Speedy Easy Ratatouille
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest contributing factors to unhealthy eating? The convenience factor. To eat well, it seems, one must have at least two of the following: money, time, and skill. So today we have a health dish that’s cheap, quick, and easy!
(You won’t need a rat in a hat to help you with this one)
You will need
- 3 ripe tomatoes, roughly chopped
- 2 zucchini, halved and chopped into thick batons
- 2 portobello mushrooms, sliced into ½” slices
- 1 large red pepper, cut into thick chunks
- 3 tbsp extra virgin olive oil
- 2 tbsp finely chopped parsley
- 2 tsp garlic paste
- 2 tsp thyme leaves, destalked
- 1 tsp rosemary leaves, destalked
- 1 tsp red chili flakes
- 1 tsp black pepper
- Optional: 1 tsp MSG, or 1 tsp low sodium salt (the MSG is the healthier option as it contains less sodium than even low sodium salt)
- Optional: other vegetables, chopped. Use what’s in your fridge! This is a great way to use up leftovers. Particularly good options include chopped eggplant, chopped red onion, and/or chopped carrot.
Method
(we suggest you read everything at least once before doing anything)
1) Put the olive oil into a sauté pan and set the heat on medium. When hot but smoking, add the mushrooms and any optional vegetables (but not the others from the list yet), and fry for 5 minutes.
Note: if you aren’t pressed for time, then you can diverge from the “speedy” part of this by cooking each of the vegetables separately before combining, which allows each to keep its flavor more distinct.
2) Add the garlic, followed by the zucchini, red pepper, chili flakes, and thyme; stir periodically (you shouldn’t have to stir constantly) for 10 minutes.
3) Add the tomatoes and a cup of water to the pan, along with any MSG/salt. Cover with the lid and allow to simmer for a further 10 minutes.
4) Serve, adding the garnish.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- The Magic Of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we had 3/5 today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
- MSG vs Salt: Sodium Comparison
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cognitive Enhancement Without Drugs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cognitive Enhancement Without Drugs
This is Elizabeth Ricker. She’s a Harvard-and-MIT-trained neuroscientist and researcher, who now runs the “Citizen Science” DIY-neurohacking organization, NeuroEducate.
Sounds fun! What’s it about?
The philosophy that spurs on her research and practice can be summed up as follows:
❝I’m not going to leave my brain up to my doctor or [anyone else]… My brain is my own responsibility, and I’m going to do the best that I can to optimize it❞
Her goal is not just to optimize her own brain though; she wants to make the science accessible to everyone.
What’s this about Citizen Science?
“Citizen Science” is the idea that while there’s definitely an important role in society for career academics, science itself should be accessible to all. And, not just the conclusions, but the process too.
This can take the form of huge experiments, often facilitated these days by apps where we opt-in to allow our health metrics (for example) to be collated with many thousands of others, for science. It can also involve such things as we talked about recently, getting our own raw genetic data and “running the numbers” at home to get far more comprehensive and direct information than the genetic testing company would ever provide us.
For Ricker, her focus is on the neuroscience side of biohacking, thus, neurohacking.
I’m ready to hack my brain! Do I need a drill?
Happily not! Although… Bone drills for the skull are very convenient instruments that make it quite hard to go wrong even with minimal training. The drill bit has a little step/ledge partway down, which means you can only drill through the thickness of the skull itself, before the bone meeting the wider part of the bit stops you from accidentally drilling into the brain. Still, please don’t do this at home.
What you can do at home is a different kind of self-experimentation…
If you want to consider which things are genuinely resulting in cognitive enhancement and which things are not, you need to approach the matter like a scientist. That means going about it in an organized fashion, and recording results.
There are several ways cognitive enhancement can be measured, including:
- Learning and memory
- Executive function
- Emotional regulation
- Creative intelligence
Let’s look at each of them, and what can be done. We don’t have a lot of room here; we’re a newsletter not a book, but we’ll cover one of Ricker’s approaches for each:
Learning and memory
This one’s easy. We’re going to leverage neuroplasticity (neurons that fire together, wire together!) by simple practice, and introduce an extra element to go alongside your recall. Perhaps a scent, or a certain item of clothing. Tell yourself that clinical studies have shown that this will boost your recall. It’s true, but that’s not what’s important; what’s important is that you believe it, and bring the placebo effect to bear on your endeavors.
You can test your memory with word lists, generated randomly by AI, such as this one:
You’ll soon find your memory improving—but don’t take our word for it!
Executive function
Executive function is the aspect of your brain that tells the other parts how to work, when to work, and when to stop working. If you’ve ever spent 30 minutes thinking “I need to get up” but you were stuck in scrolling social media, that was executive dysfunction.
This can be trained using the Stroop Color and Word Test, which shows you words, specifically the names of colors, which will themselves be colored, but not necessarily in the color the word pertains to. So for example, you might be shown the word “red”, colored green. Your task is to declare either the color of the word only, ignoring the word itself, or the meaning of the word only, ignoring its appearance. It can be quite challenging, but you’ll get better quite quickly:
The Stroop Test: Online Version
Emotional Regulation
This is the ability to not blow up angrily at the person with whom you need to be diplomatic, or to refrain from laughing when you thought of something funny in a sombre situation.
It’s an important part of cognitive function, and success or failure can have quite far-reaching consequences in life. And, it can be trained too.
There’s no online widget for this one, but: when and if you’re in a position to safely* do so, think about something that normally triggers a strong unwanted emotional reaction. It doesn’t have to be something life-shattering, but just something that you feel in some way bad about. Hold this in your mind, sit with it, and practice mindfulness. The idea is to be able to hold the unpleasant idea in your mind, without becoming reactive to it, or escaping to more pleasant distractions. Build this up.
*if you perchance have PTSD, C-PTSD, or an emotional regulation disorder, you might want to talk this one through with a qualified professional first.
Creative Intelligence
Another important cognitive skill, and again, one that can be cultivated and grown.
The trick here is volume. A good, repeatable test is to think of a common object (e.g. a rock, a towel, a banana) and, within a time constraint (such as 15 minutes) list how many uses you can think of for that item.
Writer’s storytime: once upon a time, I was sorting through an inventory of medical equipment with a colleague, and suggested throwing out our old arterial clamps, as we had newer, better ones—in abundance. My colleague didn’t want to part with them, so I challenged him “Give me one use for these, something we could in some possible world use them for that the new clamps don’t do better, and we’ll keep them”. He said “Thumbscrews”, and I threw my hands up in defeat, saying “Fine!”, as he had technically fulfilled my condition.
What’s the hack to improve this one? Just more volume. Creativity, as it turns out, isn’t something we can expend—like a muscle, it grows the more we use it. And because the above test is repeatable (with different objects), you can track your progress.
And if you feel like using your grown creative muscle to write/paint/compose/etc your magnum opus, great! Or if you just want to apply it to the problem-solving of everyday life, also great!
In summary…
Our brain is a wonderful organ with many functions. Society expects us to lose these as we get older, but the simple, scientific truth is that we can not only maintain our cognitive function, but also enhance and grow it as we go.
Want to know more from today’s featured expert?
You might enjoy her book, “Smarter Tomorrow”, which we reviewed back in March
Share This Post
-
Pain Doesn’t Belong on a Scale of Zero to 10
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Over the past two years, a simple but baffling request has preceded most of my encounters with medical professionals: “Rate your pain on a scale of zero to 10.”
I trained as a physician and have asked patients the very same question thousands of times, so I think hard about how to quantify the sum of the sore hips, the prickly thighs, and the numbing, itchy pain near my left shoulder blade. I pause and then, mostly arbitrarily, choose a number. “Three or four?” I venture, knowing the real answer is long, complicated, and not measurable in this one-dimensional way.
Pain is a squirrely thing. It’s sometimes burning, sometimes drilling, sometimes a deep-in-the-muscles clenching ache. Mine can depend on my mood or how much attention I afford it and can recede nearly entirely if I’m engrossed in a film or a task. Pain can also be disabling enough to cancel vacations, or so overwhelming that it leads people to opioid addiction. Even 10+ pain can be bearable when it’s endured for good reason, like giving birth to a child. But what’s the purpose of the pains I have now, the lingering effects of a head injury?
The concept of reducing these shades of pain to a single number dates to the 1970s. But the zero-to-10 scale is ubiquitous today because of what was called a “pain revolution” in the ’90s, when intense new attention to addressing pain — primarily with opioids — was framed as progress. Doctors today have a fuller understanding of treating pain, as well as the terrible consequences of prescribing opioids so readily. What they are learning only now is how to better measure pain and treat its many forms.
About 30 years ago, physicians who championed the use of opioids gave robust new life to what had been a niche specialty: pain management. They started pushing the idea that pain should be measured at every appointment as a “fifth vital sign.” The American Pain Society went as far as copyrighting the phrase. But unlike the other vital signs — blood pressure, temperature, heart rate, and breathing rate — pain had no objective scale. How to measure the unmeasurable? The society encouraged doctors and nurses to use the zero-to-10 rating system. Around that time, the FDA approved OxyContin, a slow-release opioid painkiller made by Purdue Pharma. The drugmaker itself encouraged doctors to routinely record and treat pain, and aggressively marketed opioids as an obvious solution.
To be fair, in an era when pain was too often ignored or undertreated, the zero-to-10 rating system could be regarded as an advance. Morphine pumps were not available for those cancer patients I saw in the ’80s, even those in agonizing pain from cancer in their bones; doctors regarded pain as an inevitable part of disease. In the emergency room where I practiced in the early ’90s, prescribing even a few opioid pills was a hassle: It required asking the head nurse to unlock a special prescription pad and making a copy for the state agency that tracked prescribing patterns. Regulators (rightly) worried that handing out narcotics would lead to addiction. As a result, some patients in need of relief likely went without.
After pain doctors and opioid manufacturers campaigned for broader use of opioids — claiming that newer forms were not addictive, or much less so than previous incarnations — prescribing the drugs became far easier and were promoted for all kinds of pain, whether from knee arthritis or back problems. As a young doctor joining the “pain revolution,” I probably asked patients thousands of times to rate their pain on a scale of zero to 10 and wrote many scripts each week for pain medication, as monitoring “the fifth vital sign” quickly became routine in the medical system. In time, a zero-to-10 pain measurement became a necessary box to fill in electronic medical records. The Joint Commission on the Accreditation of Healthcare Organizations made regularly assessing pain a prerequisite for medical centers receiving federal health care dollars. Medical groups added treatment of pain to their list of patient rights, and satisfaction with pain treatment became a component of post-visit patient surveys. (A poor showing could mean lower reimbursement from some insurers.)
But this approach to pain management had clear drawbacks. Studies accumulated showing that measuring patients’ pain didn’t result in better pain control. Doctors showed little interest in or didn’t know how to respond to the recorded answer. And patients’ satisfaction with their doctors’ discussion of pain didn’t necessarily mean they got adequate treatment. At the same time, the drugs were fueling the growing opioid epidemic. Research showed that an estimated 3% to 19% of people who received a prescription for pain medication from a doctor developed an addiction.
Doctors who wanted to treat pain had few other options, though. “We had a good sense that these drugs weren’t the only way to manage pain,” Linda Porter, director of the National Institutes of Health’s Office of Pain Policy and Planning, told me. “But we didn’t have a good understanding of the complexity or alternatives.” The enthusiasm for narcotics left many varietals of pain underexplored and undertreated for years. Only in 2018, a year when nearly 50,000 Americans died of an overdose, did Congress start funding a program — the Early Phase Pain Investigation Clinical Network, or EPPIC-Net — designed to explore types of pain and find better solutions. The network connects specialists at 12 academic specialized clinical centers and is meant to jump-start new research in the field and find bespoke solutions for different kinds of pain.
A zero-to-10 scale may make sense in certain situations, such as when a nurse uses it to adjust a medication dose for a patient hospitalized after surgery or an accident. And researchers and pain specialists have tried to create better rating tools — dozens, in fact, none of which was adequate to capture pain’s complexity, a European panel of experts concluded. The Veterans Health Administration, for instance, created one that had supplemental questions and visual prompts: A rating of 5 correlated with a frown and a pain level that “interrupts some activities.” The survey took much longer to administer and produced results that were no better than the zero-to-10 system. By the 2010s, many medical organizations, including the American Medical Association and the American Academy of Family Physicians, were rejecting not just the zero-to-10 scale but the entire notion that pain could be meaningfully self-reported numerically by a patient.
In the years that opioids had dominated pain remedies, a few drugs — such as gabapentin and pregabalin for neuropathy, and lidocaine patches and creams for musculoskeletal aches — had become available. “There was a growing awareness of the incredible complexity of pain — that you would have to find the right drugs for the right patients,” Rebecca Hommer, EPPIC-Net’s interim director, told me. Researchers are now looking for biomarkers associated with different kinds of pain so that drug studies can use more objective measures to assess the medications’ effect. A better understanding of the neural pathways and neurotransmitters that create different types of pain could also help researchers design drugs to interrupt and tame them.
Any treatments that come out of this research are unlikely to be blockbusters like opioids; by design, they will be useful to fewer people. That also makes them less appealing prospects to drug companies. So EPPIC-Net is helping small drug companies, academics, and even individual doctors design and conduct early-stage trials to test the safety and efficacy of promising pain-taming molecules. That information will be handed over to drug manufacturers for late-stage trials, all with the aim of getting new drugs approved by the FDA more quickly.
The first EPPIC-Net trials are just getting underway. Finding better treatments will be no easy task, because the nervous system is a largely unexplored universe of molecules, cells, and electronic connections that interact in countless ways. The 2021 Nobel Prize in Physiology or Medicine went to scientists who discovered the mechanisms that allow us to feel the most basic sensations: cold and hot. In comparison, pain is a hydra. A simple number might feel definitive. But it’s not helping anyone make the pain go away.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Hospitals worldwide are short of saline. We can’t just switch to other IV fluids – here’s why
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Last week, the Australian Therapeutic Goods Administration added intravenous (IV) fluids to the growing list of medicines in short supply. The shortage is due to higher-than-expected demand and manufacturing issues.
Two particular IV fluids are affected: saline and compound sodium lactate (also called Hartmann’s solution). Both fluids are made with salts.
There are IV fluids that use other components, such as sugar, rather than salt. But instead of switching patients to those fluids, the government has chosen to approve salt-based solutions by other overseas brands.
So why do IV fluids contain different chemicals? And why can’t they just be interchanged when one runs low?
Pavel Kosolapov/Shutterstock We can’t just inject water into a vein
Drugs are always injected into veins in a water-based solution. But we can’t do this with pure water, we need to add other chemicals. That’s because of a scientific principle called osmosis.
Osmosis occurs when water moves rapidly in and out of the cells in the blood stream, in response to changes to the concentration of chemicals dissolved in the blood plasma. Think salts, sugars, nutrients, drugs and proteins.
Too high a concentration of chemicals and protein in your blood stream leads it to being in a “hypertonic” state, which causes your blood cells to shrink. Not enough chemicals and proteins in your blood stream causes your blood cells to expand. Just the right amount is called “isotonic”.
Mixing the drug with the right amount of chemicals, via an injection or infusion, ensures the concentration inside the syringe or IV bag remains close to isotonic.
Australia is currently short on two salt-based IV fluids. sirnength88/Shutterstock What are the different types of IV fluids?
There are a range of IV fluids available to administer drugs. The two most popular are:
- 0.9% saline, which is an isotonic solution of table salt. This is one of the IV fluids in short supply
- a 5% solution of the sugar glucose/dextrose. This fluid is not in short supply.
There are also IV fluids that combine both saline and glucose, and IV fluids that have other salts:
- Ringer’s solution is an IV fluid which has sodium, potassium and calcium salts
- Plasma-Lyte has different sodium salts, as well as magnesium
- Hartmann’s solution (compound sodium lactate) contains a range of different salts. It is generally used to treat a condition called metabolic acidosis, where patients have increased acid in their blood stream. This is in short supply.
What if you use the wrong solution?
Some drugs are only stable in specific IV fluids, for instance, only in salt-based IV fluids or only in glucose.
Putting a drug into the wrong IV fluid can potentially cause the drug to “crash out” of the solution, meaning patients won’t get the full dose.
Or it could cause the drug to decompose: not only will it not work, but it could also cause serious side effects.
An example of where a drug can be transformed into something toxic is the cancer chemotherapy drug cisplatin. When administered in saline it is safe, but administration in pure glucose can cause life-threatening damage to a patients’ kidneys.
What can hospitals use instead?
The IV fluids in short supply are saline and Hartmann’s solution. They are provided by three approved Australian suppliers: Baxter Healthcare, B.Braun and Fresenius Kabi.
The government’s solution to this is to approve multiple overseas-registered alternative saline brands, which they are allowed to do under current legislation without it going through the normal Australian quality checks and approval process. They will have received approval in their country of manufacture.
The government is taking this approach because it may not be effective or safe to formulate medicines that are meant to be in saline into different IV fluids. And we don’t have sufficient capacity to manufacture saline IV fluids here in Australia.
The Australian Society of Hospital Pharmacists provides guidance to other health staff about what drugs have to go with which IV fluids in their Australian Injectable Drugs Handbook. If there is a shortage of saline or Hartmann’s solution, and shipments of other overseas brands have not arrived, this guidance can be used to select another appropriate IV fluid.
Why don’t we make it locally?
The current shortage of IV fluids is just another example of the problems Australia faces when it is almost completely reliant on its critical medicines from overseas manufacturers.
Fortunately, we have workarounds to address the current shortage. But Australia is likely to face ongoing shortages, not only for IV fluids but for any medicines that we rely on overseas manufacturers to produce. Shortages like this put Australian lives at risk.
In the past both myself, and others, have called for the federal government to develop or back the development of medicines manufacturing in Australia. This could involve manufacturing off-patent medicines with an emphasis on those medicines most used in Australia.
Not only would this create stable, high technology jobs in Australia, it would also contribute to our economy and make us less susceptible to future global drug supply problems.
Nial Wheate, Professor and Director Academic Excellence, Macquarie University and Shoohb Alassadi, Casual academic, pharmaceutical sciences, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Lyme Disease At-A-Glance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Good info as always…was wondering if you have any recommendations for fighting Lyme disease naturally along wDr advice? Dr’s aren’t real keen on alternatives so always interested. Thanks❞
That depends on whether we’re looking at prevention or cure!
Prevention:
- Try not to get bitten by Lyme-disease-carrying ticks. Boots and long socks are your friends. As are long-gauntletted gloves for gardening.
- If you are in a high-risk area and/or engage in high-risk activities, check your body daily.
- This is because it usually takes 36–48 hours of being attached for a tick to cause an infection
- Obviously best if you can get a partner or close friend to help you with this, unless you have mastered some advanced pretzel positions of yoga.
- Contrary to many folk remedies, the safest way to remove a tick is with tweezers (carefully!).
- If you find and remove a tick, or otherwise suspect you have developed symptoms, go to your doctor immediately (not next week; today; time really counts for this).
Cure:
- No. Sorry. Regretfully, antibiotics are the only known effective treatment.
However! As with almost any kind of recovery, getting good rest, including good quality sleep, will hasten things. Also sensible is reducing stress if possible, and anything that could worsen inflammation.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How does cancer spread to other parts of the body?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
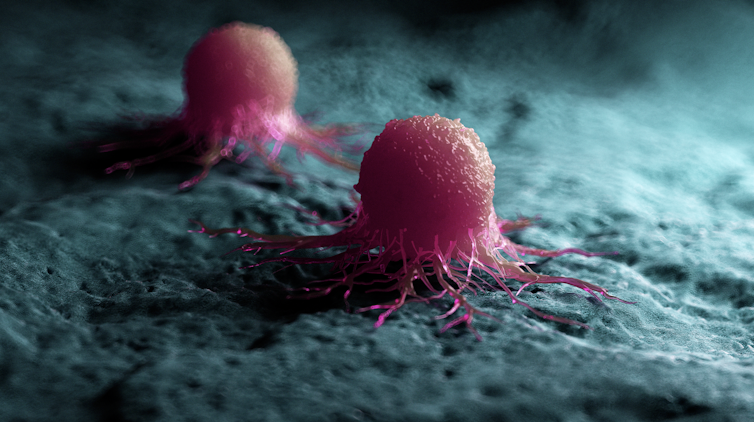
All cancers begin in a single organ or tissue, such as the lungs or skin. When these cancers are confined in their original organ or tissue, they are generally more treatable.
But a cancer that spreads is much more dangerous, as the organs it spreads to may be vital organs. A skin cancer, for example, might spread to the brain.
This new growth makes the cancer much more challenging to treat, as it can be difficult to find all the new tumours. If a cancer can invade different organs or tissues, it can quickly become lethal.
When cancer spreads in this way, it’s called metastasis. Metastasis is responsible for the majority (67%) of cancer deaths.
Cells are supposed to stick to surrounding tissue
Our bodies are made up of trillions of tiny cells. To keep us healthy, our bodies are constantly replacing old or damaged cells.
Each cell has a specific job and a set of instructions (DNA) that tells it what to do. However, sometimes DNA can get damaged.
This damage might change the instructions. A cell might now multiply uncontrollably, or lose a property known as adherence. This refers to how sticky a cell is, and how well it can cling to other surrounding cells and stay where it’s supposed to be.
If a cancer cell loses its adherence, it can break off from the original tumour and travel through the bloodstream or lymphatic system to almost anywhere. This is how metastasis happens.
Many of these travelling cancer cells will die, but some will settle in a new location and begin to form new cancers.
Some cells settle in a new location.
Scipro/ShutterstockParticular cancers are more likely to metastasise to particular organs that help support their growth. Breast cancers commonly metastasise to the bones, liver, and lungs, while skin cancers like melanomas are more likely to end up in the brain and heart.
Unlike cancers which form in solid organs or tissues, blood cancers like leukaemia already move freely through the bloodstream, but can escape to settle in other organs like the liver or brain.
When do cancers metastasise?
The longer a cancer grows, the more likely it is to metastasise. If not caught early, a patient’s cancer may have metastasised even before it’s initially diagnosed.
Metastasis can also occur after cancer treatment. This happens when cancer cells are dormant during treatment – drugs may not “see” those cells. These invisible cells can remain hidden in the body, only to wake up and begin growing into a new cancer months or even years later.
For patients who already have cancer metastases at diagnosis, identifying the location of the original tumour – called the “primary site” – is important. A cancer that began in the breast but has spread to the liver will probably still behave like a breast cancer, and so will respond best to an anti-breast cancer therapy, and not anti-liver cancer therapy.
As metastases can sometimes grow faster than the original tumour, it’s not always easy to tell which tumour came first. These cancers are called “cancers of unknown primary” and are the 11th most commonly diagnosed cancers in Australia.
One way to improve the treatment of metastatic cancer is to improve our ways of detecting and identifying cancers, to ensure patients receive the most effective drugs for their cancer type.
What increases the chances of metastasis and how can it be prevented?
If left untreated, most cancers will eventually acquire the ability to metastasise.
While there are currently no interventions that specifically prevent metastasis, cancer patients who have their tumours surgically removed may also be given chemotherapy (or other drugs) to try and weed out any hidden cancer cells still floating around.
The best way to prevent metastasis is to diagnose and treat cancers early. Cancer screening initiatives such as Australia’s cervical, bowel, and breast cancer screening programs are excellent ways to detect cancers early and reduce the chances of metastasis.
The best way to prevent cancer spreading is to diagnose and treat them early.
Peakstock/ShutterstockNew screening programs to detect cancers early are being researched for many types of cancer. Some of these are simple: CT scans of the body to look for any potential tumours, such as in England’s new lung cancer screening program.
Using artificial intelligence (AI) to help examine patient scans is also possible, which might identify new patterns that suggest a cancer is present, and improve cancer detection from these programs.
More advanced screening methods are also in development. The United States government’s Cancer Moonshot program is currently funding research into blood tests that could detect many types of cancer at early stages.
One day there might even be a RAT-type test for cancer, like there is for COVID.
Will we be able to prevent metastasis in the future?
Understanding how metastasis occurs allows us to figure out new ways to prevent it. One idea is to target dormant cancer cells and prevent them from waking up.
Directly preventing metastasis with drugs is not yet possible. But there is hope that as research efforts continue to improve cancer therapies, they will also be more effective at treating metastatic cancers.
For now, early detection is the best way to ensure a patient can beat their cancer.
Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, Walter and Eliza Hall Institute and John (Eddie) La Marca, Senior Resarch Officer, Walter and Eliza Hall Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Your Simplest Life – by Lisa Turner
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We probably know how to declutter, and perhaps even do a “unnecessary financial expenditures” audit. So, what does this offer beyond that?
A large portion of this book focuses on keeping our general life in a state of “flow”, and strategies include:
- How to make sure you’re doing the right part of the 80:20 split on a daily basis
- Knowing when to switch tasks, and when not to
- Knowing how to plan time for tasks
- No more reckless optimism, but also without falling foul of Parkinson’s Law (i.e. work expands to fill the time allotted to it)
- Decluttering your head, too!
When it comes to managing life responsibilities in general, Turner is very attuned to generational differences… Including the different challenges faced by each generation, what’s more often expected of us, what we’re used to, and how we probably initially learned to do it (or not).
To this end, a lot of strategies are tailored with variations for each age group. Not often does an author take the time to address each part of their readership like that, and it’s really helpful that she does!
All in all, a great book for simplifying your daily life.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: