Top 10 Early Warning Signs Of Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s a harmless momentary mind-blank, and what’s a potential warning sign of dementia? Dementia Careblazers, a dementia care organization, has input:
The signs
With the caveat that this is a list of potential warning signs, not a diagnostic tool, the 10 signs are:
- Memory loss: e.g. forgetting important or well-learned information, such as one’s home address
- Challenges in planning or solving problems: e.g. difficulty with tasks such as paying bills (for organizational rather than financial reasons), following recipes, or managing medications
- Difficulty completing familiar tasks: e.g. trouble remembering rules of a familiar game, or directions to a familiar place
- Confusion with place or time: e.g. forgetting where one is, or making mistakes with the date, season, or other time-related details. Note that anyone can be momentarily unsure of today’s date, but if someone thinks it’s 1995, probably something wrong is not quite right. Similarly, being wrong about who is the current national leader is often used as a test, too—assuming countries with enough political stability to not have five different national leaders in the past four years, including one who did not outlast a lettuce *side-eyeing the UK*
- Trouble understanding visual images and spatial relationships: e.g. increased clumsiness, difficulty parking, or bumping into objects
- New problems with speaking or writing: e.g. losing track in conversations, or struggling to find the right words
- Misplacing things: e.g. losing items and being unable to retrace one’s steps to find them
- Decreased or poor judgment: e.g. falling for scams, giving out too much information or money without investigating appropriately first
- Withdrawal from social activities or hobbies: e.g. losing interest in activities one used to enjoy or avoiding social interactions
- Changes in mood and personality: e.g. increased irritability, anxiety, or other noticeable changes in behavior and personality
For more information on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Dementia: Spot The Signs (Because None Of Us Are Immune)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Processed Is The Food You Buy, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ultraprocessed foods are a) ubiquitous in industrialized nations b) generally not fabulous for the health. See for example:
- Eat To Beat Cancer ← skipping the ultraprocessed foods is one main point
- What To Leave Off Your Table (To Stay Off This Surgeon’s) ← have a guess
Abstaining from ultraprocessed food can also be difficult psychologically, because they are generally engineered specifically to trigger certain physiological responses, often with their combination of sweet and/or salty flavors with simple carbohydrates that will zip straight into one’s veins and feel immediately rewarding, even if there is a health price to pay later.
And worse, being habituated to ultraprocessed food can make unprocessed or minimally-processed food seem less appealing:
What causes food cravings? And what can we do about them?
Fortunately, we can reverse this, and once we get habituated to unprocessed or minimally-processed food, the ultraprocessed will start to seem like not-food to us. You will wonder: how did I ever eat that crap?
Now, one other thing to bear in mind:
There is a scale of “badness”
You might recall this article:
Not all ultra-processed foods are bad for your health, whatever you might have heard
For example, Reese’s confectionary and Huel nutrition powder are both ultra-processed, but one is definitely better than the other.
See also: Are plant-based burgers really bad for your heart? Here’s what’s behind the scary headlines
Some comparisons are obvious; others, not so much. So, how to tell the difference?
The “True Food” Scale
A large study analyzed ingredient lists, nutrition facts, and prices of over 50,000 food items from Target, Whole Foods, and Walmart. Using a rigorous statistical method, they assigned processing scores and compiled data into a giant database, with results published publicly.
You can find the study here:
Prevalence of processed foods in major US grocery stores
That in and of itself doesn’t tell a lot that’s useful to the consumer, because the paper itself does not have all of the data from all 50,000 food items, just the aggregate results, trends, implications for public health, and suggestions for public health policy.
However, what does tell a lot, is the public face of the database itself, which you can browse for free, and look up your regular shopping items, if you are wondering “are these textured soy pieces basically a step away from soy beans, or a frankenfood that will murder me in my sleep?”
How it works: it examines each food, its listed ingredients, and what is known about the processedness of such ingredients. It also draws a distinction between ingredients and additives, rendering the entire process of the production of the food into an “ingredient tree”, showing what was added to what along the way. Minimally-processed foods will have barely an ingredient sapling, while ultraprocessed foods will have an ingredient tree whose branches can barely be counted, they are so numerous. It’s not just about the number of ingredients though; it’s about the processes that each underwent.
How it represents this data: you can look at the food in the database, and it’ll tell you the ingredients and nutritional facts (which you probably knew already; it’s written on the packaging), and then show you how processed it is, and then ranking that against all other foods in the database of the same kind.
So for example, if you are looking at a pizza (have you ever noticed how some are marketed with bright flashy colors, and others in natural tones to suggest minimal processing? This is marketing, not reliable information! Sometimes the product that looks healthier, isn’t!), then it’ll give it a score reflecting how it ranks compared to all other pizze in the database. This number is out of a hundred, and it reflects the percentile into which it falls.
So for example, if the score your pizza gets is 47, then that means that if you looked at it next to 99 others, on average your pizza would would rank better than 46 of them and worse than 53 of them.
In other words, the lower the score, the less processed it is on the whole.
Here’s a side-by-side example of two cakes, one of which got a score of 3, and the other got a score of 61:
Mini No Sugar Added Cheesecake vs EDWARDS Desserts Original Whipped Cheesecake
And here is the main menu of the database, in which you can use the search function to look up the food you want to check, or else browse by category:
The TrueFood Database: Search or Browse (it’s free!)
Enjoy!
Want to know more?
You might like this book that we reviewed a little while back:
Ultra-Processed People: The Science Behind Food That Isn’t Food – by Dr. Chris van Tulleken
Enjoy!
Share This Post
-
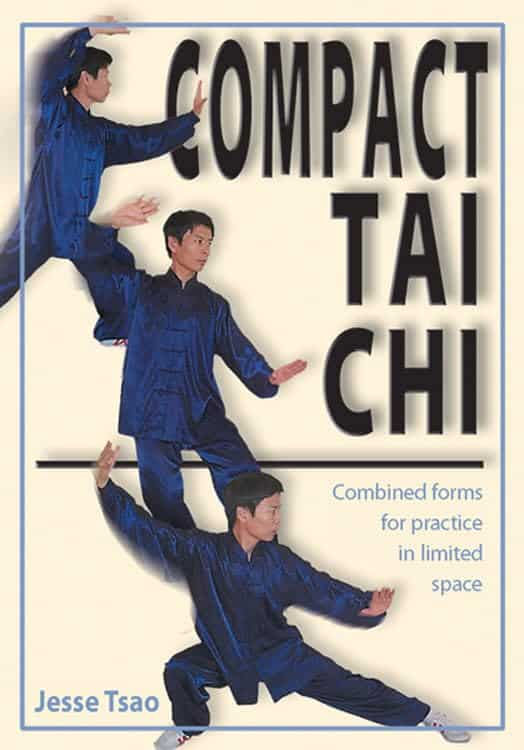
Compact Tai Chi – by Dr. Jesse Tsao
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A very frustrating thing when practicing tai chi, especially when learning, is the space typically required. We take a step this way and lunge that way and turn and now we’ve kicked a bookcase. Add a sword, and it’s goodnight to the light fixtures at the very least.
While a popular suggestion may be “do it outside”, we do not all have the luxury of living in a suitable climate. We also may prefer to practice in private, with no pressing urge to have an audience.
Tsao’s book, therefore, is very welcome. But how does he do it? The very notion of constriction is antithetical to tai chi, after all.
He takes the traditional forms, keeps the movements mostly the same, and simply changes the order of them. This way, the practitioner revolves around a central point. Occasionally, a movement will become a smaller circle than it was, but never in any way that would constrict movement.
Of course, an obvious question for any such book is “can one learn this from a book?” and the answer is complex, but we would lean towards yes, and insofar as one can learn any physical art from a book, this one does a fine job. It helps that it builds up progressively, too.
All in all, this book is a great choice for anyone who’s interested in taking up tai chi, and/but would like to do so without leaving their home.
Share This Post
-
Exercises for Aging-Ankles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can Ankles Deterioration be Stopped?
As we all know (or have experienced!), Ankle mobility deteriorates with age.
We’re here to argue that it’s not all doom and gloom!
(In fact, we’ve written about keeping our feet, and associated body parts, healthy here).
This video by “Livinleggings” (below) provides a great argument that yes, ankle deterioration can be stopped, or even reversed. It’s a must-watch for anyone from yoga enthusiasts to gym warriors who might be unknowingly crippling their ankle-health.
How We Can Prioritise Our Ankles
Poor ankle flexibility isn’t just an inconvenience – it’s a direct route to knee issues, hip hiccups, and back pain. More importantly, ankle strength is a core component of building overall mobility.
With 12 muscles in the ankle, it can be overwhelming to work out which to strengthen – and how. But fear not, we can prioritise three of the twelve: the calf duo (gastrocnemius and soleus) and the shin’s main muscle, the tibialis anterior.
The first step is to test yourself! A simple wall test reveals any hidden truths about your ankle flexibility. Go to the 1:55 point in the video to see how it’s done.
If you can’t do it, you’ve got work to be done.
If you read the book we recommended on great functional exercises for seniors, then you may already be familiar with some super ankle exercises.
Otherwise, these four ankle exercises are a great starting point:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
Related Posts
-
Syphilis Is Killing Babies. The U.S. Government Is Failing to Stop the Disease From Spreading.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Karmin Strohfus, the lead nurse at a South Dakota jail, punched numbers into a phone like lives depended on it. She had in her care a pregnant woman with syphilis, a highly contagious, potentially fatal infection that can pass into the womb. A treatment could cure the woman and protect her fetus, but she couldn’t find it in stock at any pharmacy she called — not in Hughes County, not even anywhere within an hour’s drive.
Most people held at the jail where Strohfus works are released within a few days. “What happens if she gets out before I’m able to treat her?” she worried. Exasperated, Strohfus reached out to the state health department, which came through with one dose. The treatment required three. Officials told Strohfus to contact the federal Centers for Disease Control and Prevention for help, she said. The risks of harm to a developing baby from syphilis are so high that experts urge not to delay treatment, even by a day.
Nearly three weeks passed from when Strohfus started calling pharmacies to when she had the full treatment in hand, she said, and it barely arrived in time. The woman was released just days after she got her last shot.
Last June, Pfizer, the lone U.S. manufacturer of the injections, notified the Food and Drug Administration of an “impending stock out” that it anticipated would last a year. The company blamed “an increase in syphilis infection rates as well as competitive shortages.”
Across the country, physicians, clinic staff and public health experts say that the shortage is preventing them from reining in a surge of syphilis and that the federal government is downplaying the crisis. State and local public health authorities, which by law are responsible for controlling the spread of infectious diseases, report delays getting medicine to pregnant people with syphilis. This emergency was predictable: There have been shortages of this drug in eight of the last 20 years.
Yet federal health authorities have not prevented the drug shortages in the past and aren’t doing much to prevent them in the future.
Syphilis, which is typically spread during sex, can be devastating if it goes untreated in pregnancy: About 40% of babies born to women with untreated syphilis can be stillborn or die as newborns, according to the CDC. Infants that survive can suffer from deformed bones, excruciating pain or brain damage, and some struggle to hear, see or breathe. Since this is entirely preventable, a baby born with syphilis is a shameful sign of a failing public health system.
In 2022, the most recent year for which the CDC has data available, more than 3,700 babies were infected with syphilis, including nearly 300 who were stillborn or died as infants. More than 50% of these cases occurred because, even though the pregnant parent was diagnosed with syphilis, they were never properly treated.
That year, there were 200,000 cases identified in the U.S., a 79% increase from five years before. Infection rates among pregnant people and babies increased by more than 250% in that time; South Dakota, where Strohfus works, had the highest rates — including a more than 400% increase among pregnant women. Statewide, the rate of babies born with the disease, a condition known as congenital syphilis, jumped more than 40-fold in just five years.
And that was before the current shortage of shots.
In Mississippi, the state with the second highest rate of syphilis in pregnant women, Dr. Caroline Weinberg started having trouble this summer finding treatments for her clinic’s patients, most of whom are uninsured, live in poverty or lack transportation. She began spending hours each month scouring medicine suppliers’ websites for available doses of the shots, a form of penicillin sold under the brand name Bicillin L-A.
“The way people do it for Taylor Swift, that’s how I’ve been with the Bicillin shortage,” Weinberg said. “Desperately checking the websites to see what I can snag.”
The shortage is driving up infection rates even further.
In a November survey by the National Coalition of STD Directors, 68% of health departments that responded said the drug shortage will cause syphilis rates in their area to increase, further crushing the nation’s most disadvantaged populations.
“This is the most basic medicine,” said Meghan O’Connell, chief public health officer for the Great Plains Tribal Leaders’ Health Board, which represents 18 tribal communities in South Dakota and three other states. “We allow ourselves to continue to not have enough, and it impacts so many people.”
ProPublica examined what the federal government has done to manage the crisis and the ways in which experts say it has fallen short.
The government could pressure Pfizer to be more transparent.
Twenty years ago, there were at least three manufacturers of the syphilis shot. Then Pfizer, one of the manufacturers, purchased the other two companies and became the lone U.S. supplier.
Pfizer’s supply has fallen short since then. In 2016, the company announced a shortage due to a manufacturing issue; it lasted two years. Even during times when Pfizer had not notified the FDA of an official shortage, clinics across the country told ProPublica, the shots were often hard to get.
Several health officials said they would like to see the government use its power as the largest purchaser of the drug to put pressure on Pfizer to produce adequate supplies and to be more transparent about how much of the drug they have on hand, when it will be widely available and how stable the supply will be going forward.
In response to questions, Pfizer said there are two reasons its supply is falling short. One, the company said, was a surge in use of the pediatric form of the drug after a shortage of a different antibiotic last winter. Pfizer also blamed a 70% increase in demand for the adult shots since last February, which it described as unexpected.
Public health experts say the increase in cases and subsequent rise in demand was easy to see coming. Officials have been raising the alarm about skyrocketing syphilis cases for years. “If Pfizer was truly caught completely off guard, it raises significant questions about the competency of the company to forecast obvious infectious disease trends,” a coalition of organizations wrote to the White House Drug Shortage Task Force in September.
Pfizer said it is consistently communicating with the CDC and FDA about its supply and that it has been transparent with public health groups and policymakers.
The FDA has a group dedicated to addressing drug shortages. But Valerie Jensen, associate director of that staff, said the FDA can’t force manufacturers to make more of a drug. “It is up to manufacturers to decide how to respond to that increased demand.” she said. “What we’re here to do is help with those plans.”
Pfizer said it had a target of increasing production by about 20% in 2023 but faced delays toward the end of the year. The company did not explain the reason for those delays.
The company said it has invested $38 million in the last five years in the Michigan facility where it makes the shots and that it is increasing production capacity. It also said it is adding evening shifts at the facility and actively recruiting and training new workers. Pfizer said it also reduced manufacturing time from 110 to 50 days. By the end of June, the company expects the supply to recover, which it described as having eight weeks of inventory based on its forecast demands with no disruptions in sight.
The government could manufacture the drug itself.
Having only one supplier for a drug, especially one of public health importance, makes the country vulnerable to shortages. With just one manufacturer, any disruption — contamination at a plant, a shortage of raw materials, a severe weather event or a flawed prediction of demand — can put lives at risk. What’s ultimately needed, public health experts say, is another manufacturer.
Congressional Democrats recently introduced a bill that would authorize the U.S. Department of Health and Human Services to manufacture generic drugs in exactly this scenario, when there are few manufacturers and regular shortages. Called the Affordable Drug Manufacturing Act, it would also establish an office of drug manufacturing.
This same bill was introduced in 2018, but it didn’t have bipartisan support and was never taken up for a vote. Sen. Elizabeth Warren, the Massachusetts Democrat who introduced the bill in the Senate, said she’s hopeful this time will be different. Lawmakers from both parties understand the risks created by drug shortages, and COVID-19 helped everyone understand the role the government can play to boost manufacturing.
Still, it’s unlikely to be passed with the current gridlock in Congress.
The government could reserve syphilis drugs for infected patients.
Responding to the shortage of shots to treat the disease, the CDC in July asked health care providers nationwide to preserve the scarce remaining doses for people who are pregnant. The shots are considered the gold standard treatment for anyone with syphilis, faster and with fewer side effects than an alternative pill regimen. And for people who are pregnant, the pills are not an option; the shots are the only safe treatment.
Despite that call, the military is giving shots to new recruits who don’t have syphilis, to prevent outbreaks of severe bacterial respiratory infections. The Army has long administered this treatment at boot camps held at Fort Leonard Wood, Fort Moore and Fort Sill. The Army has been unable to obtain the shots several times in the past few years, according to the U.S. Army Center for Initial Military Training. But the Defense Health Agency’s pharmacy operations center has been working with Pfizer to ensure military sites can get them, a spokesperson for the Defense Health Agency said.
“Until we think about public health the way we think about our military, we’re not going to see a difference,” said Dr. John Vanchiere, chief of pediatric infectious diseases at Louisiana State University Health Shreveport.
Some public health officials, including Alaska’s chief medical officer, Dr. Anne Zink, questioned whether the military should be using scarce shots for prevention.
“We should ask if that’s the best use,” she said.
Using antibiotics to prevent streptococcal outbreaks is a well-established, evidence-based public health practice that’s also used by other branches of the armed services, said Lt. Col. Randy Ready, a public affairs officer with the Army’s Initial Military Training center. “The Army continues to work with the CDC and the entire medical community in regards to public health while also taking into account the unique missions and training environments our Soldiers face,” including basic training, Ready said in a written statement.
The government isn’t stockpiling syphilis drugs.
In rare instances, the federal government has created stockpiles of drugs considered key to public health. In 2018, confronting shortages of various drugs to treat tuberculosis, the CDC created a small stockpile of them. And the federal Administration for Strategic Preparedness and Response keeps a national stockpile of supplies necessary for public health emergencies, including vaccines, medical supplies and antidotes needed in case of a chemical warfare attack.
In November, the Biden administration announced it was creating a new syphilis task force. When asked why the federal government doesn’t stockpile syphilis treatments, Adm. Rachel Levine, the HHS official who leads the task force, said officials don’t routinely stockpile drugs, because they have expiration dates.
In a written statement, an HHS spokesperson said that Bicillin has a shelf life of two years and that the Strategic National Stockpile “does not deploy products that are commercially available.” In general, the spokesperson wrote, stockpiles are most effective before a national shortage begins and can’t overcome the problems of limited suppliers or fragile supply chains. “There is also a risk that stockpiles can exacerbate shortages, particularly when supply is already low, by removing drugs from circulation that would have otherwise been available,” the spokesperson wrote.
Stephanie Pang, a senior director with the coalition of STD directors, said that given the critical role of this drug and the severe access concerns, she thinks a stockpile is necessary. “I don’t have another solution that actually gets drugs to patients,” Pang said.
The government could declare a federal emergency.
Some public health officials say the federal government needs to treat the syphilis crisis the way it did Ebola or monkeypox.
Declare a federal emergency, said Dr. Michael Dube, an infectious disease specialist for more than 30 years. That would free up money for more public health staff and fund more creative approaches that could lead to a long-term solution to the near-constant shortages, he said. “I’d hate to have to wait for some horrible anecdotes to get out there in order to get the public’s and the policymakers’ minds on it,” said Dube, who oversees medical care for AIDS Healthcare Foundation wellness clinics across the country.
Citing an alarming surge in syphilis cases, the Great Plains Tribes wrote to the HHS secretary last week asking that the agency declare a public health emergency in their areas. In the request, they asked HHS to work globally to find adequate syphilis treatment and send the needed medicine to the Great Plains region.
During the 2014 outbreak of Ebola in West Africa, Congress gave hundreds of millions of dollars to HHS to help develop new rapid tests and vaccines. Facing a global outbreak of monkeypox in 2022, a White House task force deployed more than a million vaccines, regularly briefed the public and sent extra resources to Pride parades and other places where people at risk were gathered.
Levine, leader of the federal syphilis task force, countered that declaring an emergency wouldn’t make much of a difference. The government, she said, already has a “dramatic and coordinated response” involving several agencies.
The FDA recently approved an emergency import of a similar syphilis treatment made by a French manufacturer that had plenty on hand. According to the company, Provepharm, the imported shots are enough to cover approximately one or two months of typical use by all people in the U.S. (The FDA would not say how many doses Provepharm sent, and the company said it was not allowed to reveal that number under the federal rules governing such emergency imports.)
Clinics applaud that development. But many of them can’t afford the imported shots.
The government could do more to rein in the cost.
Clinics and hospitals that primarily serve low-income patients often qualify for a federal program that allows them to purchase drugs at steeply discounted prices. Pharmaceutical companies that want Medicaid to cover their outpatient drugs must participate in the program.
One factor in determining the discount price is whether a pharmaceutical company has raised the price of a drug by more than the rate of inflation. Because Pfizer has hiked the price of its Bicillin shots significantly over the years, the government requires that it be sold to qualifying clinics for just pennies a dose. Otherwise, a single Pfizer shot can retail for upwards of $500. The French shots are comparable in retail price and not eligible for the discount program.
Several clinic directors also said they worried that drug distributors were reserving the limited supply of the Pfizer shot for organizations that could pay full price. For several days in January, for example, the website of Henry Schein, a medical supplier, showed doses of the shot available at full price, while doses at the penny pricing were out of stock, according to screenshots shared with ProPublica. When asked whether it was only selling shots at full price, a spokesperson for Henry Schein did not respond to the question.
Local health departments that qualify for the discount program told ProPublica they’ve had to pay full price at other distributors, because it was the only stock available.
The Health Resources and Services Administration, the federal agency that regulates the discount program, said that a drug manufacturer is ultimately responsible for ensuring that when supplies are available, they are available at the discounted price. When asked about this, Pfizer said that it has “one inventory that is distributed to our trade partners” and that hospitals and clinics that qualify for the discount program are “responsible for ensuring compliance with the program and orders through the wholesaler accordingly.” The company added, “Pfizer plays no part in this process.”
In October, on Weinberg’s regular search for shots for her Mississippi clinic, she found doses of Bicillin for sale at the discounted price and purchased 40. “The idea that we’re supposed to be hoarding treatment is a horrific compact,” she said. Word got out that the clinic, called Plan A, has some shots, and other clinics began sending pregnant patients there.
The clinic’s supply is dwindling. Weinberg is happy to get the shots to patients who need them. But she’s not sure how much longer her reserve will last — or if she’ll be able to find more when they’re gone.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Women spend more of their money on health care than men. And no, it’s not just about ‘women’s issues’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medicare, Australia’s universal health insurance scheme, guarantees all Australians access to a wide range of health and hospital services at low or no cost.
Although access to the scheme is universal across Australia (regardless of geographic location or socioeconomic status), one analysis suggests women often spend more out-of-pocket on health services than men.
Other research has found men and women spend similar amounts on health care overall, or even that men spend a little more. However, it’s clear women spend a greater proportion of their overall expenditure on health care than men. They’re also more likely to skip or delay medical care due to the cost.
So why do women often spend more of their money on health care, and how can we address this gap?
Elizaveta Galitckaia/Shutterstock Women have more chronic diseases, and access more services
Women are more likely to have a chronic health condition compared to men. They’re also more likely to report having multiple chronic conditions.
While men generally die earlier, women are more likely to spend more of their life living with disease. There are also some conditions which affect women more than men, such as autoimmune conditions (for example, multiple sclerosis and rheumatoid arthritis).
Further, medical treatments can sometimes be less effective for women due to a focus on men in medical research.
These disparities are likely significant in understanding why women access health services more than men.
For example, 88% of women saw a GP in 2021–22 compared to 79% of men.
As the number of GPs offering bulk billing continues to decline, women are likely to need to pay more out-of-pocket, because they see a GP more often.
In 2020–21, 4.3% of women said they had delayed seeing a GP due to cost at least once in the previous 12 months, compared to 2.7% of men.
Data from the Australian Bureau of Statistics has also shown women are more likely to delay or avoid seeing a mental health professional due to cost.
Women are more likely to live with chronic medical conditions than men. Drazen Zigic/Shutterstock Women are also more likely to need prescription medications, owing at least partly to their increased rates of chronic conditions. This adds further out-of-pocket costs. In 2020–21, 62% of women received a prescription, compared to 37% of men.
In the same period, 6.1% of women delayed getting, or did not get prescribed medication because of the cost, compared to 4.9% of men.
Reproductive health conditions
While women are disproportionately affected by chronic health conditions throughout their lifespan, much of the disparity in health-care needs is concentrated between the first period and menopause.
Almost half of women aged over 18 report having experienced chronic pelvic pain in the previous five years. This can be caused by conditions such as endometriosis, dysmenorrhoea (period pain), vulvodynia (vulva pain), and bladder pain.
One in seven women will have a diagnosis of endometriosis by age 49.
Meanwhile, a quarter of all women aged 45–64 report symptoms related to menopause that are significant enough to disrupt their daily life.
All of these conditions can significantly reduce quality of life and increase the need to seek health care, sometimes including surgical treatment.
Of course, conditions like endometriosis don’t just affect women. They also impact trans men, intersex people, and those who are gender diverse.
Diagnosis can be costly
Women often have to wait longer to get a diagnosis for chronic conditions. One preprint study found women wait an average of 134 days (around 4.5 months) longer than men for a diagnosis of a long-term chronic disease.
Delays in diagnosis often result in needing to see more doctors, again increasing the costs.
Despite affecting about as many people as diabetes, it takes an average of between six-and-a-half to eight years to diagnose endometriosis in Australia. This can be attributed to a number of factors including society’s normalisation of women’s pain, poor knowledge about endometriosis among some health professionals, and the lack of affordable, non-invasive methods to accurately diagnose the condition.
There have been recent improvements, with the introduction of Medicare rebates for longer GP consultations of up to 60 minutes. While this is not only for women, this extra time will be valuable in diagnosing and managing complex conditions.
But gender inequality issues still exist in the Medicare Benefits Schedule. For example, both pelvic and breast ultrasound rebates are less than a scan for the scrotum, and no rebate exists for the MRI investigation of a woman’s pelvic pain.
Management can be expensive too
Many chronic conditions, such as endometriosis, which has a wide range of symptoms but no cure, can be very hard to manage. People with endometriosis often use allied health and complementary medicine to help with symptoms.
On average, women are more likely than men to use both complementary therapies and allied health.
While women with chronic conditions can access a chronic disease management plan, which provides Medicare-subsidised visits to a range of allied health services (for example, physiotherapist, psychologist, dietitian), this plan only subsidises five sessions per calendar year. And the reimbursement is usually around 50% or less, so there are still significant out-of-pocket costs.
In the case of chronic pelvic pain, the cost of accessing allied or complementary health services has been found to average A$480.32 across a two-month period (across both those who have a chronic disease management plan and those who don’t).
More spending, less saving
Womens’ health-care needs can also perpetuate financial strain beyond direct health-care costs. For example, women with endometriosis and chronic pelvic pain are often caught in a cycle of needing time off from work to attend medical appointments.
Our preliminary research has shown these repeated requests, combined with the common dismissal of symptoms associated with pelvic pain, means women sometimes face discrimination at work. This can lead to lack of career progression, underemployment, and premature retirement.
More women are prescribed medication than men. PeopleImages.com – Yuri A/Shutterstock Similarly, with 160,000 women entering menopause each year in Australia (and this number expected to increase with population growth), the financial impacts are substantial.
As many as one in four women may either shift to part-time work, take time out of the workforce, or retire early due to menopause, therefore earning less and paying less into their super.
How can we close this gap?
Even though women are more prone to chronic conditions, until relatively recently, much of medical research has been done on men. We’re only now beginning to realise important differences in how men and women experience certain conditions (such as chronic pain).
Investing in women’s health research will be important to improve treatments so women are less burdened by chronic conditions.
In the 2024–25 federal budget, the government committed $160 million towards a women’s health package to tackle gender bias in the health system (including cost disparities), upskill medical professionals, and improve sexual and reproductive care.
While this reform is welcome, continued, long-term investment into women’s health is crucial.
Mike Armour, Associate Professor at NICM Health Research Institute, Western Sydney University; Amelia Mardon, Postdoctoral Research Fellow in Reproductive Health, Western Sydney University; Danielle Howe, PhD Candidate, NICM Health Research Institute, Western Sydney University; Hannah Adler, PhD Candidate, Health Communication and Health Sociology, Griffith University, and Michelle O’Shea, Senior Lecturer, School of Business, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Unfuck Your Brain – by Dr. Faith Harper
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book takes a trauma-informed care approach, which is relatively novel in the mental health field and it’s quickly becoming the industry standard because of its effectiveness.
The basic premise of trauma-informed care is that you had a bad experience (possibly even more than one—what a thought!) and that things that remind you of that will tend to prompt reactivity from you in a way that probably isn’t healthy. By identifying each part of that process, we can then interrupt it, much like we might with CBT (the main difference being that CBT, for all its effectiveness, tends to assume that the things that are bothering you are not true, while TIC acknowledges that they might well be, and that especially historically, they probably were).
A word of warning: if something that triggers a trauma-based reactivity response in you is people swearing, then this book will either cure you by exposure therapy or leave you a nervous wreck, because it’s not just the title; Dr. Harper barely gets through a sentence without swearing. It’s a lot, even by this (European) reviewer’s standards (we’re a lot more relaxed about swearing over here, than people tend to be in America).
On the other hand, something that Dr. Harper excels at is actually explaining stuff very well. So while it sometimes seems like she’s “trying too hard” style-wise in terms of being “not like other therapists”, in her defence she’s nevertheless a very good writer; she knows her stuff, and knows how to communicate it clearly.
Bottom line: if you don’t mind a writer who swears more than 99% of soldiers, then this book is an excellent how-to guide for self-administered trauma-informed care.
Click here to check out Unfuck Your Brain, and indeed unfuck it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: