When Carbs, Proteins, & Fats Switch Metabolic Roles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Strange Things Happening In The Islets Of Langerhans
It is generally known and widely accepted that carbs have the biggest effect on blood sugar levels (and thus insulin response), fats less so, and protein least of all.
And yet, there was a groundbreaking study published yesterday which found:
❝Glucose is the well-known driver of insulin, but we were surprised to see such high variability, with some individuals showing a strong response to proteins, and others to fats, which had never been characterized before.
Insulin plays a major role in human health, in everything from diabetes, where it is too low*, to obesity, weight gain and even some forms of cancer, where it is too high.
These findings lay the groundwork for personalized nutrition that could transform how we treat and manage a range of conditions.❞
*saying ”too low” here is potentially misleading without clarification; yes, Type 1 Diabetics will have too little [endogenous] insulin (because the pancreas is at war with itself and thus isn’t producing useful quantities of insulin, if any). Type 2, however, is more a case of acquired insulin insensitivity, because of having too much at once too often, thus the body stops listening to it, “boy who cried wolf”-style, and the pancreas also starts to get fatigued from producing so much insulin that’s often getting ignored, and does eventually produce less and less while needing more and more insulin to get the same response, so it can be legitimately said “there’s not enough”, but that’s more of a subjective outcome than an objective cause.
Back to the study itself, though…
What they found, and how they found it
Researchers took pancreatic islets from 140 heterogenous donors (varied in age and sex; ostensibly mostly non-diabetic donors, but they acknowledge type 2 diabetes could potentially have gone undiagnosed in some donors*) and tested cell cultures from each with various carbs, proteins, and fats.
They found the expected results in most of the cases, but around 9% responded more strongly to the fats than the carbs (even more strongly than to glucose specifically), and even more surprisingly 8% responded more strongly to the proteins.
*there were also some known type 2 diabetics amongst the donors; as expected, those had a poor insulin response to glucose, but their insulin response to proteins and fats were largely unaffected.
What this means
While this is, in essence, a pilot study (the researchers called for larger and more varied studies, as well as in vivo human studies), the implications so far are important:
It appears that, for a minority of people, a lot of (generally considered very good) antidiabetic advice may not be working in the way previously understood. They’re going to (for example) put fat on their carbs to reduce the blood sugar spike, which will technically still work, but the insulin response is going to be briefly spiked anyway, because of the fats, which very insulin response is what will lower the blood sugars.
In practical terms, there’s not a lot we can do about this at home just yet—even continuous glucose monitors won’t tell us precisely, because they’re monitoring glucose, not the insulin response. We could probably measure everything and do some math and work out what our insulin response has been like based on the pace of change in blood sugar levels (which won’t decrease without insulin to allow such), but even that is at best grounds for a hypothesis for now.
Hopefully, more publicly-available tests will be developed soon, enabling us all to know our “insulin response type” per the proteome predictors discovered in this study, rather than having to just blindly bet on it being “normal”.
Ironically, this very response may have hidden itself for a while—if taking fats raised insulin response without raising blood sugar levels, then if blood sugar levels are the only thing being measured, all we’ll see is “took fats at dinner; blood sugars returned to normal more quickly than when taking carbs without fats”.
You can read the study in full here:
Proteomic predictors of individualized nutrient-specific insulin secretion in health and disease
Want to know more about blood sugar management?
You might like to catch up on:
- 10 Ways To Balance Your Blood Sugars
- Track Your Blood Sugars For Better Personalized Health
- How To Turn Back The Clock On Insulin Resistance
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Macadamia Nuts vs Brazil Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing macadamia nuts to Brazil nuts, we picked the Brazil nuts.
Why?
They’re a lot more nutrient dense! But watch out…
First, to do due diligence in terms of macros: Brazil nuts have twice as much protein and less fat, as well as being a little higher in fiber and slightly lower in carbs.
In terms of vitamins, Brazil nuts are about 10x higher in vitamin E, while macadamias are somewhat higher in several B-vitamins.
The category of minerals is where it gets interesting. Macadamia nuts are a little higher in iron and considerably higher in Manganese. But… Brazil nuts are a lot higher in calcium, copper, magnesium, phosphorus, potassium, selenium, and zinc.
About that selenium… Specifically, it’s more than 5,000x higher, and a cup of Brazil nuts would give nearly 10,000x the recommended daily amount of selenium. Now, selenium is an essential mineral (needed for thyroid hormone production, for example), and at the RDA it’s good for good health. Your hair will be luscious and shiny. However, go much above that, and selenium toxicity becomes a thing, you may get sick, and it can cause your (luscious and shiny) hair to fall out. For this reason, it’s recommended to eat no more than 3–4 Brazil nuts per day.
In short… Brazil nuts are much more nutrient dense in general, and thus come out on top here. But, they’re so nutrient dense in the case of selenium, that careful moderation is advised.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
-
Fast Diet, Fast Exercise, Fast Improvements
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Diet & Exercise, Optimized
This is Dr. Michael Mosley. He originally trained in medicine with the intention of becoming a psychiatrist, but he grew disillusioned with psychiatry as it was practised, and ended up pivoting completely into being a health educator, in which field he won the British Medical Association’s Medical Journalist of the Year Award.
He also died under tragic circumstances very recently (he and his wife were vacationing in Greece, he went missing while out for a short walk on the 5th of June, appears to have got lost, and his body was found 100 yards from a restaurant on the 9th). All strength and comfort to his family; we offer our small tribute here today in his honor.
The “weekend warrior” of fasting
Dr. Mosley was an enjoyer (and proponent) of intermittent fasting, which we’ve written about before:
Fasting Without Crashing? We Sort The Science From The Hype
However, while most attention is generally given to the 16:8 method of intermittent fasting (fast for 16 hours, eat during an 8 hour window, repeat), Dr. Mosley preferred the 5:2 method (which generally means: eat at will for 5 days, then eat a reduced calorie diet for the other 2 days).
Specifically, he advocated putting that cap at 800 kcal for each of the weekend days (doesn’t have to be specifically the weekend).
He also tweaked the “eat at will for 5 days” part, to “eat as much as you like of a low-carb Mediterranean diet for 5 days”:
❝The “New 5:2” approach involves restricting calories to 800 on fasting days, then eating a healthy lower carb, Mediterranean-style diet for the rest of the week.
The beauty of intermittent fasting means that as your insulin sensitivity returns, you will feel fuller for longer on smaller portions. This is why, on non-fasting days, you do not have to count calories, just eat sensible portions. By maintaining a Mediterranean-style diet, you will consume all of the healthy fats, protein, fibre and fresh plant-based food that your body needs.❞
Read more: The Fast 800 | The New 5:2
And about that tweaked Mediterranean Diet? You might also want to check out:
Four Ways To Upgrade The Mediterranean Diet
Knowledge is power
Dr. Mosley encouraged the use of genotyping tests for personal health, not just to know about risk factors, but also to know about things such as, for example, whether you have the gene that makes you unable to gain significant improvements in aerobic fitness by following endurance training programs:
The Real Benefit Of Genetic Testing
On which note, he himself was not a fan of exercise, but recognised its importance, and instead sought to minimize the amount of exercise he needed to do, by practising High Intensity Interval Training. We reviewed a book of his (teamed up with a sports scientist) not long back; here it is:
Fast Exercise: The Simple Secret of High Intensity Training – by Dr. Michael Mosley & Peta Bee
You can also read our own article on the topic, here:
How To Do HIIT (Without Wrecking Your Body)
Just One Thing…
As well as his many educational TV shows, Dr. Mosley was also known for his radio show, “Just One Thing”, and a little while ago we reviewed his book, effectively a compilation of these:
Just One Thing: How Simple Changes Can Transform Your Life – by Dr. Michael Mosley
Enjoy!
Share This Post
-
Captivate – by Vanessa van Edwards
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book isn’t just for one area of human interactions. It covers everything from the boardroom to the bedroom (not necessarily a progression with the same person!), business associates, friends, partners, kids, and more.
She presents information in a layered manner, covering for example, chapter-by-chapter:
- the first five minutes
- the first five hours
- the first five days
She also covers such things as:
- starting conversations in a way that makes you memorable (without making it weird!)
- the importance of really listening (and how to do that)
- collecting like-minded people appropriately
- introducing other people! Because a) it’s not all about you, but also b) you’re the person who knows everybody now
- where to stand at parties / networking events!
- dating and early-days dating messages
- reading the room, reading the people
All in all, a great resource for anyone who wants to make (and maintain!) meaningful relationships with those around you.
Share This Post
Related Posts
-
Foam Rolling – by Karina Inkster
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever bought a foam roller only to place it under your lower back once and then put it somewhere for safekeeping and never use it again, this book will help fix that.
Karina Inkster (what a cool name) is a personal trainer, and the book also features tips and advice from physiotherapists and sports medicine specialist doctors too, so all bases are well and truly covered.
This is not, in case you’re wondering, a book that could have been a pamphlet, with photos of the exercises and one-liner explanation and that’s it. Rather, Inkster takes us through the anatomy and physiology of what’s going on, so that we can actually use this thing correctly and get actual noticeable improvements to our health from it—as promised in the subtitle’s mention of “for massage, injury prevention, and core strength”. To be clear, a lot of it is also about soft tissue mobilization, and keeping our fascia healthy (an oft-underestimated aspect of general mobility).
We would mention that since the photos are pleasantly colorful (like those on the cover) and this adds to the clarity, we’d recommend springing for the (quite inexpensive) physical copy, rather than a Kindle edition (if your e-reader is a monochrome e-ink device like this reviewer’s, anyway).
Bottom line: this book will enable your foam roller to make a difference to your life.
Click here to check out Foam Rolling, and get rolling (correctly)!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
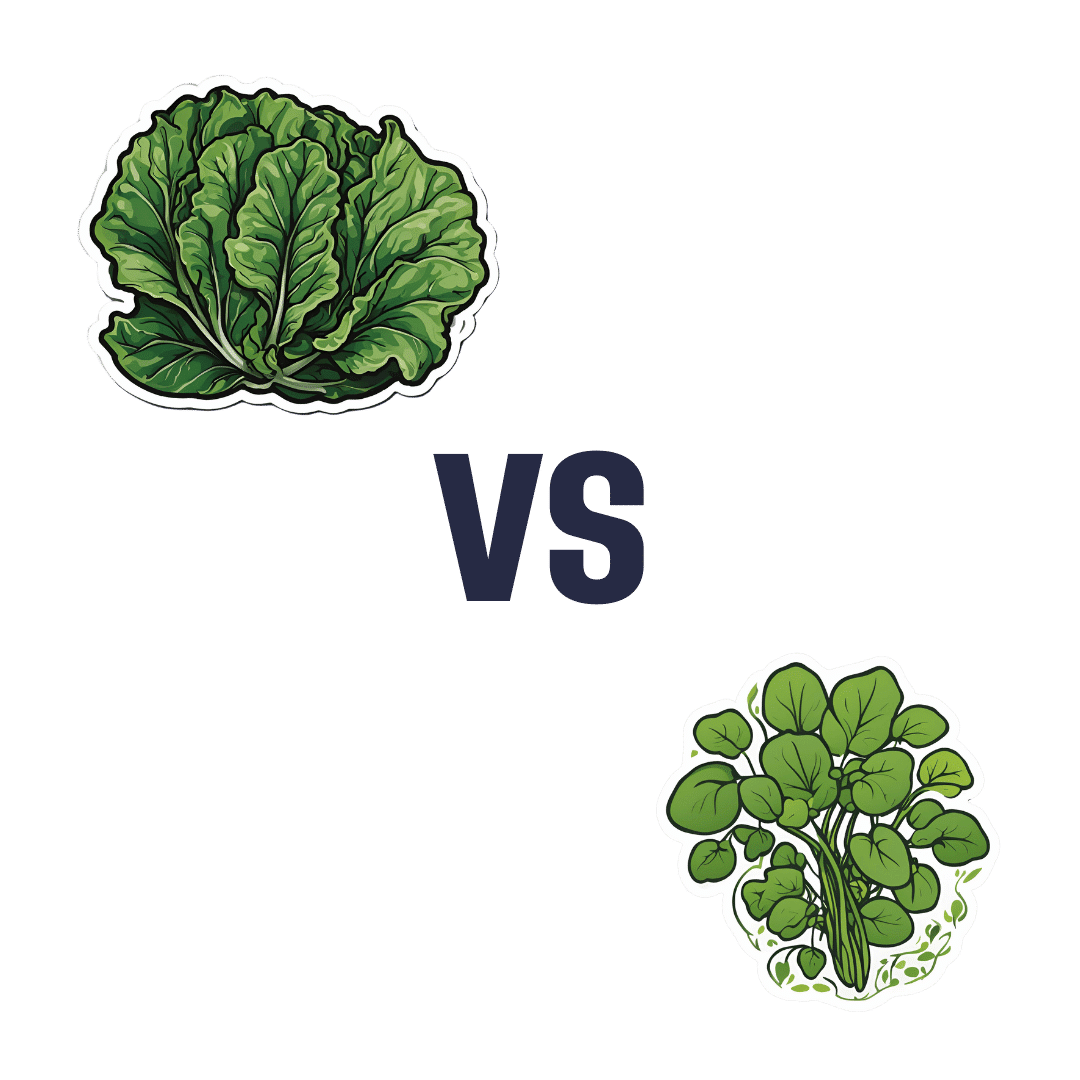
Collard Greens vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing collard greens to watercress, we picked the collard greens.
Why?
It was close! But…
In terms of macros, collard greens have 8x the fiber, 4x the carbs, and slightly more protein. The fiber-to-carbs ratio also gives collard greens the lower glycemic index, although honestly, nobody is getting metabolic disease from eating watercress. Still, by the numbers it’s a clear win for collard greens, and especially 8x the fiber is not to be undervalued!
When it comes to vitamins, things were much more even; collard greens have more of vitamins A, B3, B9, K, and choline, while watercress has more of vitamins B1, B2, B5, C, and E. They’re tied on vitamin B6, so that makes a 5.5:5.5 tie overall. Looking for a tiebreaker, collard greens’ margins of difference are greater, so we could call this a tie or the narrowest of wins for collard greens ion this category.
In the category of minerals, collard greens have more calcium, copper, iron, manganese, and zinc, while watercress has more copper, phosphorus, potassium, and selenium. They’re tied on magnesium. This time the margins of difference are also comparable, so there’s really no tiebreaker available for this one. Thus, an absolute tie on minerals.
Looking at polyphenols, watercress has slightly more, with the main contender being 4mg/100g quercetin.
Adding up the sections results in either a tie or a slight for collard greens based on the tiebreaker in the vitamins category.
We can also put the two clear wins (one for collard greens and one for watercress), and say that in our opinion, collard greens’ 4g/100g fiber beats watercress’s 4mg/100g quercetin.
Quercetin is great and all, but:
- if you buy a quercetin supplement like this one on Amazon it’s 1000mg capsules, so how critical is watercress’s 4mg, really? Yes, getting it from food is better, but it’s not 25,000% better.
- no doctor that we know of is saying “you need more quercetin or you’re going to die”, but they do say “you need more fiber or you’re going to die”
- indeed, the WHO passionately proclaims that 95% of people in the US especially desperately need to eat more fiber, whereas there is no similar giant public health campaign begging people to have 4mg more of quercetin
…so we’ll say that’s another tiebreaker in favor of collard greens.
In short: collard greens scrape a win based on several tiebreakers, but watercress was a very close contender indeed!
Of course, by all means enjoy either or (ideally!) both; diversity is good.
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce Knee Pain After Sitting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sitting is bad for the health, and doubly so if you have arthritis, as a lack of regular movement can cause joints to “seize up”. So, what to do about it if you have to sit for an extended time?
Dr. Alyssa Kuhn, arthritis specialist, explains:
Movement remains key
The trick is to continue periodically moving, notwithstanding that you may need to remain seated. So…
- Heel slides
- Straighten and bend your leg by sliding or lifting your heel.
- Promotes blood flow and reduces fluid buildup in the knee.
- Helps lubricate the joint, making standing up easier.
- Heel lifts
- Lift your heels up and down while keeping feet on the ground.
- This one’s ideal for tight spaces, such as when riding in a car or airplane.
- Improves blood circulation and can reduce ankle swelling and leg heaviness.
Do 20–30 repetitions every now and again, to keep your joints moving.
Note: if you are a wheelchair user whose legs lack the strength and/or motor function to do this, in this case it’s the movement of the leg that counts, not where that movement originated from. So, if you use one hand to lift your leg slightly and the other to push it like a swing, that will also be sufficient to give the joint the periodic movement it needs.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Stand Up For Your Health (Or Don’t) ← our main feature on this also includes more things you can do if you must sit, to make sitting less bad!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Heel slides