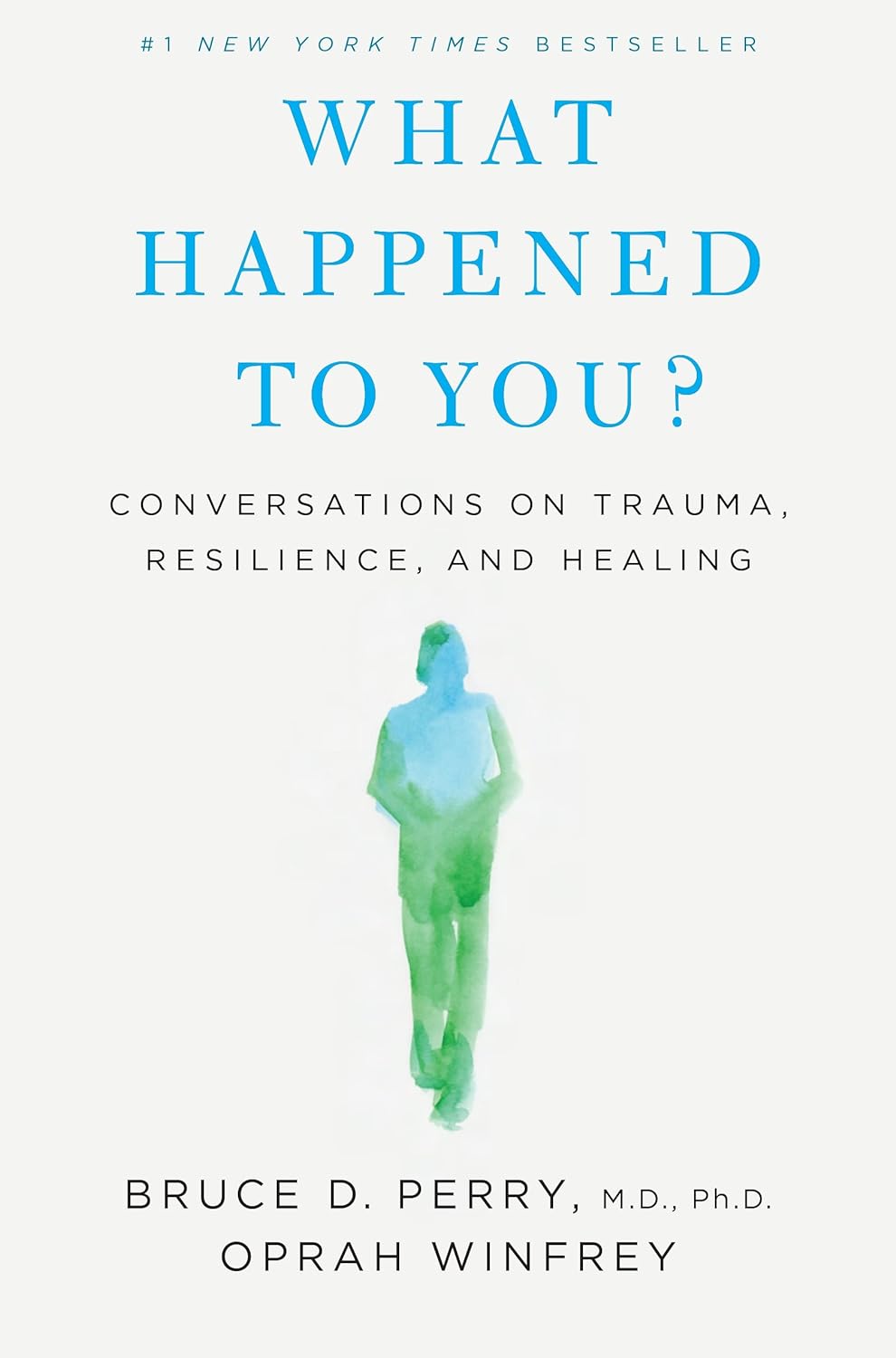
What Happened to You? – by Dr. Bruce Perry and Oprah Winfrey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The very title “What Happened To You?” starts with an assumption that the reader has suffered trauma. This is not just a sample bias of “a person who picks up a book about healing from trauma has probably suffered trauma”, but is also a statistically safe assumption. Around 60% of adults report having suffered some kind of serious trauma.
The authors examine, as the subtitle suggests, these matters in three parts:
- Trauma
- Resilience
- Healing
Trauma can take many forms; sometimes it is a very obvious dramatic traumatic event; sometimes less so. Sometimes it can be a mountain of small things that eroded our strength leaving us broken. But what then, of resilience?
Resilience (in psychology, anyway) is not imperviousness; it is the ability to suffer and recover from things.
Healing is the tail-end part of that. When we have undergone trauma, displayed whatever amount of resilience we could at the time, and now have outgrown our coping strategies and looking to genuinely heal.
The authors present many personal stories and case studies to illustrate different kinds of trauma and resilience, and then go on to outline what we can do to grow from there.
Bottom line: if you or a loved one has suffered trauma, this book may help a lot in understanding and processing that, and finding a way forwards from it.
Click here to check out “What Happened To You?” and give yourself what you deserve.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: