Breast Milk’s Benefits That Are (So Far) Not Replicable
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Simply The Breast 🎶
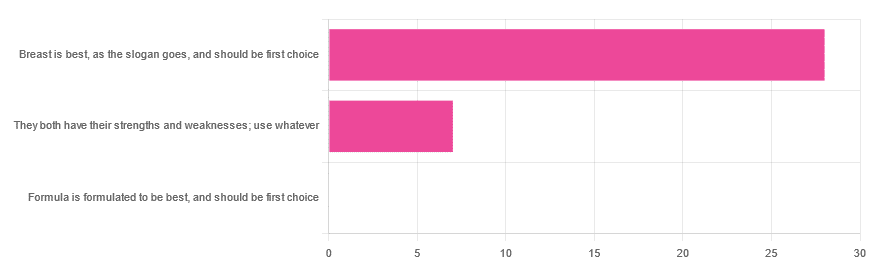
In Wednesday’s newsletter, we asked you for your opinion on breast vs formula milk (for babies!), and got the above-depicted, below-described, set of responses:
- 80% said “Breast is best, as the slogan goes, and should be first choice”
- 20% said “They both have their strengths and weaknesses; use whatever”
- 0% said “Formula is formulated to be best, and should be first choice”
That’s the first time we’ve ever had a possible poll option come back with zero votes whatsoever! It seems this topic is relatively uncontentious amongst our readership, so we’ll keep things brief today, but there is still a little mythbusting to be done.
So, what does the science say?
[Breast milk should be the first choice] at least for the few few weeks and months for the benefit of baby’s health as breast milk has protective factors formula does not: True or False?
True! The wording here was taken from one of our readers’ responses, by the way (thank you, Robin). There are a good number of those protective factors, the most well-known of which is passing on immune cells and cell-like things; in other words, immune-related information being passed from parent* to child.
*usually the mother, though in principle it could be someone else and in practice sometimes it is; the only real requirements are that the other person be healthy, lactating, and willing.
As for immune benefits, see for example:
Perspectives on Immunoglobulins in Colostrum and Milk
And for that matter, also:
(Colostrum is simply the milk that is produced for a short period after giving birth; the composition of milk will tend to change later)
In any case, immunoglobulin A is a very important component in breast milk (colostrum and later), as well as lactoferrin (has an important antimicrobial effect and is good for the newborn’s gut), and a plethora of cytokines:
As for that about the gut, lactoferrin isn’t the only breast milk component that benefits this, by far, and there’s a lot that can’t be replicated yet:
Human Breast Milk and the Gastrointestinal Innate Immune System
As long as your infant/child is nutritiously fed, it shouldn’t matter if it comes from breast or formula: True or False?
False! Formula milk will not convey those immune benefits.
This doesn’t mean that formula-feeding is neglectful; as several people who commented mentioned*, there are many reasons a person may not be able to breastfeed, and they certainly should not be shamed for that.
*(including the reader whose words we borrowed for this True/False item; the words we quoted above were prefaced with: “Not everyone is able to breastfeed for many different reasons”)
But, while formula milk is a very good second choice, and absolutely a respectable choice if breast milk isn’t an option (or an acceptable option) for whatever reason, it still does not convey all the health benefits of breast milk—yet! The day may come when they’ll find a way to replicate the immune benefits, but today is not that day.
They both have their strengths and weaknesses: True or False?
True! But formula’s strengths are only in the category of convenience and sometimes necessity—formula conveys no health benefits that breast milk could not do better, if available.
For many babies, formula means they get to eat, when without it they would starve due to non-availability of breast milk. That’s a pretty important role!
Note also: this is a health science publication, not a philosophical publication, but we’d be remiss not to mention one thing; let’s bring it in under the umbrella of sociology:
The right to bodily autonomy continues to be the right to bodily autonomy even if somebody else wants/needs something from your body.
Therefore, while there are indeed many good reasons for not being able to breastfeed, or even just not being safely* able to breastfeed, it is at the very least this writer’s opinion that nobody should be pressed to give their reason for not breastfeeding; “no” is already a sufficient answer.
*Writer’s example re safety: when I was born, my mother was on such drugs that it would have been a very bad idea for her to breastfeed me. There are plenty of other possible reasons why it might be unsafe for someone one way or another, but “on drugs that have a clear ‘do not take while pregnant or nursing’ warning” is a relatively common one.
All that said, for those who are willing and safely able, the science is clear: breast is best.
Want to read more?
The World Health Organization has a wealth of information (including explanations of its recommendations of, where possible, exclusive breastfeeding for the first 6 months, ideally continuing some breastfeeding for the first 2 years), here:
World Health Organization | Breastfeeding
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
He Fell Ill on a Cruise. Before He Boarded the Rescue Boat, They Handed Him the Bill.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Vincent Wasney and his fiancée, Sarah Eberlein, had never visited the ocean. They’d never even been on a plane. But when they bought their first home in Saginaw, Michigan, in 2018, their real estate agent gifted them tickets for a Royal Caribbean cruise.
After two years of delays due to the coronavirus pandemic, they set sail in December 2022.
The couple chose a cruise destined for the Bahamas in part because it included a trip to CocoCay, a private island accessible to Royal Caribbean passengers that featured a water park, balloon rides, and an excursion swimming with pigs.
It was on that day on CocoCay when Wasney, 31, started feeling off, he said.
The next morning, as the couple made plans in their cabin for the last full day of the trip, Wasney made a pained noise. Eberlein saw him having a seizure in bed, with blood coming out of his mouth from biting his tongue. She opened their door to find help and happened upon another guest, who roused his wife, an emergency room physician.
Wasney was able to climb into a wheelchair brought by the ship’s medical crew to take him down to the medical facility, where he was given anticonvulsants and fluids and monitored before being released.
Wasney had had seizures in the past, starting about 10 years ago, but it had been a while since his last one. Imaging back then showed no tumors, and doctors concluded he was likely epileptic, he said. He took medicine initially, but after two years without another seizure, he said, his doctors took him off the medicine to avoid liver damage.
Wasney had a second seizure on the ship a few hours later, back in his cabin. This time he stopped breathing, and Eberlein remembered his lips being so purple, they almost looked black. Again, she ran to find help but, in her haste, locked herself out. By the time the ship’s medical team got into the cabin, Wasney was breathing again but had broken blood vessels along his chest and neck that he later said resembled tiger stripes.
Wasney was in the ship’s medical center when he had a third seizure — a grand mal, which typically causes a loss of consciousness and violent muscle contractions. By then, the ship was close enough to port that Wasney could be evacuated by rescue boat. He was put on a stretcher to be lowered by ropes off the side of the ship, with Eberlein climbing down a rope ladder to join him.
But before they disembarked, the bill came.
The Patient: Vincent Wasney, 31, who was uninsured at the time.
Medical Services: General and enhanced observation, a blood test, anticonvulsant medicine, and a fee for services performed outside the medical facility.
Service Provider: Independence of the Seas Medical Center, the on-ship medical facility on the cruise ship operated by Royal Caribbean International.
Total Bill: $2,500.22.
What Gives: As part of Royal Caribbean’s guest terms, cruise passengers “agree to pay in full” all expenses incurred on board by the end of the cruise, including those related to medical care. In addition, Royal Caribbean does not accept “land-based” health insurance plans.
Wasney said he was surprised to learn that, along with other charges like wireless internet, Royal Caribbean required he pay his medical bills before exiting the ship — even though he was being evacuated urgently.
“Are we being held hostage at this point?” Eberlein remembered asking. “Because, obviously, if he’s had three seizures in 10 hours, it’s an issue.”
Wasney said he has little memory of being on the ship after his first seizure — seizures often leave victims groggy and disoriented for a few hours afterward.
But he certainly remembers being shown a bill, the bulk of which was the $2,500.22 in medical charges, while waiting for the rescue boat.
Still groggy, Wasney recalled saying he couldn’t afford that and a cruise employee responding: “How much can you pay?”
They drained their bank accounts, including money saved for their next house payment, and maxed out Wasney’s credit card but were still about $1,000 short, he said.
Ultimately, they were allowed to leave the ship. He later learned his card was overdrafted to cover the shortfall, he said.
Royal Caribbean International did not respond to multiple inquiries from KFF Health News.
Once on land, in Florida, Wasney was taken by ambulance to the emergency room at Broward Health Medical Center in Fort Lauderdale, where he incurred thousands of dollars more in medical expenses.
He still isn’t entirely sure what caused the seizures.
On the ship he was told it could have been extreme dehydration — and he said he does remember being extra thirsty on CocoCay. He also has mused whether trying escargot for the first time the night before could have played a role. Eberlein’s mother is convinced the episode was connected to swimming with pigs, he said. And not to be discounted, Eberlein accidentally broke a pocket mirror three days before their trip.
Wasney, who works in a stone shop, was uninsured when they set sail. He said that one month before they embarked on their voyage, he finally felt he could afford the health plan offered through his employer and signed up, but the plan didn’t start until January 2023, after their return.
They also lacked travel insurance. As inexperienced travelers, Wasney said, they thought it was for lost luggage and canceled trips, not unexpected medical expenses. And because the cruise was a gift, they were never prompted to buy coverage, which often happens when tickets are purchased.
The Resolution: Wasney said the couple returned to Saginaw with essentially no money in their bank account, several thousand dollars of medical debt, and no idea how they would cover their mortgage payment. Because he was uninsured at the time of the cruise, Wasney did not try to collect reimbursement for the cruise bill from his new health plan when his coverage began weeks later.
The couple set up payment plans to cover the medical bills for Wasney’s care after leaving the ship: one each with two doctors he saw at Broward Health, who billed separately from the hospital, and one with the ambulance company. He also made payments on a bill with Broward Health itself. Those plans do not charge interest.
But Broward Health said Wasney missed two payments to the hospital, and that bill was ultimately sent to collections.
In a statement, Broward Health spokesperson Nina Levine said Wasney’s bill was reduced by 73% because he was uninsured.
“We do everything in our power to provide the best care with the least financial impact, but also cannot stress enough the importance of taking advantage of private and Affordable Care Act health insurance plans, as well as travel insurance, to lower risks associated with unplanned medical issues,” she said.
The couple was able to make their house payment with $2,690 they raised through a GoFundMe campaign that Wasney set up. Wasney said a lot of that help came from family as well as friends he met playing disc golf, a sport he picked up during the pandemic.
“A bunch of people came through for us,” Wasney said, still moved to tears by the generosity. “But there’s still the hospital bill.”
The Takeaway: Billing practices differ by cruise line, but Joe Scott, chair of the cruise ship medicine section of the American College of Emergency Physicians, said medical charges are typically added to a cruise passenger’s onboard account, which must be paid before leaving the ship. Individuals can then submit receipts to their insurers for possible reimbursement.
More from Bill of the Month
- Sign Here? Financial Agreements May Leave Doctors in the Driver’s Seat Apr 30, 2024
- A Mom’s $97,000 Question: How Was Her Baby’s Air-Ambulance Ride Not Medically Necessary? Mar 25, 2024
- Without Medicare Part B’s Shield, Patient’s Family Owes $81,000 for a Single Air-Ambulance Flight Feb 27, 2024
He recommended that those planning to take a cruise purchase travel insurance that specifically covers their trips. “This will facilitate reimbursement if they do incur charges and potentially cover a costly medical evacuation if needed,” Scott said.
Royal Caribbean suggests that passengers who receive onboard care submit their paid bills to their health insurer for possible reimbursement. Many health plans do not cover medical services received on cruise ships, however. Medicare will sometimes cover medically necessary health care services on cruise ships, but not if the ship is more than six hours away from a U.S. port.
Travel insurance can be designed to address lots of out-of-town mishaps, like lost baggage or even transportation and lodging for a loved one to visit if a traveler is hospitalized.
Travel medical insurance, as well as plans that offer “emergency evacuation and repatriation,” are two types that can specifically assist with medical emergencies. Such plans can be purchased individually. Credit cards may offer travel medical insurance among their benefits, as well.
But travel insurance plans come with limitations. For instance, they may not cover care associated with preexisting conditions or what the plans consider “risky” activities, such as rock climbing. Some plans also require that travelers file first with their primary health insurance before seeking reimbursement from travel insurance.
As with other insurance, be sure to read the fine print and understand how reimbursement works.
Wasney said that’s what they plan to do before their next Royal Caribbean cruise. They’d like to go back to the Bahamas on basically the same trip, he said — there’s a lot about CocoCay they didn’t get to explore.
Bill of the Month is a crowdsourced investigation by KFF Health News and NPR that dissects and explains medical bills. Do you have an interesting medical bill you want to share with us? Tell us about it!
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
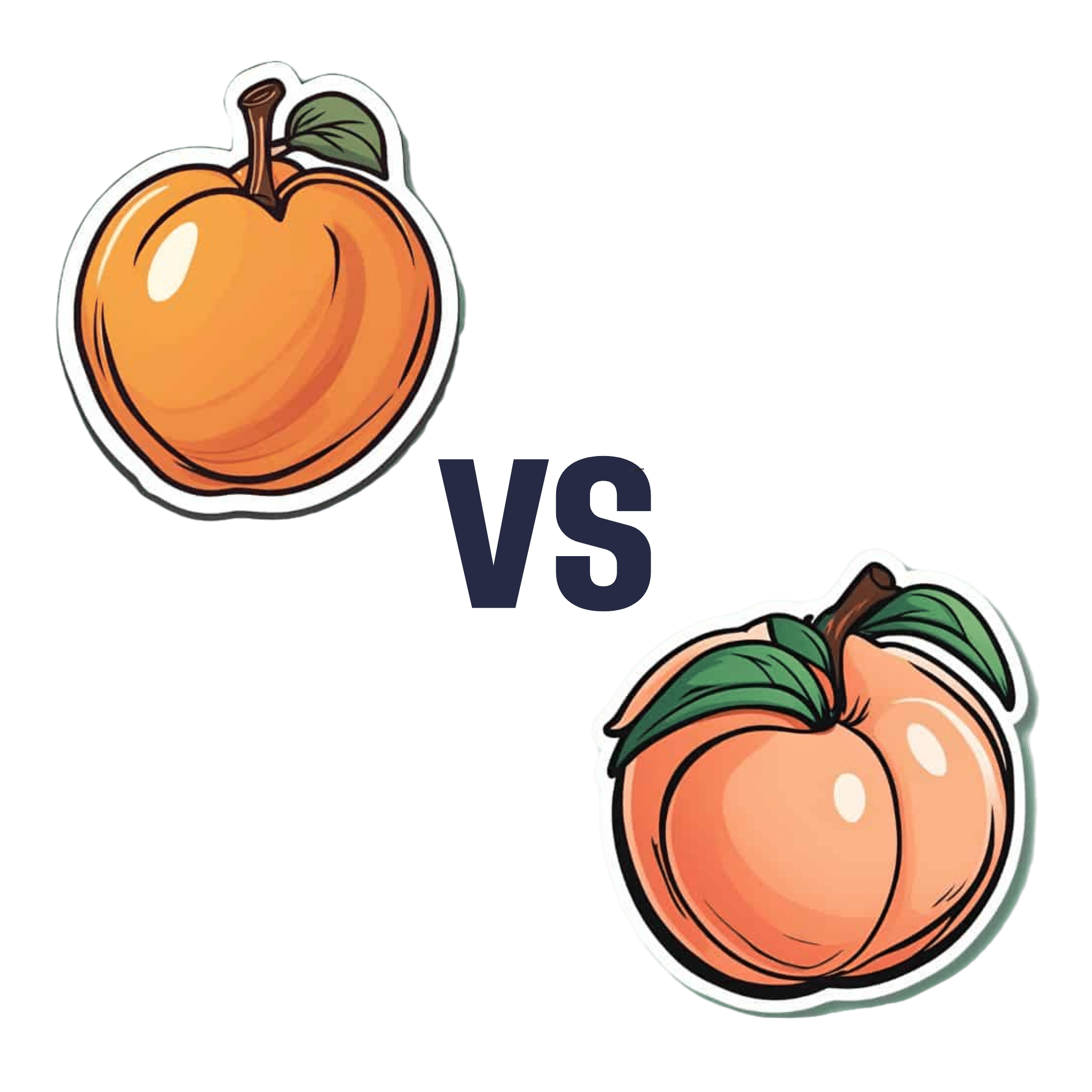
Apricots vs Peaches – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apricots to peaches, we picked the apricots.
Why?
Both are great! But there’s a clear winner:
In terms of macros, apricots have more fiber and, which is less important because the numbers are small, more protein. Apricots do also have more carbs, and/but carbs from whole fruit are not a problem for most people (especially because of the fiber), unless undertaking a very carb-controlled diet.
When it comes to vitamins, apricots sweep with more of vitamins A, B1, B2, B5, B6, B9, C, E, & K. Peaches meanwhile boast more vitamin B3, and that only marginally, as well as more choline.
In the category of minerals, apricots sweep again with more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. Peaches are not higher in any minerals.
Finally, if we consider polyphenols, apricots sweep yet again. The flavonols that peaches have, apricots have more of, and apricots have a long list of flavonols that peaches don’t.
Outside of flavonols, there is one (1) phenolic acid that peaches have more of (it’s 3-Caffeoylquinic acid), and it’s only slightly more, and it’s mostly in the skin which isn’t included if you buy your fruit ready-chopped. So in those cases, apricots would have the higher 3-Caffeoylquinic acid content anyway.
All in all, with their higher content of fiber, vitamins, minerals, and polyphenols, apricots easily win the day.
Enjoy both, though! Diversity is healthy!
Want to learn more?
You might like to read:
- Dried Apricots vs Dried Prunes – Which is Healthier?
- Which Sugars Are Healthier, And Which Are Just The Same? ← we know we link this one a lot, but we think it’s important for everyone to know how fruit is good and juice isn’t (and why, less that seem bizarrely arbitrary)
Take care!
Share This Post
-
How Primary Care Is Being Disrupted: A Video Primer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How patients are seeing their doctor is changing, and that could shape access to and quality of care for decades to come.
More than 100 million Americans don’t have regular access to primary care, a number that has nearly doubled since 2014. Yet demand for primary care is up, spurred partly by record enrollment in Affordable Care Act plans. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades.
KFF Health News senior correspondent Julie Appleby breaks down what is happening — and what it means for patients.
More From This Investigation
Primary Care Disrupted
Known as the “front door” to the health system, primary care is changing. Under pressure from increased demand, consolidation, and changing patient expectations, the model of care no longer means visiting the same doctor for decades. KFF Health News looks at what this means for patients.
Credits
Hannah Norman Video producer and animator Oona Tempest Illustrator and creative director KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
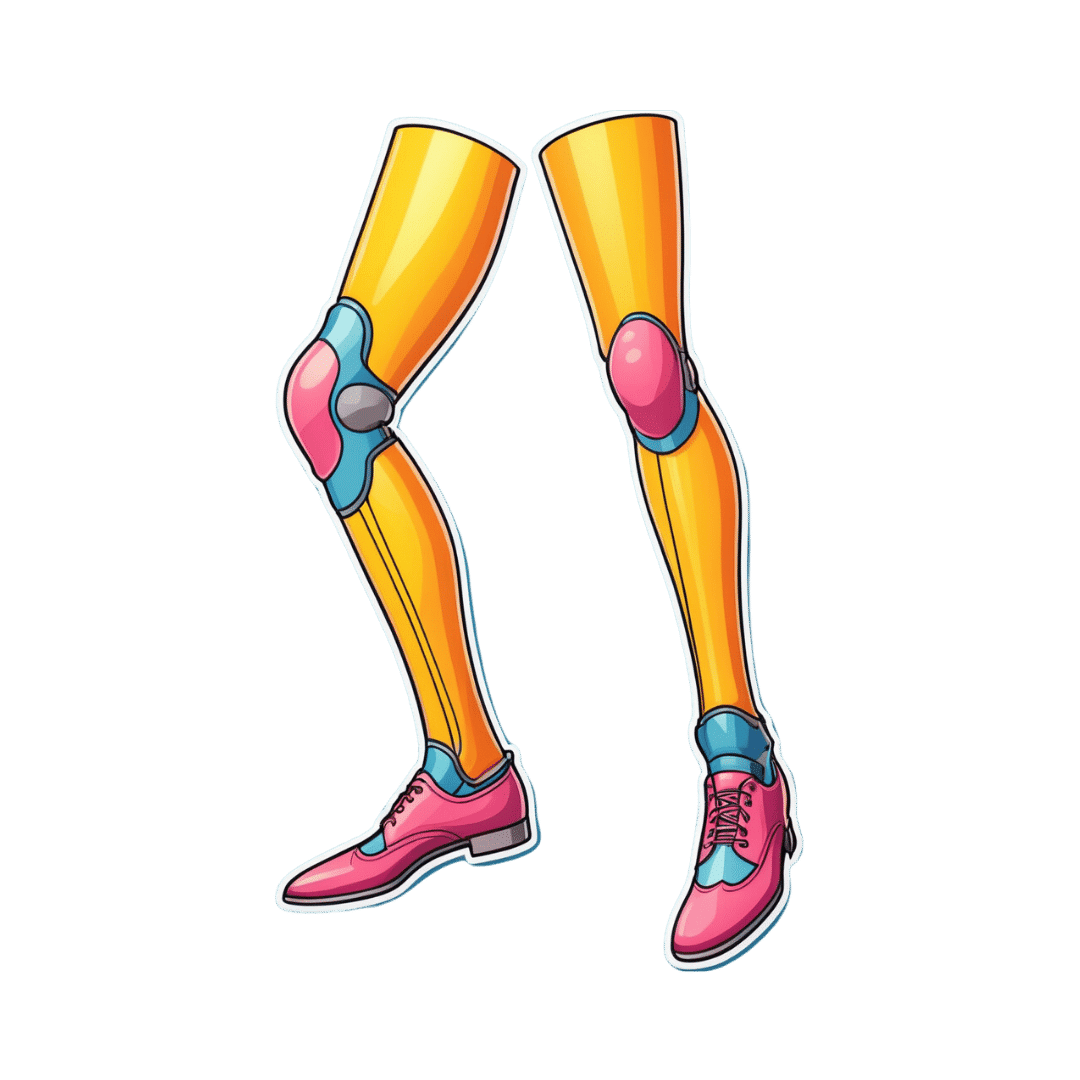
Health Insurers Limit Coverage of Prosthetic Limbs, Questioning Their Medical Necessity
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Michael Adams was researching health insurance options in 2023, he had one very specific requirement: coverage for prosthetic limbs.
Adams, 51, lost his right leg to cancer 40 years ago, and he has worn out more legs than he can count. He picked a gold plan on the Colorado health insurance marketplace that covered prosthetics, including microprocessor-controlled knees like the one he has used for many years. That function adds stability and helps prevent falls.
But when his leg needed replacing last January after about five years of everyday use, his new marketplace health plan wouldn’t authorize it. The roughly $50,000 leg with the electronically controlled knee wasn’t medically necessary, the insurer said, even though Colorado law leaves that determination up to the patient’s doctor, and his has prescribed a version of that leg for many years, starting when he had employer-sponsored coverage.
“The electronic prosthetic knee is life-changing,” said Adams, who lives in Lafayette, Colorado, with his wife and two kids. Without it, “it would be like going back to having a wooden leg like I did when I was a kid.” The microprocessor in the knee responds to different surfaces and inclines, stiffening up if it detects movement that indicates its user is falling.
People who need surgery to replace a joint typically don’t encounter similar coverage roadblocks. In 2021, 1.5 million knee or hip joint replacements were performed in United States hospitals and hospital-owned ambulatory facilities, according to the federal Agency for Healthcare Research and Quality, or AHRQ. The median price for a total hip or knee replacement without complications at top orthopedic hospitals was just over $68,000 in 2020, according to one analysis, though health plans often negotiate lower rates.
To people in the amputee community, the coverage disparity amounts to discrimination.
“Insurance covers a knee replacement if it’s covered with skin, but if it’s covered with plastic, it’s not going to cover it,” said Jeffrey Cain, a family physician and former chair of the board of the Amputee Coalition, an advocacy group. Cain wears two prosthetic legs, having lost his after an airplane accident nearly 30 years ago.
AHIP, a trade group for health plans, said health plans generally provide coverage when the prosthetic is determined to be medically necessary, such as to replace a body part or function for walking and day-to-day activity. In practice, though, prosthetic coverage by private health plans varies tremendously, said Ashlie White, chief strategy and programs officer at the Amputee Coalition. Even though coverage for basic prostheses may be included in a plan, “often insurance companies will put caps on the devices and restrictions on the types of devices approved,” White said.
An estimated 2.3 million people are living with limb loss in the U.S., according to an analysis by Avalere, a health care consulting company. That number is expected to as much as double in coming years as people age and a growing number lose limbs to diabetes, trauma, and other medical problems.
Fewer than half of people with limb loss have been prescribed a prosthesis, according to a report by the AHRQ. Plans may deny coverage for prosthetic limbs by claiming they aren’t medically necessary or are experimental devices, even though microprocessor-controlled knees like Adams’ have been in use for decades.
Cain was instrumental in getting passed a 2000 Colorado law that requires insurers to cover prosthetic arms and legs at parity with Medicare, which requires coverage with a 20% coinsurance payment. Since that measure was enacted, about half of states have passed “insurance fairness” laws that require prosthetic coverage on par with other covered medical services in a plan or laws that require coverage of prostheses that enable people to do sports. But these laws apply only to plans regulated by the state. Over half of people with private coverage are in plans not governed by state law.
The Medicare program’s 80% coverage of prosthetic limbs mirrors its coverage for other services. Still, an October report by the Government Accountability Office found that only 30% of beneficiaries who lost a limb in 2016 received a prosthesis in the following three years.
Cost is a factor for many people.
“No matter your coverage, most people have to pay something on that device,” White said. As a result, “many people will be on a payment plan for their device,” she said. Some may take out loans.
The federal Consumer Financial Protection Bureau has proposed a rule that would prohibit lenders from repossessing medical devices such as wheelchairs and prosthetic limbs if people can’t repay their loans.
“It is a replacement limb,” said White, whose organization has heard of several cases in which lenders have repossessed wheelchairs or prostheses. Repossession is “literally a punishment to the individual.”
Adams ultimately owed a coinsurance payment of about $4,000 for his new leg, which reflected his portion of the insurer’s negotiated rate for the knee and foot portion of the leg but did not include the costly part that fits around his stump, which didn’t need replacing. The insurer approved the prosthetic leg on appeal, claiming it had made an administrative error, Adams said.
“We’re fortunate that we’re able to afford that 20%,” said Adams, who is a self-employed leadership consultant.
Leah Kaplan doesn’t have that financial flexibility. Born without a left hand, she did not have a prosthetic limb until a few years ago.
Growing up, “I didn’t want more reasons to be stared at,” said Kaplan, 32, of her decision not to use a prosthesis. A few years ago, the cycling enthusiast got a prosthetic hand specially designed for use with her bike. That device was covered under the health plan she has through her county government job in Spokane, Washington, helping developmentally disabled people transition from school to work.
But when she tried to get approval for a prosthetic hand to use for everyday activities, her health plan turned her down. The myoelectric hand she requested would respond to electrical impulses in her arm that would move the hand to perform certain actions. Without insurance coverage, the hand would cost her just over $46,000, which she said she can’t afford.
Working with her doctor, she has appealed the decision to her insurer and been denied three times. Kaplan said she’s still not sure exactly what the rationale is, except that the insurer has questioned the medical necessity of the prosthetic hand. The next step is to file an appeal with an independent review organization certified by the state insurance commissioner’s office.
A prosthetic hand is not a luxury device, Kaplan said. The prosthetic clinic has ordered the hand and made the customized socket that will fit around the end of her arm. But until insurance coverage is sorted out, she can’t use it.
At this point she feels defeated. “I’ve been waiting for this for so long,” Kaplan said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are Electrolyte Supplements Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When To Take Electrolytes (And When We Shouldn’t!)
Any sports nutrition outlet will sell electrolyte supplements. Sometimes in the form of sports drinks that claim to be more hydrating than water, or tablets that can be dissolved in water to make the same. How do they work, and should we be drinking them?
What are electrolytes?
They’re called “electrolytes” because they are ionized particles (so, they have a positive or negative electrical charge, depending on which kind of ion they are) that are usually combined in the form of salts.
The “first halves” of the salts include:
- Sodium
- Potassium
- Calcium
- Magnesium
The “second halves” of the salts include:
- Chloride
- Phosphate
- Bicarbonate
- Nitrate
It doesn’t matter too much which way they’re combined, provided we get what we need. Specifically, the body needs them in a careful balance. Too much or too little, and bad things will start happening to us.
If we live in a temperate climate with a moderate lifestyle and a balanced diet, and have healthy working kidneys, usually our kidneys will keep them all in balance.
Why might we need to supplement?
Firstly, of course, you might have a dietary deficiency. Magnesium deficiency in particular is very common in North America, as people simply do not eat as much greenery as they ideally would.
But, also, you might sweat out your electrolytes, in which case, you will need to replace them.
In particular, endurance training and High Intensity Interval Training are likely to prompt this.
However… Are you in a rush? Because if not, you might just want to recover more slowly:
❝Vigorous exercise and warm/hot temperatures induce sweat production, which loses both water and electrolytes. Both water and sodium need to be replaced to re-establish “normal” total body water (euhydration).
This replacement can be by normal eating and drinking practices if there is no urgency for recovery.
But if rapid recovery (<24 h) is desired or severe hypohydration (>5% body mass) is encountered, aggressive drinking of fluids and consuming electrolytes should be encouraged to facilitate recovery❞
Source: Fluid and electrolyte needs for training, competition, and recovery
Should we just supplement anyway, as a “catch-all” to be sure?
Probably not. In particular, it is easy to get too much sodium in one’s diet, let alone by supplementation.And, oversupplementation of calcium is very common, and causes its own health problems. See:
To look directly to the science on this one, we see a general consensus amongst research reviews: “this is complicated and can go either way depending on what else people are doing”:
- Trace minerals intake: risks and benefits for cardiovascular health
- Electrolyte minerals intake and cardiovascular health
Well, that’s not helpful. Any clearer pointers?
Yes! Researchers Latzka and Mountain put together a very practical list of tips. Rather, they didn’t put it as a list, but the following bullet points are information extracted directly from their abstract, though we’ve also linked the full article below:
- It is recommended that individuals begin exercise when adequately hydrated.
- This can be facilitated by drinking 400 mL to 600 mL of fluid 2 hours before beginning exercise and drinking sufficient fluid during exercise to prevent dehydration from exceeding 2% body weight.
- A practical recommendation is to drink small amounts of fluid (150-300 mL) every 15 to 20 minutes of exercise, varying the volume depending on sweating rate.
- During exercise lasting less than 90 minutes, water alone is sufficient for fluid replacement
- During prolonged exercise lasting longer than 90 minutes, commercially available carbohydrate electrolyte beverages should be considered to provide an exogenous carbohydrate source to sustain carbohydrate oxidation and endurance performance.
- Electrolyte supplementation is generally not necessary because dietary intake is adequate to offset electrolytes lost in sweat and urine; however, during initial days of hot-weather training or when meals are not calorically adequate, supplemental salt intake may be indicated to sustain sodium balance.
Source: Water and electrolyte requirements for exercise
Bonus tip:
We’ve talked before about the specific age-related benefits of creatine supplementation, but if you’re doing endurance training or HIIT, you might also want to consider a creatine-electrolyte combination sports drink (even if you make it yourself):
Where can I get electrolyte supplements?
They’re easy to find in any sports nutrition store, or you can buy them online; here’s an example product on Amazon for your convenience
You can also opt for natural and/or homemade electrolyte drinks:
Healthline | 8 Healthy Drinks Rich in Electrolytes
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Menopause: 50 Things You Need to Know – by Dr. Felice Gersh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you list 50 important facts about the menopause? If not, you’ll surely find things to learn in here.
The book is divided into three main sections:
- What to expect in perimenopause
- What to expect in early menopause
- What to expect in late menopause
Each section comes with an alarming array of symptoms, ranging from perimenopause fatigue and acne to late menopause tooth loss and vaginal prolapse. This is not to say that everyone will experience everything (fortunately), but rather, that these are the things that can happen and should not arrive unexpected.
Helpfully, of course, Dr. Gersh also gives advice on how to improve your energy and skin health, as well as keep your teeth and vagina in place. And similar professional insights for the rest of the “50 things you need to know”.
The style is like one big (182 pages) patient information leaflet—thus, very clear, explaining everything, and offering reassurance where possible and also what things are reasonable cause for seeking personalized medical attention.
Bottom line: if menopause is in your future, present, or very near past, this is an excellent book for you.
Click here to check out Menopause: 50 Things You Need To Know, and know them!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: