Thinking about trying physiotherapy for endometriosis pain? Here’s what to expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Endometriosis is a condition that affects women and girls. It occurs when tissue similar to the lining of the uterus ends up in other areas of the body. These areas include the ovaries, bladder, bowel and digestive tract.
Endometriosis will affect nearly one million Australian women and girls in their lifetime. Many high-profile Australians are affected by endometriosis including Bindi Irwin, Sophie Monk and former Yellow Wiggle, Emma Watkins.
Symptoms of endometriosis include intense pelvic, abdominal or low back pain (that is often worse during menstruation), bladder and bowel problems, pain during sex and infertility.
But women and girls wait an average of seven years to receive a diagnosis. Many are living with the burden of endometriosis and not receiving treatments that could improve their quality of life. This includes physiotherapy.

How is endometriosis treated?
No treatments cure endometriosis. Symptoms can be reduced by taking medications such as non-steriodal anti-inflammatories (ibuprofen, aspirin or naproxen) and hormonal medicines.
Surgery is sometimes used to diagnose endometriosis, remove endometrial lesions, reduce pain and improve fertility. But these lesions can grow back.
Whether they take medication or have surgery, many women and girls continue to experience pain and other symptoms.
Pelvic health physiotherapy is often recommended as a non-drug management technique to manage endometriosis pain, in consultation with a gynaecologist or general practitioner.
The goal of physiotherapy treatment depends on the symptoms but is usually to reduce and manage pain, improve ability to do activities, and ultimately improve quality of life.
What could you expect from your first appointment?
Physiotherapy management can differ based on the severity and location of symptoms. Prior to physical tests and treatments, your physiotherapist will comprehensively explain what is going to happen and seek your permission.
They will ask questions to better understand your case and specific needs. These will include your age, weight, height as well as the presence, location and intensity of symptoms.
You will also be asked about the history of your period pain, your first period, the length of your menstrual cycle, urinary and bowel symptoms, sexual function and details of any previous treatments and tests.
They may also assess your posture and movement to see how your muscles have changed because of the related symptoms.

They will press on your lower back and pelvic muscles to spot painful areas (trigger points) and muscle tightness.
If you consent to a vaginal examination, the physiotherapist will use one to two gloved fingers to assess the area inside and around your vagina. They will also test your ability to coordinate, contract and relax your pelvic muscles.
What type of treatments could you receive?
Depending on your symptoms, your physiotherapist may use the following treatments:
General education
Your physiotherapist will give your details about the disease, pelvic floor anatomy, the types of treatment and how these can improve pain and other symptoms. They might teach you about the changes to the brain and nerves as a result of being in long-term pain.
They will provide guidance to improve your ability to perform daily activities, including getting quality sleep.
If you experience pain during sex or difficulty using tampons, they may teach you how to use vaginal dilators to improve flexibility of those muscles.
Pelvic muscle exercises
Pelvic muscles often contract too hard as a result of pain. Pelvic floor exercises will help you contract and relax muscles appropriately and provide an awareness of how hard muscles are contracting.
This can be combined with machines that monitor muscle activity or vaginal pressure to provide detailed information on how the muscles are working.
Yoga, stretching and low-impact exercises
Yoga, stretching and low impact aerobic exercise can improve fitness, flexibility, pain and blood circulation. These have general pain-relieving properties and can be a great way to contract and relax bigger muscles affected by long-term endometriosis.
These exercises can help you regain function and control with a gradual progression to perform daily activities with reduced pain.

Hydrotherapy (physiotherapy in warm water)
Performing exercises in water improves blood circulation and muscle relaxation due to the pressure and warmth of the water. Hydrotherapy allows you to perform aerobic exercise with low impact, which will reduce pain while exercising.
However, while hydrotherapy shows positive results clinically, scientific studies to show its effectiveness studies are ongoing.
Manual therapy
Women frequently have small areas of muscle that are tight and painful (trigger points) inside and outside the vagina. Pain can be temporarily reduced by pressing, massaging or putting heat on the muscles.
Physiotherapists can teach patients how to do these techniques by themselves at home.
What does the evidence say?
Overall, patients report positive experiences pelvic health physiotherapists treatments. In a study of 42 women, 80% of those who received manual therapy had “much improved pain”.
In studies investigating yoga, one study showed pain was reduced in 28 patients by an average of 30 points on a 100-point pain scale. Another study showed yoga was beneficial for pain in all 15 patients.
But while some studies show this treatment is effective, a review concluded more studies were needed and the use of physiotherapy was “underestimated and underpublicised”.
What else do you need to know?
If you have or suspect you have endometriosis, consult your gynaecologist or GP. They may be able to suggest a pelvic health physiotherapist to help you manage your symptoms and improve quality of life.
As endometriosis is a chronic condition you may be entitled to five subsidised or free sessions per calendar year in clinics that accept Medicare.
If you go to a private pelvic health physiotherapist, you won’t need a referral from a gynaecologist or GP. Physiotherapy rebates can be available to those with private health insurance.
The Australian Physiotherapy Association has a Find a Physio section where you can search for women’s and pelvic physiotherapists. Endometriosis Australia also provides assistance and advice to women with Endometriosis.
Thanks to UTS Masters students Phoebe Walker and Kasey Collins, who are researching physiotherapy treatments for endometriosis, for their contribution to this article.
Peter Stubbs, Senior Lecturer in Physiotherapy, University of Technology Sydney and Caroline Wanderley Souto Ferreira, Visiting Professor of Physiotherapy, University of Technology Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Alzheimer’s Gene That Varies By Race & Sex
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Alzheimer’s Gene That Varies By Race & Sex
You probably know that there are important genetic factors that increase or decrease Alzheimer’s Risk. If you’d like a quick refresher before we carry on, here are two previous articles on this topic:
- Genetic Testing: Health Benefits & Methods (about personal genomics and health, including Alzheimer’s)
- The Surprising Link Between Type 2 Diabetes & Alzheimer’s (about the APOE-ε4 allele that is implicated in both)
A Tale of Two Alleles
It has generally been understood that APOE-ε2 lowers Alzheimer’s disease risk, and APOE-ε4 increases it.
However, for reasons beyond the scope of this article, research populations for genetic testing are overwhelmingly white. If you, dear reader, are white, you may be thinking “well, I’m white, so this isn’t a problem for me”, you might still want to read on…
An extensive new study, published days ago, by Dr. Belloy et al., looked at how these correlations held out per race and sex. They found:
- The “APOE-ε2 lowers; APOE-ε4 increases” dictum held out strongest for white people.
- In the case of Hispanic people, there was only a small correlation on the APOE-ε4 side of things, and none on the APOE-ε2 side of things per se.
- East Asians also saw no correlation with regard to APOE-ε2 per se.
- But! Hispanic and East Asian people had a reduced risk of Alzheimer’s if and only if they had both APOE-ε2 and APOE-ε4.
- Black people, meanwhile, saw a slight correlation with regard to the protective effect of APOE-ε2, and as for APOE-ε4, if they had any European ancestry, increased European ancestry meant a higher increased risk factor if they had APOE-ε4. African ancestry, on the other hand, had a protective effect, proportional to the overall amount of that ancestry.
And as for sex…
- Specifically for white people with the APOE-ε3/ε4 genotype, especially in the age range of 60–70, the genetic risk for Alzheimer’s was highest in women.
If you’d like to read more and examine the data for yourself:
APOE Genotype and Alzheimer Disease Risk Across Age, Sex, and Population Ancestry
Want to reduce your Alzheimer’s risk?
We have just the thing for you:
How To Reduce Your Alzheimer’s Risk: It’s Never Too Early To Do These 11 Things
Take care!
Share This Post
-
Laugh Often, To Laugh Longest!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Putting The Abs Into Absurdity
We’ve talked before about the health benefits of a broadly positive outlook on life:
Optimism Seriously Increases Longevity!
…and we’re very serious about it, but that’s about optimistic life views in general, and today we’re about not just keeping good humor in questionable circumstances, but actively finding good humor in the those moments—even when the moments in question might not be generally described as good!
After all, laughter really can be the best medicine, for example:
From the roots
First a quick recap on de-toothing the psychological aspect of threats, no matter how menacing they may be:
Hello, Emotions: Time For Radical Acceptance!
…which we can then take a step further:
What’s The Worst That Could Happen?
Choose your frame
Do you remember when that hacker hacked and publicized the US Federal no-fly list, after already hacking a nationwide cloud-based security camera company, getting access to more than 150,000 companies’ and private individuals’ security cameras, amongst various other cyber crimes, mostly various kinds of fraud and data theft?
Imagine how she (age 21) must have felt, when being indicted. What do you suppose this hacker had to say for itself under such circumstances?
❝congress is investigating now 🙂
but i stay silly :3 ❞
…the latter half of which, usually rendered “but I stay silly” or “but we stay silly” has since entered popular Gen-Z parlance, usually after expressing some negative thing, often in a state of powerlessness.
Which is an important life skill if powerlessness is something that is often likely.
It’s important for many Gen-Zs with negligible life prospects economically; it’s equally important for 60-somethings getting cancer diagnoses (statistically the most likely decade to find out one has cancer, by the way), and many other kinds of people younger, older, and in between.
Because at the end of the day, we all start powerless and we all end powerless.
Learned helplessness (two kinds)
In psychology, “learned helplessness” occurs when a person or creature gives up after learning that all and any attempts to resist a Bad Thing™ fail, perhaps even badly. A lab rat may just shut down and sit there getting electroshocked, for example. A person subjected to abuse may stop trying to improve their situation, and just go with the path of least resistance.
But, there’s another kind, wherein someone in a position of absolute powerlessness not only makes their peace with that, but also, decides that the one thing the outside world can’t control, is how they take it. Like the hacker we mentioned earlier.
Sometimes the gallows humor is even more literal, laughing at one’s own impending death. Not as a matter of bravado, but genuinely seeing the funny side.
But how?
Unfortunately, fortunately
The trick here is to “find a silver lining” that is nowhere near enough to compensate for the bad thing—and it may even be worse! But that’s fine:
“Unfortunately, I didn’t have time to do the dishes before leaving for my vacation. Fortunately, I also forgot to turn the oven off, so the house burning down covered up my messy kitchen”
Writer’s personal less drastic example: today I set my espresso machine to press me an espresso; it doesn’t have an auto-off and I got distracted and it overflowed everywhere; my immediate reaction was “Oh! I have been blessed with an abundance of coffee!”
This kind of silly little thing, on a daily basis, builds a very solid habit for life that allows one to see the funny side in even the most absurd situations, even matters of life and death (can confirm: been there enough times personally—so far so good, still alive to find the remembered absurdity silly).
The point is not to genuinely value the “silver lining”, because half the time it isn’t even one, really, and it is useless to pretend, in seriousness.
But to pretend in silliness? Now we’re onto something, and the real benefit is in the laughs we had along the way.
Because those worst moments? Are probably when we need it the most, so it’s good to get some practice in!
Want more ways to find the funny and make it a life habit?
We reviewed a good book recently:
The Humor Habit: Rewire Your Brain To Stress Less, Laugh More, And Achieve More’er – by Paul Osincup
Stay silly!
Share This Post
-
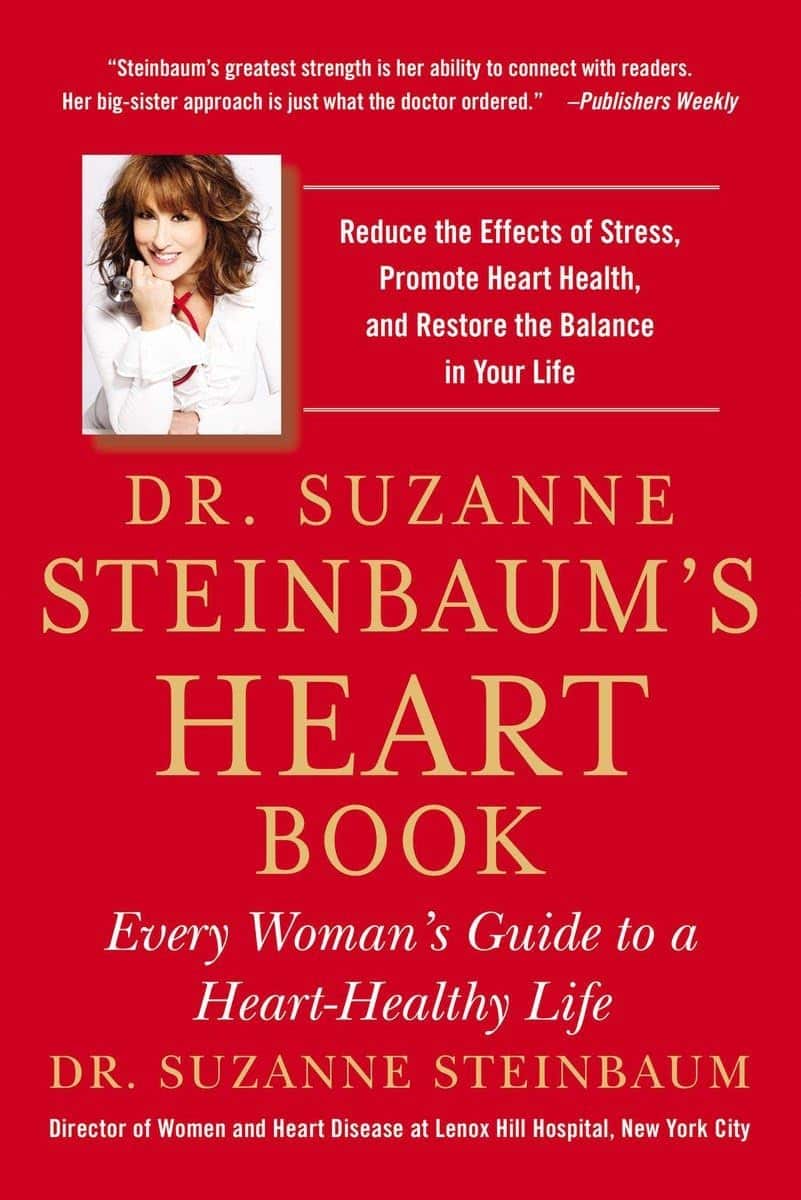
Dr. Suzanne Steinbaum’s Heart Book – by Dr. Suzanne Steinbaum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book is divided into three parts:
- What you should know
- What you should do
- All about you
This is a very useful format, since it lays out all the foundational knowledge, before offering practical advice and “how to” explanations, before finally wrapping up with personalizing things.
The latter is important, because while our basic risk factors can be assembled in a few lines of data (age, sex, race, genes, diet, exercise habits, etc) there’s a lot more to us than that, and oftentimes the data that doesn’t make the cut, makes the difference. Hormones on high on this list; we can say that a person is a 65-year-old woman and make a guess, but that’s all it is: a guess. Very few of us are the “average person” that statistical models represent accurately. And nor are social and psychological factors irrelevant; in fact often they are deciding factors!
So, it’s important to be able to look at ourselves as the whole persons we are, or else we’ll get a heart-healthy protocol that works on paper but actually falls flat in application, because the mathematical model didn’t take into account that lately we have been very stressed about such-and-such a thing, and deeply anxious about so-and-so, and a hopefully short-term respiratory infection has reduced blood oxygen levels, and all these kinds of things need to be taken into account too, for an overall plan to work.
The greatest strength of this book is that it attends to that.
The style of the book is a little like a long sales pitch (when all that’s being sold, by the way, is the ideas the book is offering; she wants you to take her advice with enthusiasm), but there’s plenty of very good information all the way through, making it quite worth the read.
Bottom line: if you’re a woman and/or love at least one woman, then you can benefit from this important book for understanding heart health that’s not the default.
Click here to check out Dr. Suzanne Steinbaum’s Heart Book, and enjoy a heart-healthy life!
Share This Post
Related Posts
-
Heart Attack: His & Hers (Be Prepared!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Heart attack symptoms vary by sex. This is governed by hormones, so if you are for example a postmenopausal woman and not on HRT, your symptoms might be nearer that of men.
The following symptom list is intended as a rough “most likely” guide. You may not get all of the symptoms you “should”. You could get symptoms from the “wrong” category. So don’t sweat the minutiae, but do be aware of…
Symptoms for everyone:
- Jaw, neck, and/or back pain
- Nausea and/or vomiting
- Shortness of breath
- Feeling of impending doom ← heart attack survivors assure us that you’ll know this one if you experience it
Additional symptoms (mostly) just for men:
- Pressure and/or pain in the upper chest
- Discomfort and/or tingling in the arms
- Sudden cold sweat
Additional symptoms (mostly) just for women:
- Pressure and/or pain in the lower chest and/or abdomen
- Feeling of fullness and/or indigestion
- Fatigue, dizziness, possibly fainting
In the event of experiencing symptoms…
Call 911 or your local equivalent.This is not the time to wait to see if it goes away by itself. If unsure, call. Better safe than sorry/dead.
If you are not alone, or if it is someone with you who is having the suspected heart attack, it may be quicker to go to the Emergency Room by car, than wait for an ambulance.
Even if you choose to do that, you should still call 911 anyway, as the responder will be able to instruct you in real-time, not something we can do in a newsletter.
Note that if available, this means three people in the car is ideal:
Driver, patient, and third person on the phone giving information and following instructions.
Emergency situations rarely go entirely by-the-book, but with a little foreknowledge and at least one person with a calm head, preventable deaths can be avoided.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
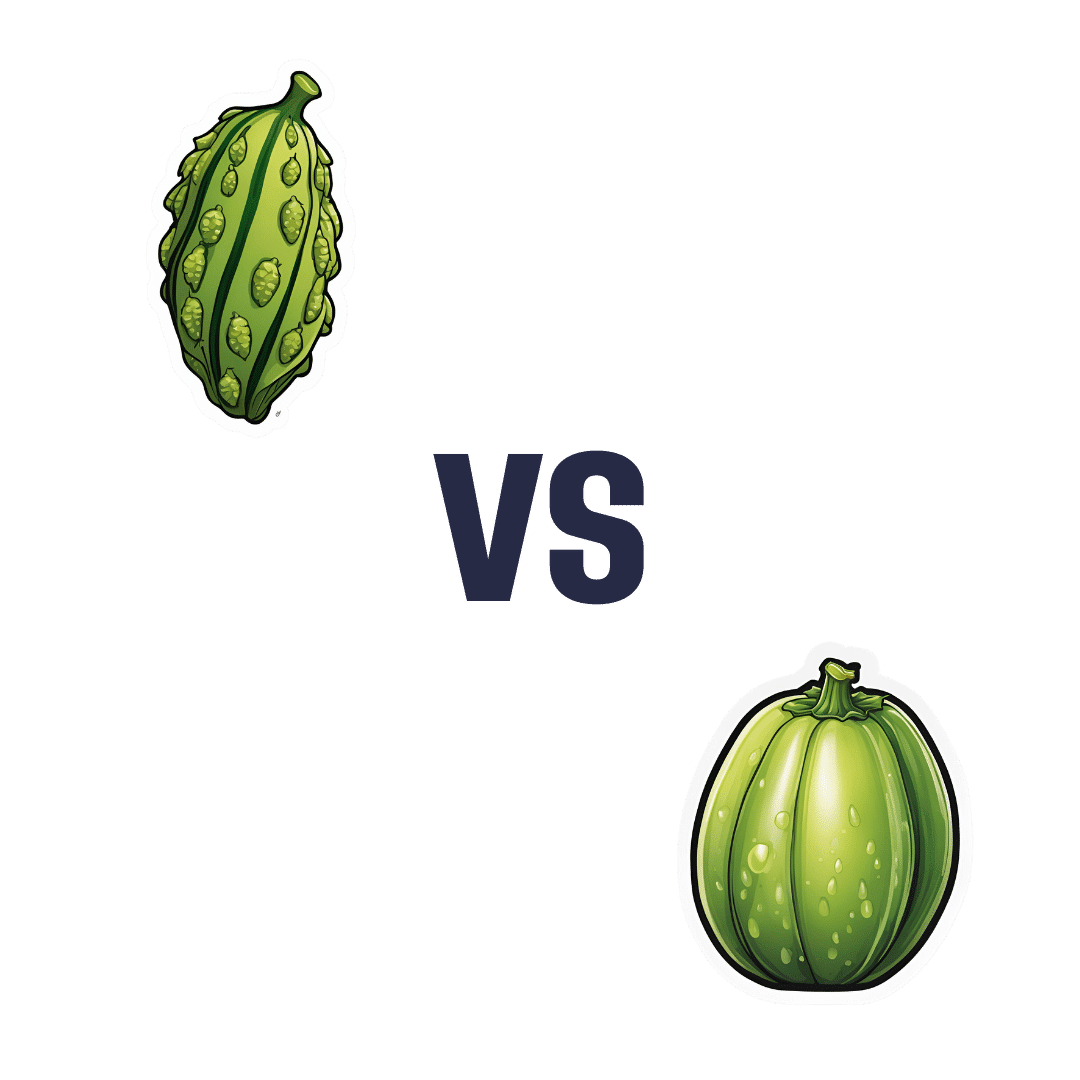
Bitter Melon vs Winter Melon – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing bitter melon to winter melon, we picked the bitter.
Why?
Did you remember the “bitter is better” dictum that goes for most plant-based foods? It certainly stands in this case!
A note on nomenclature before we begin: these two fruits are also known as the bitter gourd and the wax gourd, respectively (amongst many other names for each), but we went with what seems to be their most common names.
In terms of macros, the bitter melon has more than 13x the protein (and actually adding up to a meaningful amount, at 5.3g/100g), as well as more fiber for the same carbs, making it the better choice all around.
When it comes to vitamins, the bitter melon has a lot more of vitamins A, B1, B2, B3, B6, B7, B9, and C, while the winter melon boasts only more vitamin B5. As in, the vitamin that’s in all foods (even its scientific name means “from everywhere”) and in which it’s pretty much impossible to be deficient unless literally starving. All in all, an easy and clear win for bitter melon.
In the category of minerals, we see a similar story: the bitter melon has very much more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while the winter melon has a modest double-dose of zinc—hardly comparable to, say, bitter melon having over 100x the potassium content, and indeed, in all minerals except zinc, bitter melon had 4x–100x more. Another clear and overwhelming win for the bitter melon.
Looking up polyphenols, we see that the bitter melon also wins in that regard, shocking nobody, with an impressive polyphenolic profile, especially rich in luteolins and catechins of various kinds.
In short, enjoy either or both, but there’s a clear winner here, and it’s the bitter melon.
Want to learn more?
You might like to read:
Enjoy Bitter Foods For Your Heart & Brain
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is a ‘vaginal birth after caesarean’ or VBAC?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A vaginal birth after caesarean (known as a VBAC) is when a woman who has had a caesarean has a vaginal birth down the track.
In Australia, about 12% of women have a vaginal birth for a subsequent baby after a caesarean. A VBAC is much more common in some other countries, including in several Scandinavian ones, where 45-55% of women have one.
So what’s involved? What are the risks? And who’s most likely to give birth vaginally the next time round?
MVelishchuk/Shutterstock What happens? What are the risks?
When a woman chooses a VBAC she is cared for much like she would during a planned vaginal birth.
However, an induction of labour is avoided as much as possible, due to the slightly increased risk of the caesarean scar opening up (known as uterine rupture). This is because the medication used in inductions can stimulate strong contractions that put a greater strain on the scar.
In fact, one of the main reasons women may be recommended to have a repeat caesarean over a vaginal birth is due to an increased chance of her caesarean scar rupturing.
This is when layers of the uterus (womb) separate and an emergency caesarean is needed to deliver the baby and repair the uterus.
Uterine rupture is rare. It occurs in about 0.2-0.7% of women with a history of a previous caesarean. A uterine rupture can also happen without a previous caesarean, but this is even rarer.
However, uterine rupture is a medical emergency. A large European study found 13% of babies died after a uterine rupture and 10% of women needed to have their uterus removed.
The risk of uterine rupture increases if women have what’s known as complicated or classical caesarean scars, and for women who have had more than two previous caesareans.
Most care providers recommend you avoid getting pregnant again for around 12 months after a caesarean, to allow full healing of the scar and to reduce the risk of the scar rupturing.
National guidelines recommend women attempt a VBAC in hospital in case emergency care is needed after uterine rupture.
During a VBAC, recommendations are for closer monitoring of the baby’s heart rate and vigilance for abnormal pain that could indicate a rupture is happening.
If labour is not progressing, a caesarean would then usually be advised.
Giving birth in hospital is recommended for a vaginal birth after a caesarean. christinarosepix/Shutterstock Why avoid multiple caesareans?
There are also risks with repeat caesareans. These include slower recovery, increased risks of the placenta growing abnormally in subsequent pregnancies (placenta accreta), or low in front of the cervix (placenta praevia), and being readmitted to hospital for infection.
Women reported birth trauma and post-traumatic stress more commonly after a caesarean than a vaginal birth, especially if the caesarean was not planned.
Women who had a traumatic caesarean or disrespectful care in their previous birth may choose a VBAC to prevent re-traumatisation and to try to regain control over their birth.
We looked at what happened to women
The most common reason for a caesarean section in Australia is a repeat caesarean. Our new research looked at what this means for VBAC.
We analysed data about 172,000 low-risk women who gave birth for the first time in New South Wales between 2001 and 2016.
We found women who had an initial spontaneous vaginal birth had a 91.3% chance of having subsequent vaginal births. However, if they had a caesarean, their probability of having a VBAC was 4.6% after an elective caesarean and 9% after an emergency one.
We also confirmed what national data and previous studies have shown – there are lower VBAC rates (meaning higher rates of repeat caesareans) in private hospitals compared to public hospitals.
We found the probability of subsequent elective caesarean births was higher in private hospitals (84.9%) compared to public hospitals (76.9%).
Our study did not specifically address why this might be the case. However, we know that in private hospitals women access private obstetric care and experience higher caesarean rates overall.
What increases the chance of success?
When women plan a VBAC there is a 60-80% chance of having a vaginal birth in the next birth.
The success rates are higher for women who are younger, have a lower body mass index, have had a previous vaginal birth, give birth in a home-like environment or with midwife-led care.
For instance, an Australian study found women who accessed continuity of care with a midwife were more likely to have a successful VBAC compared to having no continuity of care and seeing different care providers each time.
An Australian national survey we conducted found having continuity of care with a midwife when planning a VBAC can increase women’s sense of control and confidence, increase their chance to be upright and active in labour and result in a better relationship with their health-care provider.
Seeing the same midwife throughout your maternity care can help. Tyler Olson/Shutterstock Why is this important?
With the rise of caesareans globally, including in Australia, it is more important than ever to value vaginal birth and support women to have a VBAC if this is what they choose.
Our research is also a reminder that how a woman gives birth the first time greatly influences how she gives birth after that. For too many women, this can lead to multiple caesareans, not all of them needed.
Hannah Dahlen, Professor of Midwifery, Associate Dean Research and HDR, Midwifery Discipline Leader, Western Sydney University; Hazel Keedle, Senior Lecturer of Midwifery, Western Sydney University, and Lilian Peters, Adjunct Research Fellow, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: