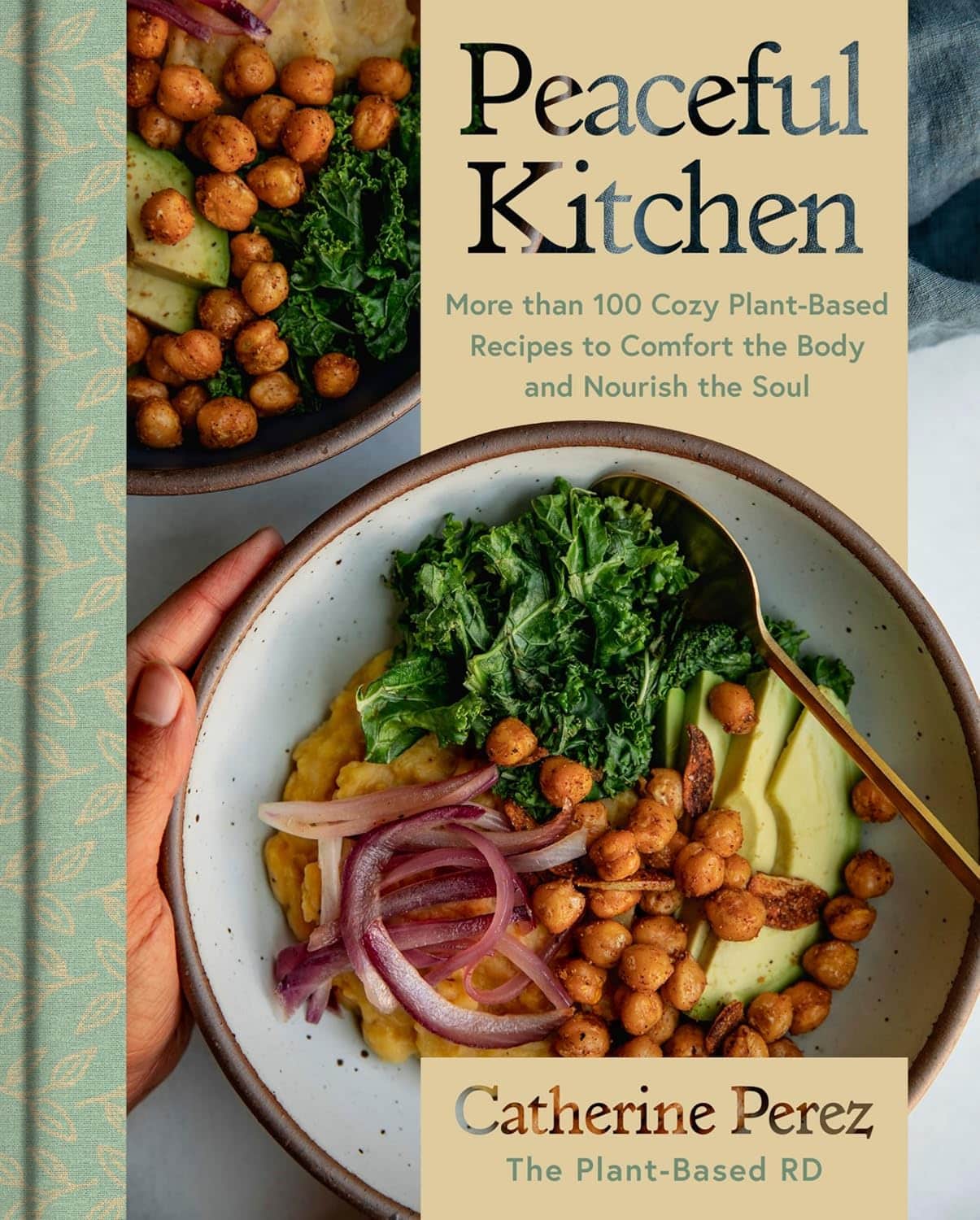
Peaceful Kitchen – by Catherine Perez
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a keen cook and Registered Dietician with a Master’s in same, covers the basics of the science of nutrition as relevant to her recipes, but first and foremost this is not a science textbook—it’s a cookbook, and its pages contain more love for the art than citations for the (perfectly respectable) science.
Mexican and Dominican cuisine are the main influences in this book, but there are dishes from around the world too.
The recipes themselves are… Comparable in difficulty to the things we often feature in our recipes section here at 10almonds. They’re probably not winning any restaurants Michelin stars, but they’re not exactly student survival recipes either. They’re made from mostly non-obscure whole foods, nutritionally-dense ingredients at that, with minimal processed foods involved.
That said, she does take a “add, don’t subtract” approach to nutrition, i.e. focussing more on adding in diversity of plants than on “don’t eat this; don’t eat that” mandates.
If there’s any criticism to be levelled at the book, it’s that in most cases we’d multiply the spices severalfold, but that’s not a big problem as readers can always judge that individually; she’s given the basic information of which spices in which proportions, which is the key knowledge.
Bottom line: if you’re looking to expand your plant-based cooking repertoire, this one is a fine choice.
Click here to check out Peaceful Kitchen, and try some new things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s Your Personal Life Expectancy?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tick Tock… Goes the Death Clock?
This fun little test will ask a few questions about you and your lifestyle, and then make a prediction of your personal life expectancy, based on global statistics from the World Health Organisation.
And then the countdown starts… Literally, it generates a clock for you to see your life-seconds ticking away—this may or may not delight you, but it sure is a curiosity.
Their “Letters” page has a lot of reactions from people who just got their results (spoiler: people’s perspectives on life vary a lot)
Who mostly uses this service? According to their stats page, it’s mostly curious under-45s, with gradually less interest in knowing about it from 45 onwards… until the age of 70, when suddenly everyone wants to know about it again!
So Is It Possible To Pause The Clock On Aging? – Q&A Spotlight Interview
Life extension is sometimes viewed as the domain of the super-rich, and with less than half of Millennials (and almost none of Gen-Z) having retirement plans, often those of us who aren’t super-rich have more mundane (and immediate!) goals than living to 120.
And yet…
Middle class and working class life-extensionists do exist, even if not garnering the same media attention. We think that’s strange—after all, while the whimsies of the super-rich may be entertaining to read about, it’s not nearly as applicable to most people as more relatable stories:
- The twenty-something who gives up smoking and adds (healthier!) years to their life
- The thirty-something who adopts a plant-based diet and is less likely to die of heart disease
- The forty-something who stops drinking, and avoids health conditions and mishaps alike
- The fifty-something who reconsiders their health plan in light of their changing body
- The sixty-something who takes up yoga, or chess, or salsa dancing
- The seventy-something who gets asked what their secret is
- …and so on
But these are ideas, textbook examples. What if we make it more personal?
We interviewed 10 Almonds subscriber and longevity enthusiast Anastasia S., and here’s what she had to say:
Q: What does life extension mean to you, in your life?
A: To me, the key is healthy life extension. People often joke “I don’t want to live longer; the last years are the worst!” but they’re missing the point that after a certain age, those difficulties are coming whether they come at 50 or 70 or 90. Personally, I’d rather keep them at bay if I can.
Q: How do you do that?
A: Firstly, which won’t be a shock: good diet and exercise. Those two things are possibly the biggest active influences on my longevity. I’m vegan, which I don’t think is outright necessary for good health but done right, it can certainly be good. In this house we eat a lot of whole grains, beans, lentils, vegetables in general, nuts too. As for exercise, I do 30–60 minutes of Pilates daily; it’s nothing fancy and it’s just me in my pajamas at home, but it keeps me strong and fit and supple. I also walk everywhere; I don’t even own a car. Beyond that… I don’t drink or smoke (probably the biggest passive influences on my longevity, i.e., things that aren’t there to make it shorter), and I try to take my sleep seriously, making sure to schedule enough time and prepare properly for it.
Q: Take your sleep seriously? How so?
A: Good “sleep hygiene” as some call it—I schedule a little wind-down time before sleep, with no glaring screens or main lights, making a space between my busy day and restful sleep, kicking anything requiring brainpower to the morning, and making a conscious choice not to think more about those things in the meantime. I take care to make my sleeping environment as conducive as possible to good sleep too; I have a good mattress and pillows, I make sure the temperature is cool but cosy. I have a pot of herbal tea on my bedside table—I hydrate a lot.
Q: Do you take any supplements?
A: I do! They’re mostly quite general though, just “covering my bases”, so to speak. I take a daily nootropic stack (a collection of supplements specifically for brain health), too. I buy them in bulk, so they don’t cost so much.
Q: This seems quite a healthy lifestyle! Do you have any vices at all?
A: I definitely drink more coffee than I probably should! But hey, nobody’s perfect. I do love coffee, though, and as vices go, it’s probably not too bad.
Q: How’s it all working out for you? Do you feel younger?
A: I’m 38 and sometimes I feel like a teenager; sometimes I feel like an old lady. But the latter is usually for social reasons, not health-related reasons. I do have streaks of gray in my hair though, and I love that! If people don’t notice my grays, then they often think I’m in my 20s, rather than pushing 40. A little while back, I was stopped in the street by someone wanting to sell me a change of household utilities provider, then she stopped herself mid-sentence and said “Oh but wait, you look a bit too young, never mind”. Most general metrics of health would put me in my 20s.
Q: That’s interesting that you love your gray hairs, for someone who wants to stay young; is it an exception?
A: It’s more that I want to minimize the problems that come with age, and not everything’s a problem. Gray hairs are cool; joint pain, not so much. A long life rich with experiences is cool; memory loss, not so much. So, I try to keep healthy, and wear my years as best I can.
Q: Sounds good to us; good luck with it!
A: Thank you; I do my best!
Here at 10 Almonds, we love featuring what our readers are doing to improve their health; if you’re willing to be featured in our newsletter, let us know by replying to this email (where an actual human will read it, we promise!)
Share This Post
-
Why Lung Cancer Is On The Rise In Women Who’ve Never Smoked
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to assume that if you’ve never smoked, lung cancer is just not a risk for you, unless you got very unlucky with an asbestos-laden environment or such.
And yes, smoking is indeed the most overwhelmingly strong risk factor:
❝It is estimated that cigarette smoking explains almost 90% of lung cancer risk in men and 70 to 80% in women❞
Which is a lot (and we’ll address that discrepancy by sex shortly), but meanwhile first let’s mention:
❝Compared with non-smokers, smokers have as much as a 30-fold increased risk of developing cancer.
31% and 26% of all cancer deaths in men and women, respectively, result from lung cancer in the United States.
Overall 5-year survival is only 15%, and 1-year survival is approximately 42%.
In total, lung cancer is responsible for more deaths than prostate, colon, pancreas, and breast cancers combined❞
Source: Smoking and Lung Cancer
Sobering statistics for any smoker, certainly.
But, “smoking is bad for the health” is not the breaking news of the century, so we’ll look now at the other risk factors.
Before we do though, let’s just drop this previous main feature of ours for anyone who does smoke or perhaps who has a loved one who smokes:
Which Addiction-Quitting Methods Work Best? ← it’s not specific just to smoking, but it does cover such also
So, Why the extra risk for women, even if we don’t smoke?
Let’s reframe that first statistic we gave, now presenting the same information differently:
Women who do not smoke are 2–3x more likely to get lung cancer than men who do not smoke.
So… why?
There are three main reasons:
Genetic risks
Cancer often arises from genetic mutations. In the case of lung cancer, genes such as ALK, ROS1, TP53, KRAS, and EGFR are implicated, and some of those are much more likely to mutate in women than in men.
In some cases, it’s because if you have XX chromosomes (as most women do), there are genes you have redundant copies of that people with XY chromosomes don’t. Other less common karyotypes, such as XXY, probably carry higher risks, but that’s just a hypothesis we’re making based on “more copies of a gene = more chances for it to mutate”.
See also: Frequency and Distinctive Spectrum of KRAS Mutations in Never Smokers with Lung Adenocarcinoma
In other cases, it’s because estrogen interacts with the gene mutations, making lung cancer more likely to develop in women over time:
Hormonal risks (but not what you might think)
When something affects women more, it’s easy to blame hormones, but, as researchers have concluded…
❝A reduced lung cancer risk was found for OC and HRT ever users. Both oestrogen only and oestrogen+progestin HRT were associated with decreased risk. No dose-response relationship was observed with years of OC/HRT use. The greatest risk reduction was seen for squamous cell carcinoma in OC users and in both adenocarcinoma and small cell carcinoma in HRT users.❞
OC = oral contraceptive
HRT = hormone replacement therapyNote: we snipped out the statistical calculations for readability and brevity, so if you are interested in those, check out the paper below:
Meanwhile, another research review of 22 studies with nearly a million participants found:
❝Current or ever HRT use is partly correlated with the decreased incidence of lung cancer in women.
Concerns about the incidence of lung cancer can be reduced when perimenopausal and postmenopausal women use current HRT to reduce menopausal symptoms.❞
So, the problem seems to at least a lot of the time be not estrogen (notwithstanding what we mentioned previously about mutations—sometimes a thing can have both pros and cons), but rather, untreated menopause being the higher risk factor.
This is very reminiscent of what we talked about in one of our main features about Alzheimer’s disease:
Alzheimer’s Sex Differences May Not Be What They Appear ← Women get Alzheimer’s at nearly 2x the rate than men do, and deteriorate more rapidly after onset, too.
Chronic inflammation
For reasons that have not been tied to genetics or hormones*, women suffer from autoimmune diseases at much higher rates than men.
*presumably it is at least one or the other, because there aren’t a lot of other options that seem plausible, but (as with many “this thing mainly affects women” maladies), science hasn’t yet determined the cause.
Because cancer is in part a disease of immune dysfunction (cells fail to kill cells they should be killing), having an autoimmune disease, or indeed chronic inflammation in general, will result in a higher risk of cancer.
For general theory, see: Cancer and Autoimmune Diseases: A Tale of Two Immunological Opposites?
For specifics, see: Non–Small Cell Lung Cancer: Role of the Immune System and Potential for Immunotherapy
And this one is the most likely explanation of why lung cancer in women who’ve never smoked is on the rise—it’s because chronic inflammation in women is on the rise. While people regardless of gender are getting chronic inflammation at increased rates nowadays (probably due in large part to the rise of ultra-processed food, as well as the higher stress of modern life, but again, we’re hypothesizing), if all other factors are equal, women will still get it more than men.
However!
Like the consideration of HRT’s protective effects (and unlike the genetic factors), this is one we can do something about.
For how, check out: How to Prevent (or Reduce) Inflammation
Want to know more?
For lung health in general, see:
Seven Things To Do For Good Lung Health!
Take care!
Share This Post
-
If You’re Poor, Fertility Treatment Can Be Out of Reach
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mary Delgado’s first pregnancy went according to plan, but when she tried to get pregnant again seven years later, nothing happened. After 10 months, Delgado, now 34, and her partner, Joaquin Rodriguez, went to see an OB-GYN. Tests showed she had endometriosis, which was interfering with conception. Delgado’s only option, the doctor said, was in vitro fertilization.
“When she told me that, she broke me inside,” Delgado said, “because I knew it was so expensive.”
Delgado, who lives in New York City, is enrolled in Medicaid, the federal-state health program for low-income and disabled people. The roughly $20,000 price tag for a round of IVF would be a financial stretch for lots of people, but for someone on Medicaid — for which the maximum annual income for a two-person household in New York is just over $26,000 — the treatment can be unattainable.
Expansions of work-based insurance plans to cover fertility treatments, including free egg freezing and unlimited IVF cycles, are often touted by large companies as a boon for their employees. But people with lower incomes, often minorities, are more likely to be covered by Medicaid or skimpier commercial plans with no such coverage. That raises the question of whether medical assistance to create a family is only for the well-to-do or people with generous benefit packages.
“In American health care, they don’t want the poor people to reproduce,” Delgado said. She was caring full-time for their son, who was born with a rare genetic disorder that required several surgeries before he was 5. Her partner, who works for a company that maintains the city’s yellow cabs, has an individual plan through the state insurance marketplace, but it does not include fertility coverage.
Some medical experts whose patients have faced these issues say they can understand why people in Delgado’s situation think the system is stacked against them.
“It feels a little like that,” said Elizabeth Ginsburg, a professor of obstetrics and gynecology at Harvard Medical School who is president-elect of the American Society for Reproductive Medicine, a research and advocacy group.
Whether or not it’s intended, many say the inequity reflects poorly on the U.S.
“This is really sort of standing out as a sore thumb in a nation that would like to claim that it cares for the less fortunate and it seeks to do anything it can for them,” said Eli Adashi, a professor of medical science at Brown University and former president of the Society for Reproductive Endocrinologists.
Yet efforts to add coverage for fertility care to Medicaid face a lot of pushback, Ginsburg said.
Over the years, Barbara Collura, president and CEO of the advocacy group Resolve: The National Infertility Association, has heard many explanations for why it doesn’t make sense to cover fertility treatment for Medicaid recipients. Legislators have asked, “If they can’t pay for fertility treatment, do they have any idea how much it costs to raise a child?” she said.
“So right there, as a country we’re making judgments about who gets to have children,” Collura said.
The legacy of the eugenics movement of the early 20th century, when states passed laws that permitted poor, nonwhite, and disabled people to be sterilized against their will, lingers as well.
“As a reproductive justice person, I believe it’s a human right to have a child, and it’s a larger ethical issue to provide support,” said Regina Davis Moss, president and CEO of In Our Own Voice: National Black Women’s Reproductive Justice Agenda, an advocacy group.
But such coverage decisions — especially when the health care safety net is involved — sometimes require difficult choices, because resources are limited.
Even if state Medicaid programs wanted to cover fertility treatment, for instance, they would have to weigh the benefit against investing in other types of care, including maternity care, said Kate McEvoy, executive director of the National Association of Medicaid Directors. “There is a recognition about the primacy and urgency of maternity care,” she said.
Medicaid pays for about 40% of births in the United States. And since 2022, 46 states and the District of Columbia have elected to extend Medicaid postpartum coverage to 12 months, up from 60 days.
Fertility problems are relatively common, affecting roughly 10% of women and men of childbearing age, according to the National Institute of Child Health and Human Development.
Traditionally, a couple is considered infertile if they’ve been trying to get pregnant unsuccessfully for 12 months. Last year, the ASRM broadened the definition of infertility to incorporate would-be parents beyond heterosexual couples, including people who can’t get pregnant for medical, sexual, or other reasons, as well as those who need medical interventions such as donor eggs or sperm to get pregnant.
The World Health Organization defined infertility as a disease of the reproductive system characterized by failing to get pregnant after a year of unprotected intercourse. It terms the high cost of fertility treatment a major equity issue and has called for better policies and public financing to improve access.
No matter how the condition is defined, private health plans often decline to cover fertility treatments because they don’t consider them “medically necessary.” Twenty states and Washington, D.C., have laws requiring health plans to provide some fertility coverage, but those laws vary greatly and apply only to companies whose plans are regulated by the state.
In recent years, many companies have begun offering fertility treatment in a bid to recruit and retain top-notch talent. In 2023, 45% of companies with 500 or more workers covered IVF and/or drug therapy, according to the benefits consultant Mercer.
But that doesn’t help people on Medicaid. Only two states’ Medicaid programs provide any fertility treatment: New York covers some oral ovulation-enhancing medications, and Illinois covers costs for fertility preservation, to freeze the eggs or sperm of people who need medical treatment that will likely make them infertile, such as for cancer. Several other states also are considering adding fertility preservation services.
In Delgado’s case, Medicaid covered the tests to diagnose her endometriosis, but nothing more. She was searching the internet for fertility treatment options when she came upon a clinic group called CNY Fertility that seemed significantly less expensive than other clinics, and also offered in-house financing. Based in Syracuse, New York, the company has a handful of clinics in upstate New York cities and four other U.S. locations.
Though Delgado and her partner had to travel more than 300 miles round trip to Albany for the procedures, the savings made it worthwhile. They were able do an entire IVF cycle, including medications, egg retrieval, genetic testing, and transferring the egg to her uterus, for $14,000. To pay for it, they took $7,000 of the cash they’d been saving to buy a home and financed the other half through the fertility clinic.
She got pregnant on the first try, and their daughter, Emiliana, is now almost a year old.
Delgado doesn’t resent people with more resources or better insurance coverage, but she wishes the system were more equitable.
“I have a medical problem,” she said. “It’s not like I did IVF because I wanted to choose the gender.”
One reason CNY is less expensive than other clinics is simply that the privately owned company chooses to charge less, said William Kiltz, its vice president of marketing and business development. Since the company’s beginning in 1997, it has become a large practice with a large volume of IVF cycles, which helps keep prices low.
At this point, more than half its clients come from out of state, and many earn significantly less than a typical patient at another clinic. Twenty percent earn less than $50,000, and “we treat a good number who are on Medicaid,” Kiltz said.
Now that their son, Joaquin, is settled in a good school, Delgado has started working for an agency that provides home health services. After putting in 30 hours a week for 90 days, she’ll be eligible for health insurance.
One of the benefits: fertility coverage.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
You can train your nose – and 4 other surprising facts about your sense of smell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Would you give up your sense of smell to keep your hair? What about your phone?
A 2022 US study compared smell to other senses (sight and hearing) and personally prized commodities (including money, a pet or hair) to see what people valued more.
The researchers found smell was viewed as much less important than sight and hearing, and valued less than many commodities. For example, half the women surveyed said they’d choose to keep their hair over sense of smell.
Smell often goes under the radar as one of the least valued senses. But it is one of the first sensory systems vertebrates developed and is linked to your mental health, memory and more.
Here are five fascinating facts about your olfactory system.
DimaBerlin/Shutterstock 1. Smell is linked to memory and emotion
Why can the waft of fresh baking trigger joyful childhood memories? And why might a certain perfume jolt you back to a painful breakup?
Smell is directly linked to both your memory and emotions. This connection was first established by American psychologist Donald Laird in 1935 (although French novelist Marcel Proust had already made it famous in his reverie about the scent of madeleines baking.)
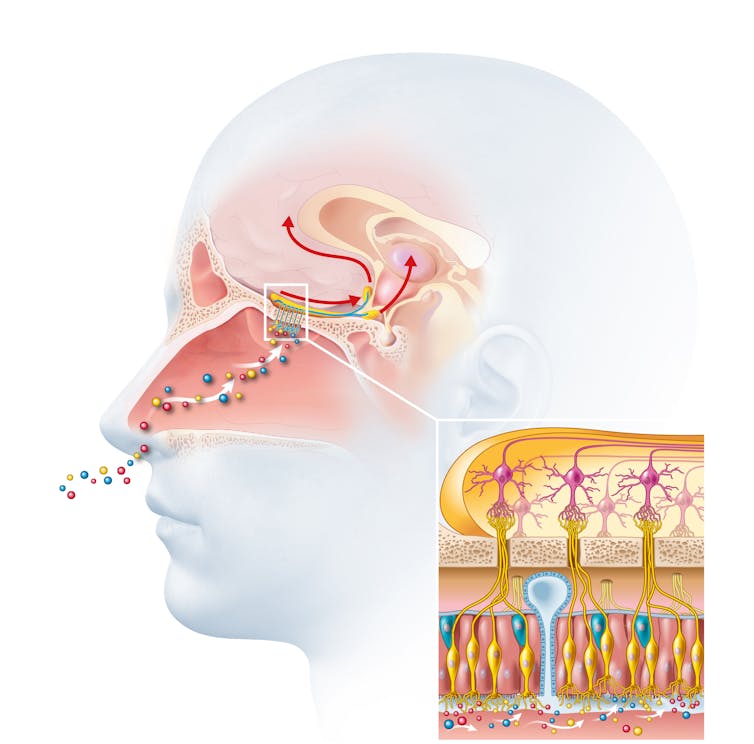
Odours are first captured by special olfactory nerve cells inside your nose. These cells extend upwards from the roof of your nose towards the smell-processing centre of your brain, called the olfactory bulb.
Smells are first detected by nerve cells in the nose. Axel_Kock/Shutterstock From the olfactory bulb they form direct connection with the brain’s limbic system. This includes the amygdala, where emotions are generated, and the hippocampus, where memories are created.
Other senses – such as sight and hearing – aren’t directly connected to the lymbic system.
One 2004 study used functional magnetic resonance imaging to demonstrate odours trigger a much stronger emotional and memory response in the brain than a visual cue.
2. Your sense of smell constantly regenerates
You can lose your ability to smell due to injury or infection – for example during and after a COVID infection. This is known as olfactory dysfunction. In most cases it’s temporary, returning to normal within a few weeks.
This is because every few months your olfactory nerve cells die and are replaced by new cells.
We’re not entirely sure how this occurs, but it likely involves your nose’s stem cells, the olfactory bulb and other cells in the olfactory nerves.
Other areas of your nervous system – including your brain and spinal cord – cannot regenerate and repair after an injury.
Constant regeneration may be a protective mechanism, as the olfactory nerves are vulnerable to damage caused by the external environment, including toxins (such as cigarette smoke), chemicals and pathogens (such as the flu virus).
But following a COVID infection some people might continue to experience a loss of smell. Studies suggest the virus and a long-term immune response damages the cells that allow the olfactory system to regenerate.
3. Smell is linked to mental health
Around 5% of the global population suffer from anosmia – total loss of smell. An estimated 15-20% suffer partial loss, known as hyposmia.
Given smell loss is often a primary and long-term symptom of COVID, these numbers are likely to be higher since the pandemic.
Yet in Australia, the prevalence of olfactory dysfunction remains surprisingly understudied.
Losing your sense of smell is shown to impact your personal and social relationships. For example, it can mean you miss out on shared eating experiences, or cause changes in sexual desire and behaviour.
In older people, declining ability to smell is associated with a higher risk of depression and even death, although we still don’t know why.
Losing your sense of smell can have a major impact on mental health. Halfpoint/Shutterstock 4. Loss of smell can help identify neurodegenerative diseases
Partial or full loss of smell is often an early indicator for a range of neurodegenerative diseases, including Alzheimer’s and Parkinson’s diseases.
Patients frequently report losing their sense of smell years before any symptoms show in body or brain function. However many people are not aware they are losing their sense of smell.
There are ways you can determine if you have smell loss and to what extent. You may be able to visit a formal smell testing centre or do a self-test at home, which assesses your ability to identify household items like coffee, wine or soap.
5. You can train your nose back into smelling
“Smell training” is emerging as a promising experimental treatment option for olfactory dysfunction. For people experiencing smell loss after COVID, it’s been show to improve the ability to detect and differentiate odours.
Smell training (or “olfactory training”) was first tested in 2009 in a German psychology study. It involves sniffing robust odours — such as floral, citrus, aromatic or fruity scents — at least twice a day for 10—20 seconds at a time, usually over a 3—6 month period.
Participants are asked to focus on the memory of the smell while sniffing and recall information about the odour and its intensity. This is believed to help reorganise the nerve connections in the brain, although the exact mechanism behind it is unclear.
Some studies recommend using a single set of scents, while others recommend switching to a new set of odours after a certain amount of time. However both methods show significant improvement in smelling.
This training has also been shown to alleviate depressive symptoms and improve cognitive decline both in older adults and those suffering from dementia.
Just like physiotherapy after a physical injury, olfactory training is thought to act like rehabilitation for your sense of smell. It retrains the nerves in your nose and the connections it forms within the brain, allowing you to correctly detect, process and interpret odours.
Lynn Nazareth, Research Scientist in Olfactory Biology, CSIRO
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Wanna read more?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You’ve Got Questions? We’ve Got Answers!
Q: Tips for reading more and managing time for it?
A: We talked about this a little bit in yesterday’s edition, so you may have seen that, but aside from that:
- If you don’t already have one, consider getting a Kindle or similar e-reader. They’re very convenient, and also very light and ergonomic—no more wrist strain as can occur with physical books. No more eye-strain, either!
- Consider making reading a specific part of your daily routine. A chapter before bed can be a nice wind-down, for instance! What’s important is it’s a part of your day that’ll always, or at least almost always, allow you to do a little reading.
- If you drive, walk, run, or similar each day, a lot of people find that’s a great time to listen to an audiobook. Please be safe, though!
- If your lifestyle permits such, a “reading retreat” can be a wonderful vacation! Even if you only “retreat” to your bedroom, the point is that it’s a weekend (or more!) that you block off from all other commitments, and curl up with the book(s) of your choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oscar contender Poor Things is a film about disability. Why won’t more people say so?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Readers are advised this article includes an offensive and outdated disability term in a quote from the film.
Poor Things is a spectacular film that has garnered critical praise, scooped up awards and has 11 Oscar nominations. That might be the problem. Audiences become absorbed in another world, so much so our usual frames of reference disappear.
There has been much discussion about the film’s feminist potential (or betrayal). What’s not being talked about in mainstream reviews is disability. This seems strange when two of the film’s main characters are disabled.
Set in a fantasy version of Victorian London, unorthodox Dr Godwin Baxter (William Dafoe) finds the just-dead body of a heavily pregnant woman in the Thames River. In keeping with his menagerie of hybrid animals, Godwin removes the unborn baby’s brain and puts it into the skull of its mother, who becomes Bella Baxter (Emma Stone).
Is Bella really disabled?
Stone has been praised for her ability to embody a small child who rapidly matures into a hypersexual person – one who has not had time to absorb the restrictive rules of gender or patriarchy.
But we also see a woman using her behaviour to express herself because she has complex communication barriers. We see a woman who is highly sensitive and responsive to the sensory world around her. A woman moving through and seeing the world differently – just like the fish-eye lens used in many scenes.
Women like this exist and they have historically been confined, studied and monitored like Bella. When medical student Max McCandless (Ramy Youssef) first meets Bella, he offensively exclaims “what a very pretty retard!” before being told the truth and promptly declared her future husband.
Even if Bella is not coded as disabled through her movements, speech and behaviour, her onscreen creator and guardian is. Godwin Baxter has facial differences and other impairments which require assistive technology.
So ignoring disability as a theme of the film seems determined and overt. The absurd humour for which the film is being lauded is often at Bella’s “primitive”, “monstrous” or “damaged” actions: words which aren’t usually used to describe children, but have been used to describe disabled people throughout history.
In reviews, Bella’s walk and speech are compared to characters like the Scarecrow in The Wizard of Oz, rather than a disabled woman. So why the resistance?
Freak shows and displays
Disability studies scholar Rosemarie Gardland-Thomson writes “the history of disabled people in the Western world is in part the history of being on display”.
In the 19th century, when Poor Things is set, “freak shows” featuring disabled people, Indigenous people and others with bodily differences were extremely popular.
Doctors used freak shows to find specimens – like Joseph Merrick (also known as the Elephant Man and later depicted on screen) who was used for entertainment before he was exhibited in lecture halls. In the mid-1800s, as medicine became a profession, observing the disabled body shifted from a public spectacle to a private medical gaze that labelled disability as “sick” and pathologised it.
Poor Things doesn’t just circle around these discourses of disability. Bella’s body is a medical experiment, kept locked away for the private viewing of male doctors who take notes about her every move in small pads. While there is something glorious, intimate and familiar about Bella’s discovery of her own sexual pleasure, she immediately recognises it as worth recording in the third person:
I’ve discovered something that I must share […] Bella discover happy when she want!
The film’s narrative arc ends with Bella herself training to be a doctor but one whose more visible disabilities have disappeared.
Framing charity and sexual abuse
Even the film’s title is an expression often used to describe disabled people. The charity model of disability sees disabled people as needing pity and support from others. Financial poverty is briefly shown at a far-off port in the film and Bella initially becomes a sex worker in Paris for money – but her more pressing concern is sexual pleasure.
Disabled women’s sexuality is usually seen as something that needs to be controlled. It is frequently assumed disabled women are either hypersexual or de-gendered and sexually innocent.
In the real world disabled people experience much higher rates of abuse, including sexual assault, than others. Last year’s Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability found women with disability are nearly twice as likely as women without disability to have been assaulted. Almost a third of women with disability have experienced sexual assault by the age of 15. Bella’s hypersexual curiosity appears to give her some layer of protection – but that portrayal denies the lived experience of many.
Watch but don’t ignore
Poor Things is a stunning film. But ignoring disability in the production ignores the ways in which the representation of disabled bodies play into deep and historical stereotypes about disabled people.
These representations continue to shape lives.
Louisa Smith, Senior lecturer, Deakin University; Gemma Digby, Lecturer – Health & Social Development, Deakin University, and Shane Clifton, Associate Professor of Practice, School of Health Sciences and the Centre for Disability Research and Policy, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: