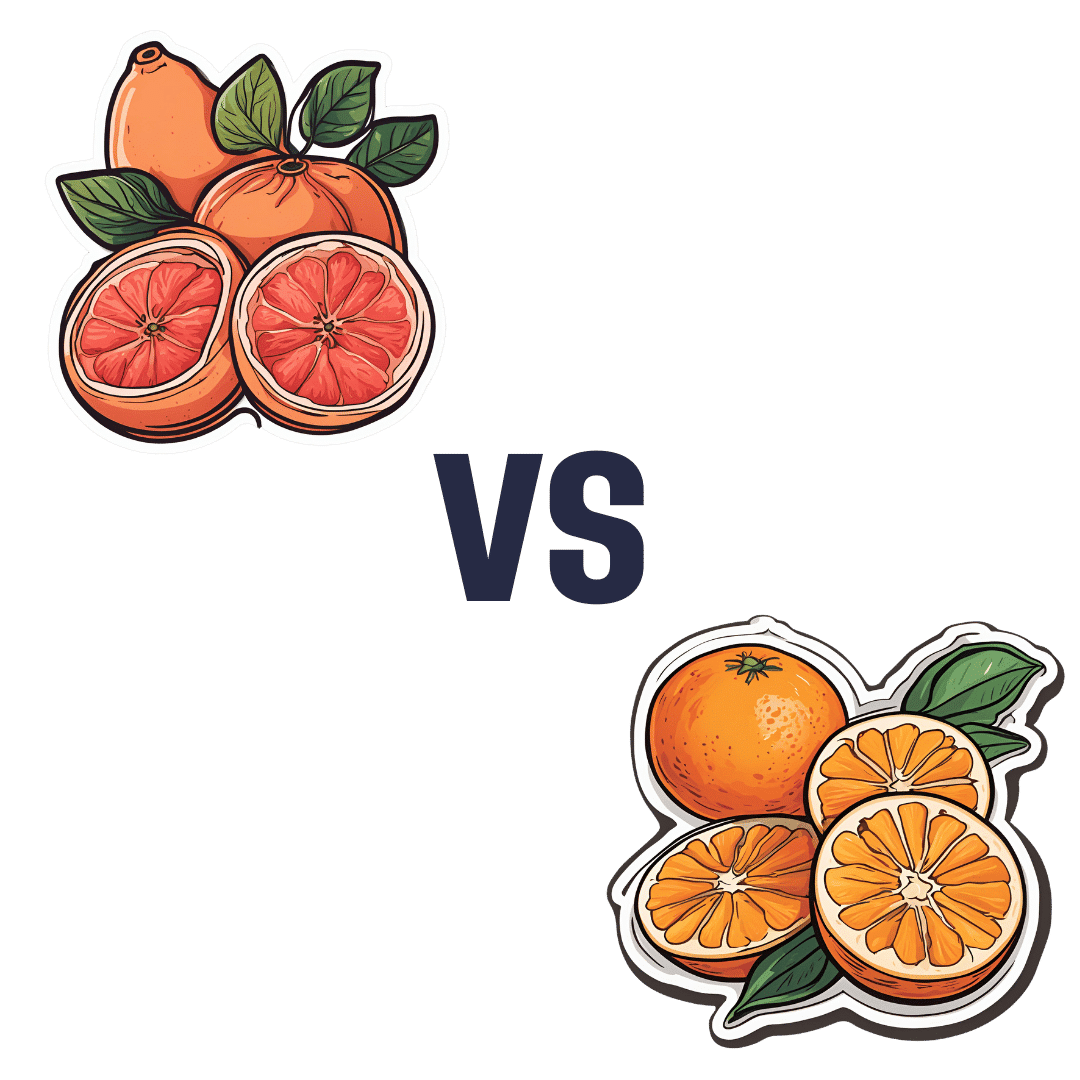
Grapefruit vs Orange – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to orange, we picked the orange.
Why?
It’s easy, when guessing which is the healthier out of two things, to guess that the more expensive or perhaps less universally available one is the healthier. But it’s not always so, and today is one of those cases!
In terms of macros, they are very similar fruits, with almost identical levels of carbohydrates, proteins, and fats, as well as water. Looking more carefully, we find that grapefruit’s sugars contain a slightly high proportion of fructose; not enough to make it unhealthy by any means (indeed, no whole unprocessed fruit is unhealthy unless it’s literally poisonous), but it is a thing to note if we’re micro-analysing the macronutrients. Also, oranges have slightly more fiber, which is always a plus.
When it comes to vitamins, oranges stand out with more of vitamins B1, B2, B3, B6, B9, C, and E, while grapefruit boasts more vitamin A (hence its color). Still, we’re calling this category another win for oranges.
In the category of minerals, oranges again sweep with more calcium, copper, iron, magnesium, manganese, potassium, and selenium, while grapefruit has just a little more phosphorus. So, another easy win for oranges.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold. It can also be found in lower quantities in Seville (sour) oranges, and it’s not present (or at least, if it is, it’s in truly tiny quantities) in most oranges.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
All in all, today’s sections add up to an overwhelming win for oranges!
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why We Remember – by Dr. Charan Ranganath
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we get older, forgetfulness can become more of a spectre; the threat that one day it could be less “where did I put my sunglasses?” and more “who is this person claiming to be my spouse?”.
Dr. Ranganath explores in this work the science of memory, from a position of neurobiology, but also in application. How and why we remember, and how and why we forget, and how and why both are important.
There is a practical element to the book too; we read about things that increase our tendency to remember (and things that increase our tendency to forget), and how we can leverage that information to curate our memory in an active, ongoing basis.
The style of the book is quite casual in tone for such a serious topic, but there’s plenty of hard science too; indeed there are 74 pages of bibliography cited.
Bottom line: while filled with a lot of science, this is also a very human book, and a helpful guide to building and preserving our memory.
Click here to check out “Why We Remember”, and learn how to hold on to what matters the most!
Share This Post
-
Do Essential Oils Really Have Medicinal Properties?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Do essential oils really have scientific merit?❞
Great question! Assuming you mean “…for medicinal purposes” then it really depends on the oil in question.
For example, one can probably buy a big book of essential oils from a New Age store, and a lot of claims for different oils will not have any scientific backing whatsoever.
However! Some definitely do. For example, we wrote a little while back about ginger:
Ginger Does A Lot More Than You Think
Now, the active compound that gives ginger those properties and more is gingerol. Which is usually found as pure ginger oil, in other words, ginger essential oil.
Another essential oil that definitely does have benefits is that of Boswellia serrata, commonly known as frankincense. It can be used in various forms, and the essential oil is one of them; see:
- Five Supplements That Actually Work Vs Arthritis
- When Painkillers Aren’t Helping, These Things Might: Science-Based Alternative Pain Relief
Meanwhile, menthol, the essential oil of peppermint, has its pros and cons:
Peppermint For Digestion & Against Nausea: How Useful Is Peppermint, Really?
And lavender essential oil does really have a sedative effect:
Herbs for Evidence-Based Health & Healing
If you have a different, particular essential oil in mind, let us know, and we can do a deep-dive on it for one of our “Research Review” editions!
A note on safety
Essential oils are pure and undiluted extracts of what’s usually a particularly potent chemical from a plant. Two things to bear in mind about this:
- Just because a chemical is potent, does not mean it will necessarily help you in a specific way, or indeed at all. On the contrary, many potent chemicals are simply harmful. So, be careful.
- Essential oils being so strong means that usually only a drop or two is required for effects; consult available literature (or ask us to do that for you!), and employ good safety practices such as:
- Do not use undiluted essential oils on your skin or internally
- If you are going to use it internally (diluted, following instructions from a reputable source, and with your doctor’s blessing, please) then test it on your skin first at the same dilution, in case of any adverse reaction.
- However you are using it, if you have any kind of adverse reaction, stop, and seek medical attention if it’s severe and/or it persists.
Take care!
Share This Post
-
Eat to Beat Your Diet – by Dr. William Li
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed Dr. Li’s excellent “Eat To Beat Disease”, so you may be wondering how much overlap there is. While he does still cover such topics as angiogenesis, organ regeneration, microbiome health, DNA protection, and immunological considerations, and much of the dietary advice is similar, most of the explanation is different.
Because, this time, rather than looking at beating disease in general, there’s a much stronger focus on metabolic disease in particular, and yes, for those who want to do so, losing fat.
The scientific explanations are in-depth, such that you come way with not merely “I should eat an avocado once in a while”, but a comprehensive understanding of the body’s metabolic processes, from the chemistry to the organs involved, from the cellular to the systemic.
The style is on the hard end of pop-science. It’s approachably readable, while having a lot of densely-packed information with minimal fluff. You will be more than getting your money’s worth out of its 496 pages.
Bottom line: if you’d like to perk up your metabolism with a dietary approach that’s enjoyable and very restrictive, then this book will arm you with the knowledge to do that.
Click here to check out Eat To Beat Your Diet, and eat to beat your diet!
Share This Post
Related Posts
-
Proteinaholic – by Dr. Garth Davis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Protein is important, yes. However, you can have too much of a good thing, and you can also get it from bad sources that do more harm than good.
That’s what this book is about, and how to go about understanding the science in a world where marketing has outstripped the conclusions of research scientists.
Firstly, let’s mention that Dr. Davis’ main issue here is (as the subtitle suggests) about animal proteins, not plant-based proteins. The former are associated with very many health risks that the latter are not. And yes, even just the lean protein, not considering the animal fat.
He does not argue that the reader must, or even necessarily needs to, adopt a vegan diet. However, he does argue for minimizing animal proteins, and getting more plants in.
A lot of the book is about the research to back this approach, and specifically, it’s largely a polemic against animal protein. He also shares anecdotes throughout, about his own health journey—from an overweight cheeseburger-fueled heart attack machine with exciting cholesterol levels, to a healthy, muscular, plant-fueled advocate for healthier eating.
He talks us through the science at hand, including chapters for each of the main health risks associated with meat consumption, as well as how the science got misrepresented by popular marketing for [not necessarily, but usually] meat-heavy diets such as Atkins and Paleo. That yes, they will give short term weight loss, but bring extra health risks in the longer term, and how.
Bottom line: if you’d like to cut down your meat consumption but worry “will I get enough protein?”, this book will set your mind at ease with an abundance of science.
Click here to check out Proteinaholic, and give your body better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
You Are Not a Before Picture – by Alex Light
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of year, and many of us are looking at what we’ll do in the coming days, weeks, and months to level-up our health. So… Is this a demotivational book?
Quite the opposite! It’s rather a case of an often much-needed reminder to ensure that our plans are really our own, and really are what’s best for us. Why wouldn’t they be, you ask?
Much of diet culture (ubiquitous! From magazine covers to movie stars to the models advertising anything from health insurance to water filters) has us reaching for “body goals” that are not possible without a different skeleton and genes and compromises and post-production edits.
Alex Light—herself having moved from the fashion and beauty industry into health education—sets out in a clear, easy-reading manner, how we can look after ourselves, not be neglectful of our bodies, and/but also not get distracted into unhelpful, impossible, castles-in-the-air.
Bottom line: you cannot self-hate your way into good health, and good health will always be much more attainable than a body that’s just not yours. This book can help you sort out which is which.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is ‘breathwork’? And do I need to do it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From “breathwork recipes” to breathing techniques, many social media and health websites are recommending breathwork to reduce stress.
But breathwork is not new. Rather it is the latest in a long history of breathing techniques such as Pranayama from India and qigong from China. Such practices have been used for thousands of years to promote a healthy mind and body.
The benefits can be immediate and obvious. Try taking a deep breath in through your nose and exhaling slowly. Do you feel a little calmer?
So, what’s the difference between the breathing we do to keep us alive and breathwork?
Taras Grebinets/Shutterstock Breathwork is about control
Breathwork is not the same as other mindfulness practices. While the latter focus on observing the breath, breathwork is about controlling inhalation and exhalation.
Normally, breathing happens automatically via messages from the brain, outside our conscious control. But we can control our breath, by directing the movement of our diaphragm and mouth.
The diaphragm is a large muscle that separates our thoracic (chest) and abdominal (belly) cavities. When the diaphragm contracts, it expands the thoracic cavity and pulls air into the lungs.
Controlling how deep, how often, how fast and through what (nose or mouth) we inhale is the crux of breathwork, from fire breathing to the humming bee breath.
Breathwork can calm or excite
Even small bits of breathwork can have physical and mental health benefits and complete the stress cycle to avoid burnout.
Calming breathwork includes diaphragmatic (belly) breathing, slow breathing, pausing between breaths, and specifically slowing down the exhale.
In diaphragmatic breathing, you consciously contract your diaphragm down into your abdomen to inhale. This pushes your belly outwards and makes your breathing deeper and slower.
You can also slow the breath by doing:
- box breathing (count to four for each of four steps: breathe in, hold, breathe out, hold), or
- coherent breathing (controlled slow breathing of five or six breaths per minute), or
- alternate nostril breathing (close the left nostril and breathe in slowly through the right nostril, then close the right nostril and breathe out slowly through the left nostril, then repeat the opposite way).
You can slow down the exhalation specifically by counting, humming or pursing your lips as you breathe out.
In contrast to these calming breathing practices, energising fast-paced breathwork increases arousal. For example, fire breathing (breathe in and out quickly, but not deeply, through your nose in a consistent rhythm) and Lion’s breath (breathe out through your mouth, stick your tongue out and make a strong “haa” sound).
What is happening in the body?
Deep and slow breathing, especially with a long exhale, is the best way to stimulate the vagus nerves. The vagus nerves pass through the diaphragm and are the main nerves of the parasympathetic nervous system.
Simulating the vagus nerves calms our sympathetic nervous system (fight or flight) stress response. This improves mood, lowers the stress hormone cortisol and helps to regulate emotions and responses. It also promotes more coordinated brain activity, improves immune function and reduces inflammation.
Taking deep, diaphragmatic breaths also has physical benefits. This improves blood flow, lung function and exercise performance, increases oxygen in the body, and strengthens the diaphragm.
Slow breathing reduces heart rate and blood pressure and increases heart rate variability (normal variation in time between heart beats). These are linked to better heart health.
Taking shallow, quick, rhythmic breaths in and out through your nose stimulates the sympathetic nervous system. Short-term, controlled activation of the stress response is healthy and develops resilience to stress.
Breathing in through the nose
We are designed to inhale through our nose, not our mouth. Inside our nose are lots of blood vessels, mucous glands and tiny hairs called cilia. These warm and humidify the air we breathe and filter out germs and toxins.
We want the air that reaches our airways and lungs to be clean and moist. Cold and dry air is irritating to our nose and throat, and we don’t want germs to get into the body.
Nasal breathing increases parasympathetic activity and releases nitric oxide, which improves airway dilation and lowers blood pressure.
Consistently breathing through our mouth is not healthy. It can lead to pollutants and infections reaching the lungs, snoring, sleep apnoea, and dental issues including cavities and jaw joint problems.
Breathing can be high and shallow when we are stressed. mi_viri/Shutterstock A free workout
Slow breathing – even short sessions at home – can reduce stress, anxiety and depression in the general population and among those with clinical depression or anxiety. Research on breathwork in helping post-traumatic stress disorder (PTSD) is also promising.
Diaphragmatic breathing to improve lung function and strengthen the diaphragm can improve breathing and exercise intolerance in chronic heart failure, chronic obstructive pulmonary disease and asthma. It can also improve exercise performance and reduce oxidative stress (an imbalance of more free radicals and/or less antioxidants, which can damage cells) after exercise.
Waiting at the lights? This could be your signal to do some breathwork. doublelee/Shutterstock A mind-body connection you can access any time
If you feel stressed or anxious, you might subconsciously take shallow, quick breaths, but this can make you feel more anxious. Deep diaphragmatic breaths through your nose and focusing on strong exhalations can help break this cycle and bring calm and mental clarity.
Just a few minutes a day of breathwork can improve your physical and mental health and wellbeing. Daily deep breathing exercises in the workplace reduce blood pressure and stress, which is important since burnout rates are high.
Bottom line: any conscious control of your breath throughout the day is positive.
So, next time you are waiting in a line, at traffic lights or for the kettle to boil, take a moment to focus on your breath. Breathe deeply into your belly through your nose, exhale slowly, and enjoy the benefits.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong and Judy Pickard, Senior Lecturer, Clinical Psychology, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: