Traveling To Die: The Latest Form of Medical Tourism
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the 18 months after Francine Milano was diagnosed with a recurrence of the ovarian cancer she thought she’d beaten 20 years ago, she traveled twice from her home in Pennsylvania to Vermont. She went not to ski, hike, or leaf-peep, but to arrange to die.
“I really wanted to take control over how I left this world,” said the 61-year-old who lives in Lancaster. “I decided that this was an option for me.”
Dying with medical assistance wasn’t an option when Milano learned in early 2023 that her disease was incurable. At that point, she would have had to travel to Switzerland — or live in the District of Columbia or one of the 10 states where medical aid in dying was legal.
But Vermont lifted its residency requirement in May 2023, followed by Oregon two months later. (Montana effectively allows aid in dying through a 2009 court decision, but that ruling doesn’t spell out rules around residency. And though New York and California recently considered legislation that would allow out-of-staters to secure aid in dying, neither provision passed.)
Despite the limited options and the challenges — such as finding doctors in a new state, figuring out where to die, and traveling when too sick to walk to the next room, let alone climb into a car — dozens have made the trek to the two states that have opened their doors to terminally ill nonresidents seeking aid in dying.
At least 26 people have traveled to Vermont to die, representing nearly 25% of the reported assisted deaths in the state from May 2023 through this June, according to the Vermont Department of Health. In Oregon, 23 out-of-state residents died using medical assistance in 2023, just over 6% of the state total, according to the Oregon Health Authority.
Oncologist Charles Blanke, whose clinic in Portland is devoted to end-of-life care, said he thinks that Oregon’s total is likely an undercount and he expects the numbers to grow. Over the past year, he said, he’s seen two to four out-of-state patients a week — about one-quarter of his practice — and fielded calls from across the U.S., including New York, the Carolinas, Florida, and “tons from Texas.” But just because patients are willing to travel doesn’t mean it’s easy or that they get their desired outcome.
“The law is pretty strict about what has to be done,” Blanke said.
As in other states that allow what some call physician-assisted death or assisted suicide, Oregon and Vermont require patients to be assessed by two doctors. Patients must have less than six months to live, be mentally and cognitively sound, and be physically able to ingest the drugs to end their lives. Charts and records must be reviewed in the state; neglecting to do so constitutes practicing medicine out of state, which violates medical licensing requirements. For the same reason, the patients must be in the state for the initial exam, when they request the drugs, and when they ingest them.
State legislatures impose those restrictions as safeguards — to balance the rights of patients seeking aid in dying with a legislative imperative not to pass laws that are harmful to anyone, said Peg Sandeen, CEO of the group Death With Dignity. Like many aid-in-dying advocates, however, she said such rules create undue burdens for people who are already suffering.
Diana Barnard, a Vermont palliative care physician, said some patients cannot even come for their appointments. “They end up being sick or not feeling like traveling, so there’s rescheduling involved,” she said. “It’s asking people to use a significant part of their energy to come here when they really deserve to have the option closer to home.”
Those opposed to aid in dying include religious groups that say taking a life is immoral, and medical practitioners who argue their job is to make people more comfortable at the end of life, not to end the life itself.
Anthropologist Anita Hannig, who interviewed dozens of terminally ill patients while researching her 2022 book, “The Day I Die: The Untold Story of Assisted Dying in America,” said she doesn’t expect federal legislation to settle the issue anytime soon. As the Supreme Court did with abortion in 2022, it ruled assisted dying to be a states’ rights issue in 1997.
During the 2023-24 legislative sessions, 19 states (including Milano’s home state of Pennsylvania) considered aid-in-dying legislation, according to the advocacy group Compassion & Choices. Delaware was the sole state to pass it, but the governor has yet to act on it.
Sandeen said that many states initially pass restrictive laws — requiring 21-day wait times and psychiatric evaluations, for instance — only to eventually repeal provisions that prove unduly onerous. That makes her optimistic that more states will eventually follow Vermont and Oregon, she said.
Milano would have preferred to travel to neighboring New Jersey, where aid in dying has been legal since 2019, but its residency requirement made that a nonstarter. And though Oregon has more providers than the largely rural state of Vermont, Milano opted for the nine-hour car ride to Burlington because it was less physically and financially draining than a cross-country trip.
The logistics were key because Milano knew she’d have to return. When she traveled to Vermont in May 2023 with her husband and her brother, she wasn’t near death. She figured that the next time she was in Vermont, it would be to request the medication. Then she’d have to wait 15 days to receive it.
The waiting period is standard to ensure that a person has what Barnard calls “thoughtful time to contemplate the decision,” although she said most have done that long before. Some states have shortened the period or, like Oregon, have a waiver option.
That waiting period can be hard on patients, on top of being away from their health care team, home, and family. Blanke said he has seen as many as 25 relatives attend the death of an Oregon resident, but out-of-staters usually bring only one person. And while finding a place to die can be a problem for Oregonians who are in care homes or hospitals that prohibit aid in dying, it’s especially challenging for nonresidents.
When Oregon lifted its residency requirement, Blanke advertised on Craigslist and used the results to compile a list of short-term accommodations, including Airbnbs, willing to allow patients to die there. Nonprofits in states with aid-in-dying laws also maintain such lists, Sandeen said.
Milano hasn’t gotten to the point where she needs to find a place to take the meds and end her life. In fact, because she had a relatively healthy year after her first trip to Vermont, she let her six-month approval period lapse.
In June, though, she headed back to open another six-month window. This time, she went with a girlfriend who has a camper van. They drove six hours to cross the state border, stopping at a playground and gift shop before sitting in a parking lot where Milano had a Zoom appointment with her doctors rather than driving three more hours to Burlington to meet in person.
“I don’t know if they do GPS tracking or IP address kind of stuff, but I would have been afraid not to be honest,” she said.
That’s not all that scares her. She worries she’ll be too sick to return to Vermont when she is ready to die. And, even if she can get there, she wonders whether she’ll have the courage to take the medication. About one-third of people approved for assisted death don’t follow through, Blanke said. For them, it’s often enough to know they have the meds — the control — to end their lives when they want.
Milano said she is grateful she has that power now while she’s still healthy enough to travel and enjoy life. “I just wish more people had the option,” she said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is ADHD Being Over-Diagnosed For Cash?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is ADHD Being Systematically Overdiagnosed?
The BBC’s investigative “Panorama” program all so recently did a documentary in which one of their journalists—who does not have ADHD—went to three private clinics and got an ADHD diagnosis from each of them:
- The BBC documentary: Private ADHD Clinics Exposed (28 mins)
- Their “5 Minutes” version: ADHD Undercover: How I Was Misdiagnosed (6 mins)
So… Is it really a case of show up, pay up, and get a shiny new diagnosis?
The BBC Panorama producers cherry-picked 3 private providers, and during those clinical assessments, their journalist provided answers that would certainly lead to a diagnosis.
This was contrasted against a three-hour assessment with an NHS psychiatrist—something that rarely happens in the NHS. Which prompts the question…
How did he walk into a 3-hour psychiatrist assessment, when most people have to wait in long waiting lists for a much more cursory appointment first with assorted gatekeepers, before going on another long waiting list, for an also-much-shorter appointment with a psychiatrist?
That would be because the NHS psychiatrist was given advance notification that this was part of an investigation and would be filmed (the private clinics were not gifted the same transparency)
So, maybe just a tad unequal treatment!
In case you’re wondering, here’s what that very NHS psychiatrist had to say on the topic:
Is it really too easy to be diagnosed with ADHD?
(we’ll give you a hint—remember Betteridge’s Law!)
❝Since the documentary aired, I have heard from people concerned that GPs could now be more likely to question legitimate diagnoses.
But as an NHS psychiatrist it is clear to me that the root of this issue is not overdiagnosis.
Instead, we are facing the combined challenges of remedying decades of underdiagnosis and NHS services that were set up when there was little awareness of ADHD.❞
~ Dr. Mike Smith, Psychiatrist
The ADHD foundation, meanwhile, has issued its own response, saying:
❝We are disappointed that BBC Panorama has opted to broadcast a poorly researched, sensationalist piece of television journalism.❞
Share This Post
-
Cannabis & Heart Attacks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For many, cannabis use has taken the place that alcohol used to have when it comes to wanting a “downer”, that is to say, a drug that relaxes us as opposed to stimulating us.
Indeed, it is generally considered safer than alcohol ← however this is not a strong claim, because alcohol is much more dangerous than one would think given its ubiquity and (in many places, at least) social acceptability.
We’ve talked a bit about cannabis use before, in its various forms, for example:
Cannabis Myths vs Reality ← a very good starting point for the curious
And one specifically about the use of THC gummies (THC is the psychoactive compound in cannabis, i.e. it’s the chemical that gets people high, as opposed to CBD, which is not psychoactive) as a sleep aid:
Sweet Dreams Are Made of THC (Or Are They?)
And for those skipping the THC, we’ve also written about CBD use, including:
CBD Oil: What Does The Science Say? and Do CBD Gummies Work?
So, about cannabis and heart attacks
Alcohol is a relaxant, and yet it can contribute to heart disease (amongst many other things, of course):
Can We Drink To Good Health? ← this is mostly about red wine’s putative heart health benefits, how the idea got popularized, and how it doesn’t stand up to scrutiny when actually looking at the evidence.
And cannabis, another relaxant? Not so good either!
New research has shown that cannabis users have a higher risk of heart attacks, even among younger and otherwise healthy individuals. This is based on analyzing data from 4,636,628 relatively healthy adults.
Specifically, the data showed that even young healthy cannabis users get:
- Sixfold increased risk of heart attack
- Fourfold increased risk of ischemic stroke
- Threefold increased risk of cardiovascular death, heart attack, or stroke
We mention the otherwise “relatively healthy” nature of the participants, because it’s important to note that less healthy people (who were perhaps using cannabis to self-medicate for some serious condition) were not included in the dataset, as it’d skew the data unhelpfully and it’d make the risk look a lot higher than the risk levels we mentioned above.
The mechanisms by which cannabis affects heart health are not fully understood, but hypotheses include:
- Disrupting heart rhythm regulation
- Increasing oxygen demand in the heart muscle
- Causing endothelial dysfunction, which affects blood vessel function
Further, heart attack risk peaked one hour after cannabis use, and while this doesn’t prove causality, it certainly doesn’t make cannabis look safe.
You can read the paper in its entirety here:
Want a safer way to relax?
We recommend:
- No-Frills, Evidence-Based Mindfulness
- Meditation Games That You’ll Actually Enjoy
- Which Style Of Yoga Is Best For You?
- 7 Kinds Of Rest When Sleep Is Not Enough
- Better Sex = Longer Life (Here’s How)
Enjoy!
Share This Post
-
10 Simple Japanese Habits For Healthier & Longer Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You don’t have to be Japanese or live in Okinawa to enjoy the benefits of healthy longevity. A lot of it comes down to simple habits:
Easy to implement
We’ll not keep the 10 habits a mystery; they are:
- Start the day with hot water: drinking hot water in the morning helps with hydration, warming the body, and aiding digestion.
- Enjoy a hearty breakfast: Japanese breakfasts are traditionally filling, nutritious, and help promote energy and longevity. Typical components include rice, miso soup, fish, and pickles.
- Take balanced meals: Japanese education emphasizes nutrition from a young age, promoting balanced meals with proteins, fiber, and vitamins & minerals.
- Enjoy fermented foods: fermented foods, such as nattō and soy-based condiments, support digestion, heart health, and the immune system.
- Drink green tea and matcha: both are rich in health benefits; preparing matcha mindfully adds a peaceful ritual to daily life too.
- Keep the “80% full” rule: “hara hachi bu” encourages eating until 80% full, which can improve longevity and, of course, prevent overeating.
- Use multiple small dishes: small servings and a variety of dishes help prevent overeating and ensure a diverse intake of nutrients.
- Gratitude before and after meals: saying “itadakimasu” and “gochisousama” promotes mindful eating, and afterwards, good digestion. Speaking Japanese is of course not the key factor here, but rather, do give yourself a moment of reflection before and after meals.
- Use vinegar in cooking: vinegar, often used in sushi rice and sauces like ponzu, adds flavor and offers health benefits, mostly pertaining to blood sugar balance.
- Eat slowly: Eating at a slower pace will improve digestion, and can enhance satiety and prevent accidentally overeating.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Get More Out Of What’s On Your Plate
Take care!
Share This Post
Related Posts
-
Ouch. That ‘Free’ Annual Checkup Might Cost You. Here’s Why.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kristy Uddin, 49, went in for her annual mammogram in Washington state last year, she assumed she would not incur a bill because the test is one of the many preventive measures guaranteed to be free to patients under the 2010 Affordable Care Act. The ACA’s provision made medical and economic sense, encouraging Americans to use screening tools that could nip medical problems in the bud and keep patients healthy.
So when a bill for $236 arrived, Uddin — an occupational therapist familiar with the health care industry’s workings — complained to her insurer and the hospital. She even requested an independent review.
“I’m like, ‘Tell me why am I getting this bill?’” Uddin recalled in an interview. The unsatisfying explanation: The mammogram itself was covered, per the ACA’s rules, but the fee for the equipment and the facility was not.
That answer was particularly galling, she said, because, a year earlier, her “free” mammogram at the same health system had generated a bill of about $1,000 for the radiologist’s reading. Though she fought that charge (and won), this time she threw in the towel and wrote the $236 check. But then she dashed off a submission to the KFF Health News-NPR “Bill of the Month” project:
“I was really mad — it’s ridiculous,” she later recalled. “This is not how the law is supposed to work.”
The ACA’s designers might have assumed that they had spelled out with sufficient clarity that millions of Americans would no longer have to pay for certain types of preventive care, including mammograms, colonoscopies, and recommended vaccines, in addition to doctor visits to screen for disease. But the law’s authors didn’t reckon with America’s ever-creative medical billing juggernaut.
Over the past several years, the medical industry has eroded the ACA’s guarantees, finding ways to bill patients in gray zones of the law. Patients going in for preventive care, expecting that it will be fully covered by insurance, are being blindsided by bills, big and small.
The problem comes down to deciding exactly what components of a medical encounter are covered by the ACA guarantee. For example, when do conversations between doctor and patient during an annual visit for preventive services veer into the treatment sphere? What screenings are needed for a patient’s annual visit?
A healthy 30-year-old visiting a primary care provider might get a few basic blood tests, while a 50-year-old who is overweight would merit additional screening for Type 2 diabetes.
Making matters more confusing, the annual checkup itself is guaranteed to be “no cost” for women and people age 65 and older, but the guarantee doesn’t apply for men in the 18-64 age range — though many preventive services that require a medical visit (such as checks of blood pressure or cholesterol and screens for substance abuse) are covered.
No wonder what’s covered under the umbrella of prevention can look very different to medical providers (trying to be thorough) and billers (intent on squeezing more dollars out of every medical encounter) than it does to insurers (who profit from narrower definitions).
For patients, the gray zone has become a billing minefield. Here are a few more examples, gleaned from the Bill of the Month project in just the past six months:
Peter Opaskar, 46, of Texas, went to his primary care doctor last year for his preventive care visit — as he’d done before, at no cost. This time, his insurer paid $130.81 for the visit, but he also received a perplexing bill for $111.81. Opaskar learned that he had incurred the additional charge because when his doctor asked if he had any health concerns, he mentioned that he was having digestive problems but had already made an appointment with his gastroenterologist. So, the office explained, his visit was billed as both a preventive physical and a consultation. “Next year,” Opasker said in an interview, if he’s asked about health concerns, “I’ll say ‘no,’ even if I have a gunshot wound.”
Kevin Lin, a technology specialist in Virginia in his 30s, went to a new primary care provider to take advantage of the preventive care benefit when he got insurance; he had no physical complaints. He said he was assured at check-in that he wouldn’t be charged. His insurer paid $174 for the checkup, but he was billed an additional $132.29 for a “new patient visit.” He said he has made many calls to fight the bill, so far with no luck.
Finally, there’s Yoori Lee, 46, of Minnesota, herself a colorectal surgeon, who was shocked when her first screening colonoscopy yielded a bill for $450 for a biopsy of a polyp — a bill she knew was illegal. Federal regulations issued in 2022 to clarify the matter are very clear that biopsies during screening colonoscopies are included in the no-cost promise. “I mean, the whole point of screening is to find things,” she said, stating, perhaps, the obvious.
Though these patient bills defy common sense, room for creative exploitation has been provided by the complex regulatory language surrounding the ACA. Consider this from Ellen Montz, deputy administrator and director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare & Medicaid Services, in an emailed response to queries and an interview request on this subject: “If a preventive service is not billed separately or is not tracked as individual encounter data separately from an office visit and the primary purpose of the office visit is not the delivery of the preventive item or service, then the plan issuer may impose cost sharing for the office visit.”
So, if the doctor decides that a patient’s mention of stomach pain does not fall under the umbrella of preventive care, then that aspect of the visit can be billed separately, and the patient must pay?
And then there’s this, also from Montz: “Whether a facility fee is permitted to be charged to a consumer would depend on whether the facility usage is an integral part of performing the mammogram or an integral part of any other preventive service that is required to be covered without cost sharing under federal law.”
But wait, how can you do a mammogram or colonoscopy without a facility?
Unfortunately, there is no federal enforcement mechanism to catch individual billing abuses. And agencies’ remedies are weak — simply directing insurers to reprocess claims or notifying patients they can resubmit them.
In the absence of stronger enforcement or remedies, CMS could likely curtail these practices and give patients the tools to fight back by offering the sort of clarity the agency provided a few years ago regarding polyp biopsies — spelling out more clearly what comes under the rubric of preventive care, what can be billed, and what cannot.
The stories KFF Health News and NPR receive are likely just the tip of an iceberg. And while each bill might be relatively small compared with the stunning $10,000 hospital bills that have become all too familiar in the United States, the sorry consequences are manifold. Patients pay bills they do not owe, depriving them of cash they could use elsewhere. If they can’t pay, those bills might end up with debt-collection agencies and, ultimately, harm their credit score.
Perhaps most disturbing: These unexpected bills might discourage people from seeking preventive screenings that could be lifesaving, which is why the ACA deemed them “essential health benefits” that should be free.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oral vaccines could provide relief for people who suffer regular UTIs. Here’s how they work
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a recent TikTok video, Australian media personality Abbie Chatfield shared she was starting a vaccine to protect against urinary tract infections (UTIs).
Huge news for the UTI girlies. I am starting a UTI vaccine tonight for the first time.
Chatfield suffers from recurrent UTIs and has turned to the Uromune vaccine, an emerging option for those seeking relief beyond antibiotics.
But Uromune is not a traditional vaccine injected to your arm. So what is it and how does it work?
9nong/Shutterstock First, what are UTIs?
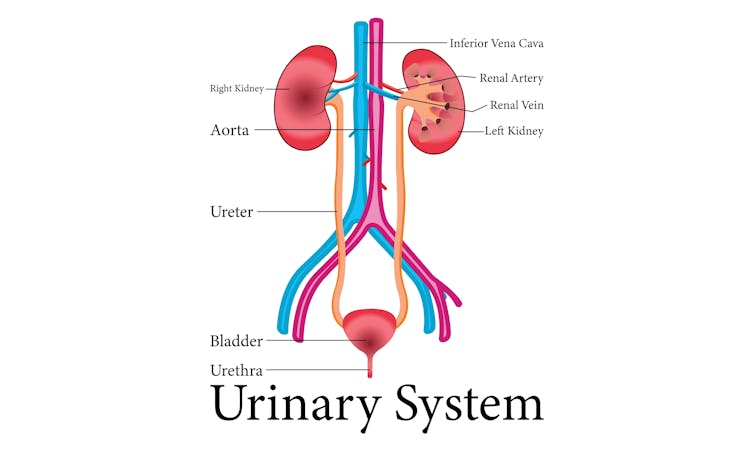
UTIs are caused by bacteria entering the urinary system. This system includes the kidneys, bladder, ureters (thin tubes connecting the kidneys to the bladder), and the urethra (the tube through which urine leaves the body).
The most common culprit is Escherichia coli (E. coli), a type of bacteria normally found in the intestines.
While most types of E. coli are harmless in the gut, it can cause infection if it enters the urinary tract. UTIs are particularly prevalent in women due to their shorter urethras, which make it easier for bacteria to reach the bladder.
Roughly 50% of women will experience at least one UTI in their lifetime, and up to half of those will have a recurrence within six months.
UTIs are caused by bacteria enterning the urinary system. oxo7051/Shutterstock The symptoms of a UTI typically include a burning sensation when you wee, frequent urges to go even when the bladder is empty, cloudy or strong-smelling urine, and pain or discomfort in the lower abdomen or back. If left untreated, a UTI can escalate into a kidney infection, which can require more intensive treatment.
While antibiotics are the go-to treatment for UTIs, the rise of antibiotic resistance and the fact many people experience frequent reinfections has sparked more interest in preventive options, including vaccines.
What is Uromune?
Uromune is a bit different to traditional vaccines that are injected into the muscle. It’s a sublingual spray, which means you spray it under your tongue. Uromune is generally used daily for three months.
It contains inactivated forms of four bacteria that are responsible for most UTIs, including E. coli. By introducing these bacteria in a controlled way, it helps your immune system learn to recognise and fight them off before they cause an infection. It can be classified as an immunotherapy.
A recent study involving 1,104 women found the Uromune vaccine was 91.7% effective at reducing recurrent UTIs after three months, with effectiveness dropping to 57.6% after 12 months.
These results suggest Uromune could provide significant (though time-limited) relief for women dealing with frequent UTIs, however peer-reviewed research remains limited.
Any side effects of Uromune are usually mild and may include dry mouth, slight stomach discomfort, and nausea. These side effects typically go away on their own and very few people stop treatment because of them. In rare cases, some people may experience an allergic reaction.
How can I access it?
In Australia, Uromune has not received full approval from the Therapeutic Goods Administration (TGA), and so it’s not something you can just go and pick up from the pharmacy.
However, Uromune can be accessed via the TGA’s Special Access Scheme or the Authorised Prescriber pathway. This means a GP or specialist can apply for approval to prescribe Uromune for patients with recurrent UTIs. Once the patient has a form from their doctor documenting this approval, they can order the vaccine directly from the manufacturer.
Antibiotics are the go-to treatment for UTIs – but scientists are looking at options to prevent them in the first place. Photoroyalty/Shutterstock Uromune is not covered under the Pharmaceutical Benefits Scheme, meaning patients must cover the full cost out-of-pocket. The cost of a treatment program is around A$320.
Uromune is similarly available through special access programs in places like the United Kingdom and Europe.
Other options in the pipeline
In addition to Uromune, scientists are exploring other promising UTI vaccines.
Uro-Vaxom is an established immunomodulator, a substance that helps regulate or modify the immune system’s response to bacteria. It’s derived from E. coli proteins and has shown success in reducing UTI recurrences in several studies. Uro-Vaxom is typically prescribed as a daily oral capsule taken for 90 days.
FimCH, another vaccine in development, targets something called the adhesin protein that helps E. coli attach to urinary tract cells. FimCH is typically administered through an injection and early clinical trials have shown promising results.
Meanwhile, StroVac, which is already approved in Germany, contains inactivated strains of bacteria such as E. coli and provides protection for up to 12 months, requiring a booster dose after that. This injection works by stimulating the immune system in the bladder, offering temporary protection against recurrent infections.
These vaccines show promise, but challenges like achieving long-term immunity remain. Research is ongoing to improve these options.
No magic bullet, but there’s reason for optimism
While vaccines such as Uromune may not be an accessible or perfect solution for everyone, they offer real hope for people tired of recurring UTIs and endless rounds of antibiotics.
Although the road to long-term relief might still be a bit bumpy, it’s exciting to see innovative treatments like these giving people more options to take control of their health.
Iris Lim, Assistant Professor in Biomedical Science, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Liver Cure – by Dr. Russell Blaylock
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about How To Unfatty A Fatty Liver, but there’s a lot more that can be said in a book that we couldn’t fit into our article.
In this book, Dr. Blaylock looks at the causes and symptoms of liver disease, the mechanisms behind such, and how we can adjust our dietary habits (and other things) to do better for ourselves.
While the book’s primary focus is on diet, he does also look at medications (especially: those that hinder liver health, which are many, including simple/common stuff like Tylenol and similar), and the effects of different lifestyle choices, including ones that aren’t diet-related.
Because most people’s knowledge of liver disease starts and ends at “don’t drink yourself to death”, this book is an important tome of knowledge for actually keeping this critical organ in good order—especially since symptoms of liver disease can initially be subtle, and slow to show, often escaping notice until it’s already far, far worse than it could have been.
Many people find out by experiencing liver failure.
The writing style is… A little repetitive for this reviewer’s preference, but it does make sure that you won’t miss things. Also, when it comes to supplements, he repeatedly recommends a particular company, and it’s not clear whether he has a financial interest there. But the actual medical information is good and important and comprehensive.
Bottom line: if you’d like to keep your liver in good health, this is a book that will help you to do just that.
Click here to check out The Liver Cure, and keep yours working well!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: