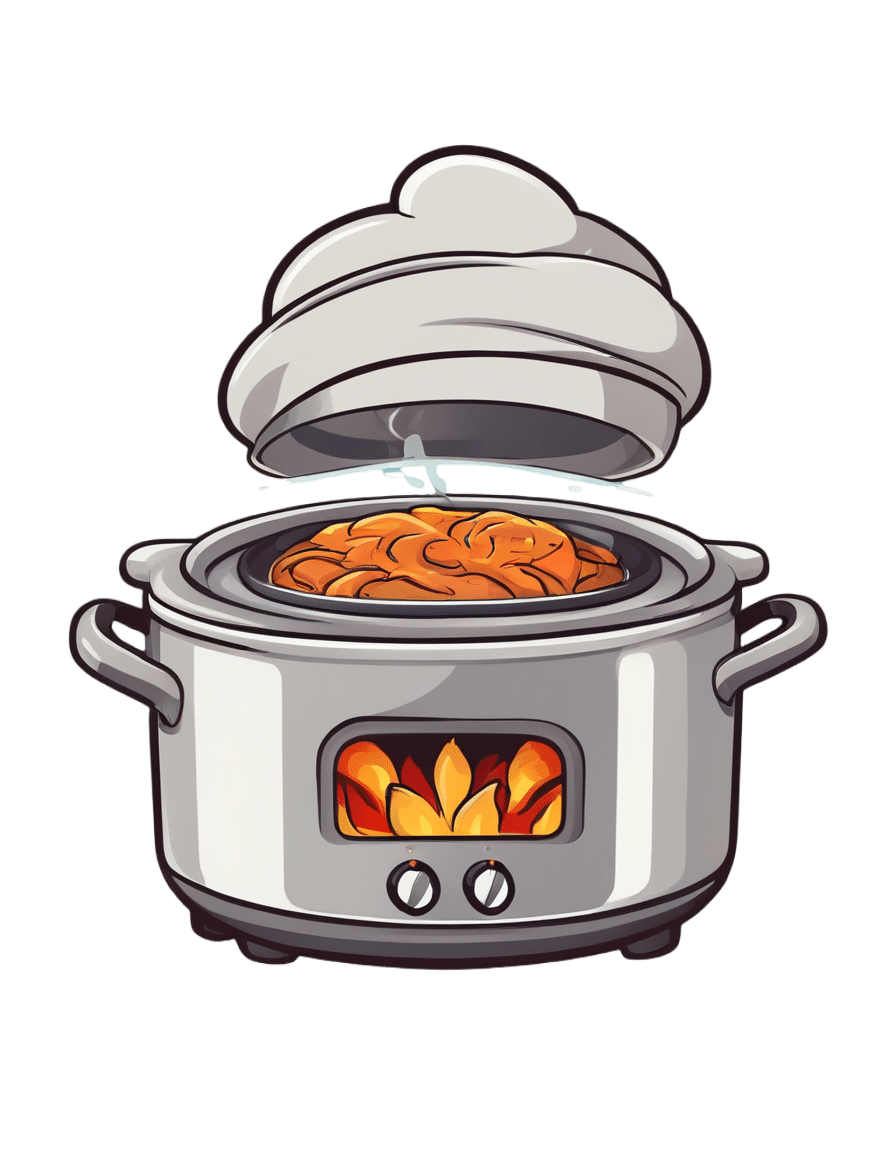
Super-Nutritious Shchi
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today we have a recipe we’ve mentioned before, but now we have standalone recipe pages for recipes, so here we go. The dish of the day is shchi—which is Russian cabbage soup, which sounds terrible, and looks as bad as it sounds. But it tastes delicious, is an incredible comfort food, and is famous (in Russia, at least) for being something one can eat for many days in a row without getting sick of it.
It’s also got an amazing nutritional profile, with vitamins A, B, C, D, as well as lots of calcium, magnesium, and iron (amongst other minerals), and a healthy blend of carbohydrates, proteins, and fats, plus an array of anti-inflammatory phytochemicals, and of course, water.
You will need
- 1 large white cabbage, shredded
- 1 cup red lentils
- ½ lb tomatoes, cut into eighths (as in: halve them, halve the halves, and halve the quarters)
- ½ lb mushrooms sliced (or halved, if they are baby button mushrooms)
- 1 large onion, chopped finely
- 1 tbsp rosemary, chopped finely
- 1 tbsp thyme, chopped finely
- 1 tbsp black pepper, coarse ground
- 1 tsp cumin, ground
- 1 tsp yeast extract
- 1 tsp MSG, or 2 tsp low-sodium salt
- A little parsley for garnishing
- A little fat for cooking; this one’s a tricky and personal decision. Butter is traditional, but would make this recipe impossible to cook without going over the recommended limit for saturated fat. Avocado oil is healthy, relatively neutral in taste, and has a high smoke point for caramelizing the onions. Extra virgin olive oil is also a healthy choice, but not as neutral in flavor and does have a lower smoke point. Coconut oil has far too strong a taste and a low smoke point. Seed oils are very heart-unhealthy. All in all, avocado oil is a respectable choice from all angles except tradition.
Note: with regard to the seasonings, the above is a basic starting guide; feel free to add more per your preference—however, we do not recommend adding more cumin (it’ll overpower it) or more salt (there’s enough sodium in here already).
Method
(we suggest you read everything at least once before doing anything)
1) Cook the lentils until soft (a rice cooker is great for this, but a saucepan is fine); be generous with the water; we are making a soup, after all. Set them aside without draining.
2) Sauté the cabbage, and put it in a big stock pot or similar large pan (not yet on the heat)
3) Fry the mushrooms, and add them to the big pot (still not yet on the heat)
4) Use a stick blender to blend the lentils in the water you cooked them in, and then add to the big pot too.
5) Turn the heat on low, and if necessary, add more water to make it into a rich soup
6) Add the seasonings (rosemary, thyme, cumin, black pepper, yeast extract, MSG-or-salt) and stir well. Keep the temperature on low; you can just let it simmer now because the next step is going to take a while:
7) Caramelize the onion (keep an eye on the big pot, stirring occasionally) and set it aside
8) Fry the tomatoes quickly (we want them cooked, but just barely) and add them to the big pot
9) Serve! The caramelized onion is a garnish, so put a little on top of each bowl of shchi. Add a little parsley too.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- The Magic Of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
- Easily Digestible Vegetarian Protein Sources
- The Bare-Bones Truth About Osteoporosis
- Some Surprising Truths About Hunger And Satiety
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Prevention Is Better Than Cure
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Preventative healthcare is the theme this week:
New year, new risks
The start of a new year is a great time to update adult vaccinations, including the flu shot, any COVID-19 boosters, and vaccines for pneumonia, shingles, and tetanus—when was your last booster, after all? Vaccination recommendations vary by age and health conditions, so do check what’s appropriate in your case. Key vaccines include the pneumonia vaccine for those 65 and older, the shingles vaccine for adults over 50, and the Tdap vaccine every 10 years to protect against tetanus, diphtheria, and pertussis (whooping cough), especially for new parents and grandparents, to protect infants:
Read in full: Why it’s important to update adult vaccinations for a new year
Related: The Truth About Vaccines
The heart-healthiest swap you can do
Based on a large (n=202,863, of which 160,123 women and 42,740 men) dataset, a higher plant-to-animal protein ratio is associated with significantly lower risks of cardiovascular disease (CVD) and coronary artery disease (CAD), with diets lower in meat (especially if lower in red meat) and instead rich in plant-based proteins like legumes, nuts, and whole grains reducing CVD risk by 19% and coronary artery disease risk by 27%. Which is quite considerable.
Substituting even small amounts of animal protein (especially if it’s red meat) with plant protein further enhances heart health:
Read in full: Higher plant-to-animal protein ratio linked to lower risk for CVD, CAD among U.S. adults
Related: Plant vs Animal Protein: Head to Head
Let’s keep pan-resistant superbugs at bay
Researchers want to warn us about the threat of pan-resistant bacteria, which could render all known antibiotics ineffective, leading to a sharp rise in global infection-related deaths.
To be clear, we don’t have anything pan-resistant yet, but antibiotic-resistant superbugs are getting close, and in the long term, are likely to win the evolutionary arms race if we don’t change things to diverge considerably from our current path. Modeling a hypothetical pan-resistant E. coli strain, researchers predicted U.S. sepsis deaths could increase 18- to 46-fold within five years of its emergence.
The study calls for urgent action, including stricter antibiotic stewardship, new drug development, and monitoring technologies, emphasizing that without intervention, the global impact could be catastrophic:
Read in full: A public health emergency is waiting at the bottom of the antibiotic resistance cliff
Related: Stop Sabotaging Your Immune System ← see also (linked therein), 4 ways antibiotics can kill you
Take care!
Share This Post
-
High Histamine Foods To Avoid (And Low Histamine Foods To Eat Instead)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nour Zibdeh is an Integrative and Functional Dietician, and she helps people overcome food intolerances. Today, it’s about getting rid of the underdiagnosed condition that is histamine intolerance, by first eliminating the triggers, and then not getting stuck on the low-histamine diet
The recommendations
High histamine foods to avoid include:
- Alcohol (all types)
- Fermented foods—normally great for the gut, but bad in this case
- That includes most cheeses and yogurts
- Aged, cured, or otherwise preserved meat
- Some plants, e.g. tomato, spinach, eggplant, banana, avocado. Again, normally all great, but not in this case.
Low histamine foods to eat include:
- Fruits and vegetables not mentioned above
- Minimally processed meat and fish, either fresh from the butcher/fishmonger, or frozen (not from the chilled food section of the supermarket), and eaten the same day they were purchased or defrosted, because otherwise histamine builds up over time (and quite quickly)
- Grains, but she recommends skipping gluten, given the high likelihood of a comorbid gluten intolerance. So instead she recommends for example quinoa, oats, rice, buckwheat, millet, etc.
For more about these (and more examples), as well as how to then phase safely off the low histamine diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Food intolerances often gang up on a person (i.e., comorbidity is high), so you might also like to read about:
- Gluten: What’s The Truth?
- Fiber For FODMAP-Avoiders
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Crohn’s, Food Intolerances, & More
Take care!
Share This Post
-
How Not to Age – by Dr. Michael Greger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First things first: it’s a great book, and it’s this reviewer’s favorite of Dr. Greger’s so far (for posterity: it’s just been published and this reviewer has just finished reading the copy she got on pre-order)
Unlike many popular physician authors, Dr. Greger doesn’t rehash a lot of old material, and instead favours prioritizing new material in each work. Where appropriate, he’ll send the reader to other books for more specific information (e.g: you want to know how to avoid premature death? Go read How Not To Die. You want to know how to lose weight? How Not To Diet. Etc).
In the category of new information, he has a lot to offer here. And with over 8,000 references, it’s information, not conjecture. On which note, we recommend the e-book version if that’s possible for you, for three reasons:
- It’s possible to just click the references and be taken straight to the cited paper itself online
- To try to keep the book’s size down, Dr. Greger has linked to other external resources too
- The only negative reviews on Amazon, so far, are people complaining that the print copy’s text is smaller than they’d like
For all its information-density (those 8,000+ references are packed into 600ish pages), the book is very readable even to a lay reader; the author is a very skilled writer.
As for the content, we can’t fit more than a few sentences here so forgive the brevity, but we’ll mention that he covers:
- Slowing 11 pathways of aging
- The optimal anti-aging regimen according to current best science
- Preserving function (specific individual aspects of aging, e.g. hearing, sight, cognitive function, sexual function, hair, bones, etc)
- “Dr. Greger’s Anti-Aging Eight”
In terms of “flavor” of anti-aging science, his approach can be summed up as: diet and lifestyle as foundation; specific supplements and interventions as cornerstones.
Bottom line: this is now the anti-aging book.
Click here to check out How Not To Age, and look after yourself with the best modern science!
Share This Post
Related Posts
-
Staying Alive – by Dr. Jenny Goodman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of “healthy long life” books are science-heavy to the point of being quite challenging to read—they become excellent reference sources, but not exactly “curl up in the armchair” books.
Dr. Goodman writes in a much more reader-friendly fashion, casual yet clear.
She kicks off with season-specific advice. What does that mean? Basically, our bodies need different things at different times of year, and we face different challenges to good health. We may ignore such at our peril!
After a chapter for each of the four seasons (assuming a temperate Northern Hemisphere climate), she goes on to cover the seasons of our life. Once again, our bodies need different things at different times in our life, and we again face different challenges to good health!
There’s plenty of “advice for all seasons”, too. Nutritional dos and don’t, and perennial health hazards to avoid.
As a caveat, she does also hold some unscientific views that may be skipped over. These range from “plant-based diets aren’t sustainable” to “this detox will get rid of heavy metals”. However, the value contained in the rest of the book is more than sufficient to persuade us to overlook those personal quirks.
In particular, she offers very good advice on overcoming cravings (and distinguishing them from genuine nutritional cravings), and taking care of our “trillions of tiny companions” (beneficial gut microbiota) without nurturing Candida and other less helpful gut flora and fauna.
In short, a fine lot of information in a very readable format.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are Brain Chips Safe?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ready For Cyborgization?
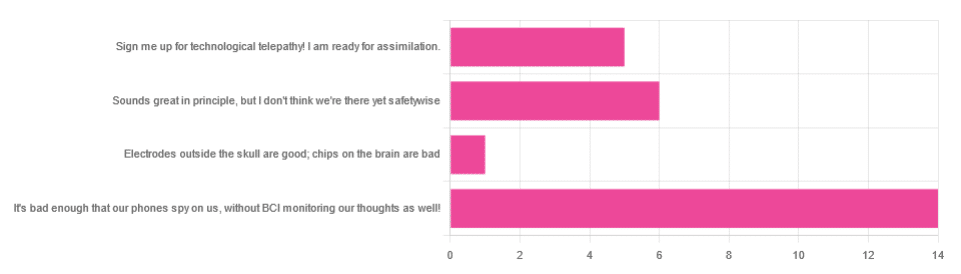
In yesterday’s newsletter, we asked you for your views on Brain-Computer Interfaces (BCIs), such as the Utah Array and Neuralink’s chips on/in brains that allow direct communication between brains and computers, so that (for example) a paralysed person can use a device to communicate, or manipulate a prosthetic limb or two.
We didn’t get as many votes as usual; it’s possible that yesterday’s newsletter ended up in a lot of spam filters due to repeated use of a word in “extra ______ olive oil” in its main feature!
However, of the answers we did get…
- About 54% said “It’s bad enough that our phones spy on us, without BCI monitoring our thoughts as well!”
- About 23% said “Sounds great in principle, but I don’t think we’re there yet safetywise”
- About 19% said “Sign me up for technological telepathy! I am ready for assimilation”
- One (1) person said “Electrode outside the skull are good; chips on the brain are bad”
But what does the science say?
We’re not there yet safetywise: True or False?
True, in our opinion, when it comes to the latest implants, anyway. While it’s very difficult to prove a negative (it could be that everything goes perfectly in human trials), “extraordinary claims require extraordinary evidence”, and so far this seems to be lacking.
The stage before human trials is usually animal trials, starting with small creatures and working up to non-human primates if appropriate, before finally humans.
- Good news: the latest hot-topic BCI device (Neuralink) was tested on animals!
- Bad news: to say it did not go well would be an understatement
The Gruesome Story of How Neuralink’s Monkeys Actually Died
The above is a Wired article, and we tend to go for more objective sources, however we chose this one because it links to very many objective sources, including an open letter from the Physicians’ Committee for Responsible Medicine, which basically confirms everything in the Wired article. There are lots of links to primary (medical and legal) sources, too.
Electrodes outside the skull are good; chips on/in the brain are bad: True or False?
True or False depending on how they’re done. The Utah Array (an older BCI implant, now 20 years old, though it’s been updated many times since) has had a good safety record, after being used by a few dozen people with paralysis to control devices:
How the Utah Array is advancing BCI science
The Utah Array works on the same general principle as Neuralink, but the mechanics of its implementation are very different:
- The Utah Array involves a tiny bundle of microelectrodes (held together by a rigid structure that looks a bit like a nanoscale hairbrush) put in place by a brain surgeon, and that’s that.
- The Neuralink has a dynamic web of electrodes, implanted by a little robot that acts like a tiny sewing machine to implant many polymer threads, each containing its own a bunch of electrodes.
In theory, the latter is much more advanced. In practice, so far, the former has a much better safety record.
I am right to be a little worried about giving companies access to my brain: True or False?
True or False, depending on the nature of your concern.
For privacy: current BCI devices have quite simple switches operated consciously by the user. So while technically any such device that then runs its data through Bluetooth or WiFi could be hacked, this risk is no greater than using a wireless mouse and/or keyboard, because it has access to about the same amount of information.
For safety: yes, probably there is cause to be worried. Likely the first waves of commercial users of any given BCI device will be severely disabled people who are more likely to waive their rights in the hope of a life-changing assistance device, and likely some of those will suffer if things go wrong.
Which on the one hand, is their gamble to make. And on the other hand, makes rushing to human trials, for companies that do that, a little more predatory.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why We’re Called “10almonds”, And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not affected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
❝Why the name “10 Almonds?” Is this recommended by the Doctor? A daily dosage? And, if so, why? Thanks! Please answer me…I truly want to know!❞
Almonds are very nutritionally dense, and for example 20g of almonds (so, about 20 almonds) would give a 100% daily dose of zinc, amongst other nutrients.
We also do like to think that we give our readers an easily digestible dose of condensed “nutrition” in the form of health information.
However! That’s not actually the reason at all. It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was circulating online! So, calling ourselves 10almonds was a bit of a nod to that story, but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: