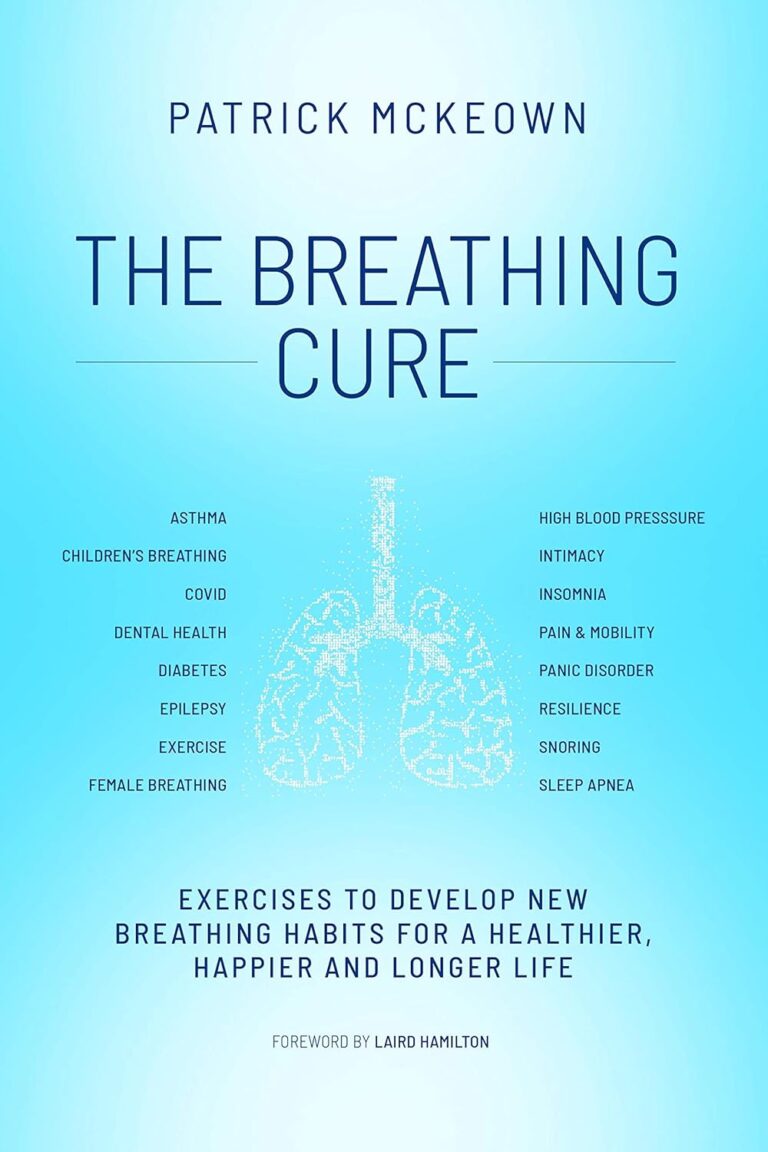
100 No-Equipment Workouts – by Neila Rey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
For those of us who for whatever reason prefer to exercise at home rather than at the gym, we must make do with what exercise equipment we can reasonably install in our homes. This book deals with that from the ground upwards—literally!
If you have a few square meters of floorspace (and a ceiling that’s not too low, for exercises that involve any kind of jumping), then all 100 of these zero-equipment exercises are at-home options.
As to what kinds of exercises they are, they each marked as being one or both of “cardio” and “strength”.
They’re also marked as being of “difficulty level” 1, 2, or 3, so that someone who hasn’t exercised in a while (or hasn’t exercised like this at all), can know where best to start, and how best to progress.
The exercises come with clear explanations in the text, and clear line-drawing illustrations of how to do each exercise. Really, they could not be clearer; this is top quality pragmatism, and reads like a military manual.
Bottom line: whatever your strength and fitness goals, this book can see you well on your way to them (if not outright get you there already in many cases). It’s also an excellent “all-rounder” for full-body workouts.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
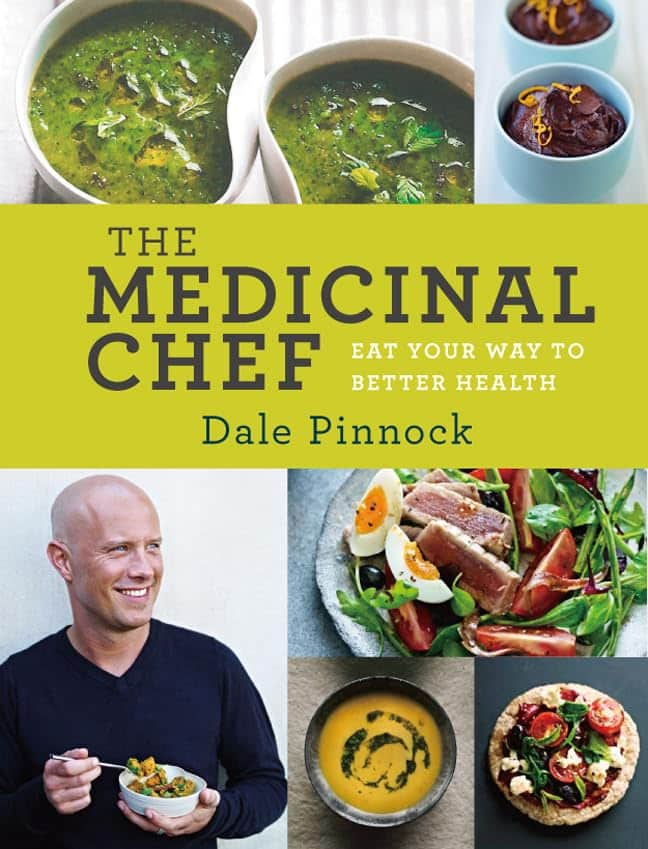
The Medicinal Chef – by Dale Pinnock
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The philosophy here is very much like our own—to borrow from Hippocrates: “let food be thy medicine”. Obviously please do also let medicine be thy medicine if you need it, but the point is that food is a very good starting place for combatting a lot of disease.
To this end, instead of labelling the recipes with such things as “V”, “Ve”, “GF” and suchlike, it assumes we can tell those things from the ingredients lists, and instead labels things per what they are especially good for:
- S: skin
- J: joints & bones
- R: respiratory system
- I: immune system
- M: metabolic health
- N: nervous system and mental health
- H: heart and circulation
- D: digestive system
- U: reproductive & urinary systems
As for the recipes themselves… They’re a lot like the recipes we share here at 10almonds in their healthiness, skill level, and balance of easy-to-find ingredients with the occasional “order it online” items that punch above their weight. In fact, we’ll probably modify some of the recipes for sharing here.
Bottom line: if you’re looking for genuinely healthy recipes that are neither too basic nor too arcane, this book has about 80 of them.
Click here to check out The Medicinal Chef: Healthy Every Day, and be healthy every day!
Share This Post
-
Eat To Beat Chronic Fatigue!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Eat To Beat Chronic Fatigue
Chronic fatigue is on the rise, and it can make life a living Hell. Days blur into one, and you try to take each day as it comes, but sometimes several days gang up on you at once.
You probably know some lifestyle changes that might help—if only you had the energy to implement them.
You’d like to eat well, but you need to…
- Buy the fresh produce (and take a little rest after)
- Put the groceries away (and take a little rest after)
- Wash the vegetables (and take a little rest after)
- Chop the things as necessary (and take a little rest after)
- Cook dinner (and take a little rest after)
…and now you’re too exhausted to eat it.
So, what can be done?
First, avoid things that cause inflammation, as this is a major contributor to chronic fatigue. You might like our previous main feature:
Next up, really do stay hydrated. It’s less about quantity, and more about ubiquity. Hydrate often.
Best is if you always have some (hydrating) drink on the go.
Do experiment with your diet, and/but keep a food journal of what you eat and how you feel 30–60 minutes after eating it. Only make one change at a time, otherwise you won’t know which change made the difference.
Notice what patterns emerge over time, and adjust your ingredients accordingly.
Limit your caffeine intake. We know that sometimes it seems like the only way to get through the day, but you will always crash later, because it was only ever taxing your adrenal system (thus: making you more tired in the long run) and pulling the wool over the eyes of your adenosine receptors (blocking you from feeling how tired you are, but not actually reducing your body’s tiredness).
Put simply, caffeine is the “payday loan” of energy.
Eat more non-starchy vegetables, and enjoy healthy fats. Those healthy fats can come from nuts and seeds, avocado, or fish (not fried, though!).
The non-starchy vegetables will boost your vitamins and fiber while being easy on your beleaguered metabolism, while the healthy fats will perk up your energy levels without spiking insulin like sugars would.
Pay the fatigue tax up front. What this means is… Instead of throwing away vegetables that didn’t get used because it would take too much effort and you just need an easier dinner today, buy ready-chopped vegetables, for example.
And if you buy vegetables frozen, they’re also often not only cheaper, but also (counterintuitively) contain more nutrients.
A note of distinction:
Many more people have chronic fatigue (the symptom: being exhausted all the time) than have chronic fatigue syndrome (the illness: myalgic encephalomyelitis).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
Share This Post
-
Ramadan is almost here. 5 tips to boost your wellbeing and energy levels if you’re fasting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ramadan is one of the most significant months of the Islamic lunar calendar. It marks the time when the Quran was revealed to Prophet Mohammed (peace be upon him).
Almost 2 billion Muslims worldwide observe this month of prayer and reflection, which includes fasting between two prayers, Fajr at dawn and Maghrib at sunset.
Ramadan is about purifying the mind, body and soul, and practising self-restraint. It’s a time for spiritual growth and dedication to God (or Allah in Arabic). Ramadan also brings people together for meals and celebrations, with a focus on helping those less fortunate.
Depending on where you live, Ramadan can mean going 12 to 19 hours without eating or drinking anything, including water.
Our research shows choosing balanced, nutrient-dense foods and drinks can result in better wellbeing and greater energy levels than following your usual diet during Ramadan.
Here’s what to consider if you’re fasting for Ramadan.
Drazen Zigic/Shutterstock Do you have any health issues?
Healthy Muslims are expected to fast during Ramadan once they have reached puberty.
Frail older adults are exempt from fasting, as are pregnant, breastfeeding and menstruating women. Anyone who cannot participate in fasting can make up for the missed fasting days later.
People with chronic illness or mental health may be exempt if fasting poses a risk to their health. If you suffer from chronic illness, such as diabetes, heart disease or kidney problems, and want to fast, consult your GP first.
Fasting can have severe health consequences for people with certain medical conditions and those who rely on prescription medication. Some medications need to be taken at a specific time (and some with food) to be safe and effective.
If you’re not drinking enough water during Ramadan, your body might also handle some medications differently: they may not work as well or cause side effects.
For people who can safely fast, here are five tips to maintain your wellbeing during Ramadan.
1. Plan ahead
In preparation for Ramadan, stock up on essentials. Plan your meals and hydration in advance, to stay on top of your nutritional intake.
Start reducing your caffeine gradually in the week leading to Ramadan, so your body can adjust. This can help prevent or reduce the fasting headaches that many experience at the beginning of Ramadan.
Move your meals gradually towards Suhoor and Iftar times, so your body gets used to the new mealtimes.
Plan your meals ahead of time. Ground Picture/Shutterstock 2. Stay hydrated
Staying hydrated is important during Ramadan. Women should aim to drink 2.1 litres of water or fluids (such as coconut water, clear soups, broths or herbal teas) each day. Men should aim for 2.6 litres.
Limit the intake of sugary or artificially sweetened drinks and enjoy fresh fruit juice only in moderation. Sugary drinks cause a rapid increase in blood sugar levels. The body responds by releasing insulin, causing a drop in blood sugar, which can leave you feeling fatigued, irritable and hungry.
Increase your hydration by including water-rich foods, such as cucumbers and watermelon, in your diet.
3. Get your nutrients early
Before dawn, have a nutrient-rich, slow-digesting meal, along with plenty of water.
Select healthy nutrient-dense food with proteins and fats from lean meats, fish, chickpeas, tofu, nuts and seeds.
Choose whole grain products, a variety of vegetables and fruits, and fermented foods, such as kimchi and pickles, which can support your digestion.
When you prepare your meals, consider grilling, steaming or air frying instead of deep frying.
Stay away from processed foods such as cakes, ice cream, chips and chocolates, as they often lack essential nutrients and are high in sugar, salt and fat. Processed foods also tend to be low in fibre and protein, which are crucial for maintaining a feeling of fullness.
4. Avoid the temptation to overeat in the evening
At sunset, many Muslims come together with family and friends for the fast-breaking evening meal (Iftar). During these occasions, it may be tempting to overindulge in sweets, salty snacks and fatty dishes.
But overeating can strain the digestive system, cause discomfort and disrupt sleep.
Start with something small. Tekkol/Shutterstock Instead, listen to your body’s signals, control your portions, and eat mindfully – this means slowly and without distractions.
Start with something small, such as a date and a glass of water. You may choose to complete the Maghrib prayer before returning for your main meal and more fluids.
5. Keep moving
Finally, try to include some light exercise into your schedule, to maintain your fitness and muscle mass, and promote sleep.
But avoid heavy workouts, sauna and intensive sports while fasting, as these may increase dehydration, which can increase your risk of feeling faint and falling.
Romy Lauche, Deputy Director (Research), National Centre for Naturopathic Medicine, Southern Cross University; Fatima El-Assaad, Senior Research Fellow, Microbiome Research Centre, UNSW Sydney, and Jessica Bayes, Postdoctoral Research Fellow at the National Centre for Naturopathic Medicine, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
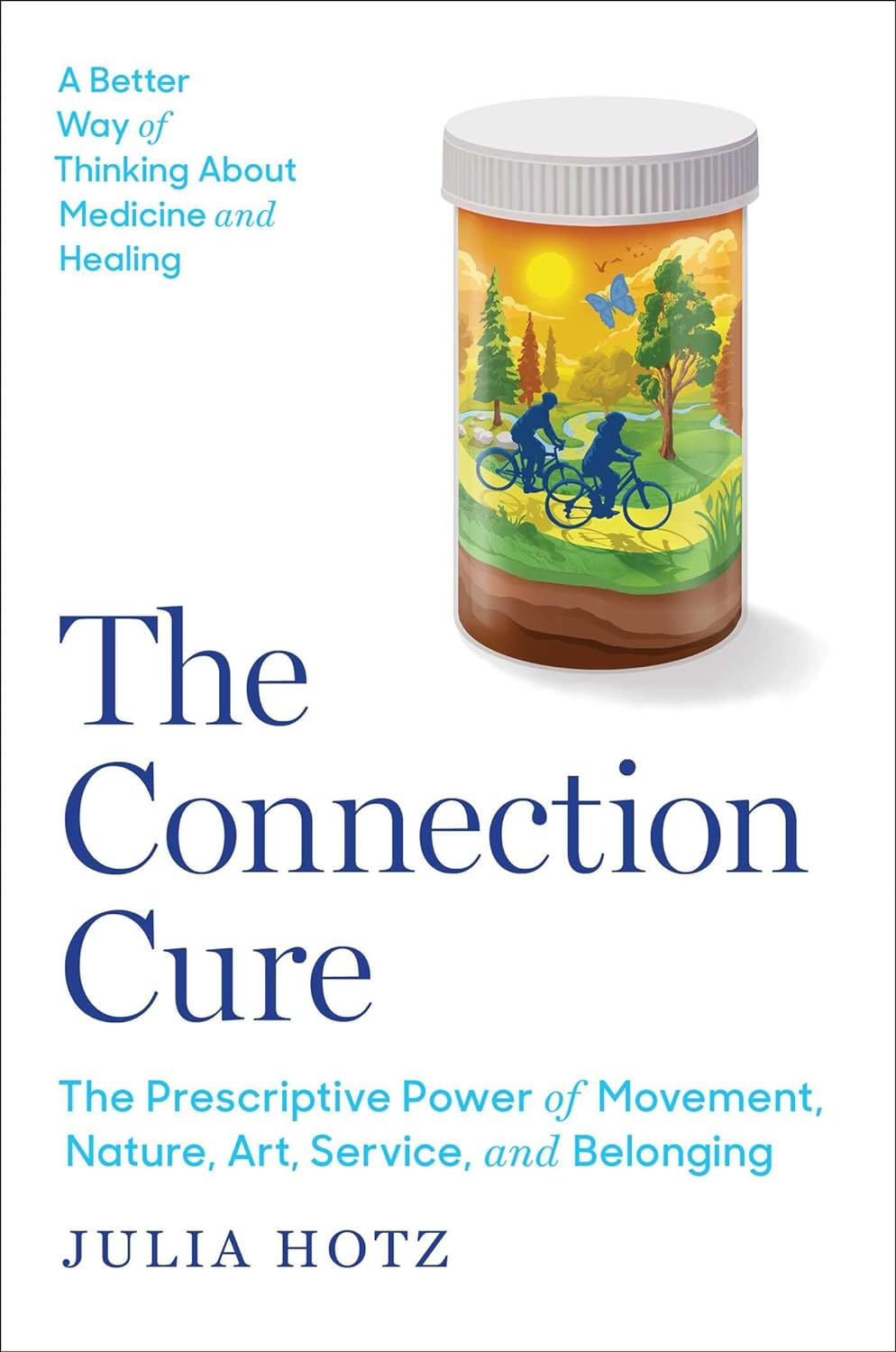
The Connection Cure – by Julia Hotz
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may recognize some of the things in the subtitle as being notable elements of the Blue Zones supercentenarians’ lifestyles, but this book looks at numerous quite diverse countries, and people from many walks of life.
What they have in common—and this is mostly a very person-centered book, relying a lot on case studies, with additional references coming from wider sociological data—is social prescribing.
What is social prescribing? That’s what the author (a journalist by general profession) answers comprehensively here, and it’s about looking at the ways medical problems can often have nonmedical solutions. It doesn’t necessarily mean that walking will cure your cancer or art will cure your diabetes, but it does mean that very often a key part of an unhealthy lifestyle is fundamentally something that can be fixed by one or more of: movement, nature, art, service, and belonging.
She looks at social prescribing in its birthplace (the UK, where cheap solutions that are nevertheless evidence-based are very much prioritized), in big countries like Canada and Australia, in aging countries like Singapore and South Korea, and yes, also in the #1 country of pill prescribing, the US.
The structure of the book is interesting, we first have 5 person-centered chapters addressing each of the social prescribing aspects and how they helped in two example case studies for each one, then 5 country-by-country epidemiological chapters looking at the big picture, then 5 person-centered chapters again, this time looking at personalizing social prescribing for oneself (this section of the book being headed “Social Prescribing For You And Me”), looking at what is going on in one’s life and health, which of the 5 elements might be missing, and what tangible goal-oriented benefits can—according to the evidence—be obtained by tending to what one actually needs in terms of social prescribing.
The style is narrative and journalistic, with very little hard science, but very little that’s wishy-washy either. It is, in short, a pleasant and informative read that helps the reader really understand social prescribing, the better to implement it in our own lives.
Bottom line: if you like having extra nonmedical approaches to avoid or alleviate medical problems, then this book will really help you achieve that.
Click here to check out The Connection Cure, and get social prescribing!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Bare-Bones Truth About Osteoporosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
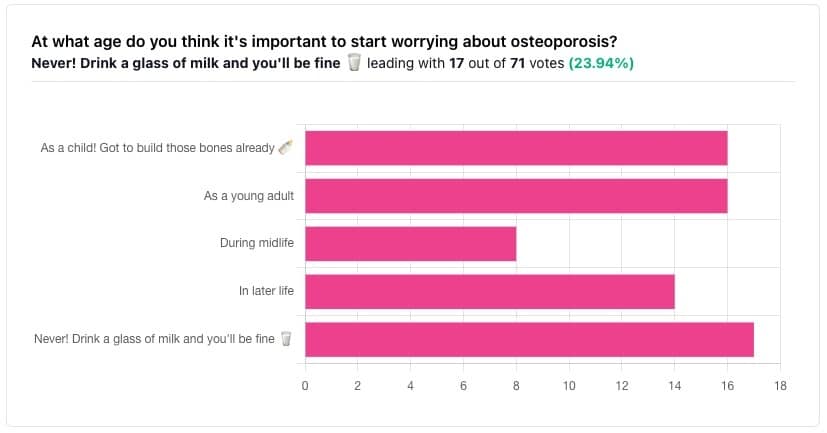
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
The Bare-bones Truth About Osteoporosis
In yesterday’s issue of 10almonds, we asked you “at what age do you think it’s important to start worrying about osteoporosis?”, and here’s the spread of answers you gave us:
At first glance it may seem shocking that a majority of respondents to a poll in a health-focused newsletter think it’ll never be an issue worth worrying about, but in fact this is partly a statistical quirk, because the vote of the strongest “early prevention” crowd was divided between “as a child” and “as a young adult”.
This poll also gave you the option to add a comment with your vote. Many subscribers chose to do so, explaining your choices… But, interestingly, not one single person who voted for “never” had any additional thoughts to add.
We loved reading your replies, by the way, and wish we had room to include them here, because they were very interesting and thought-provoking.
Let’s get to the myths and facts:
Top myth: “you will never need to worry about it; drink a glass of milk and you’ll be fine!”
The body is constantly repairing itself. Its ability to do that declines with age. Until about 35 on average, we can replace bone mineral as quickly as it is lost. After that, we lose it by up to 1% per year, and that rate climbs after 50, and climbs even more steeply for those who go through (untreated) menopause.
Losing 1% per year might not seem like a lot, but if you want to live to 100, there are some unfortunate implications!
About that menopause, by the way… Because declining estrogen levels late in life contribute significantly to osteoporosis, hormone replacement therapy (HRT) may be of value to many for the sake of bone health, never mind the more obvious and commonly-sought benefits.
On the topic of that glass of milk…
- Milk is a great source of calcium, which is useless to the body if you don’t also have good levels of vitamin D and magnesium.
- People’s vitamin D levels tend to directly correlate to the level of sun where they live, if supplementation isn’t undertaken.
- Plant-based milks are usually fortified with vitamin D (and calcium), by the way.
- Most people are deficient in magnesium, because green leafy things don’t form as big a part of most people’s diets as they should.
See also: An update on magnesium and bone health
Next most common myth: “bone health is all about calcium”
We spoke a little above about the importance of vitamin D and magnesium for being able to properly use that. But potassium is also critical:
Read more: The effects of potassium on bone health
While we’re on the topic…
People think of collagen as being for skin health. And it is important for that, but collagen’s benefits (and the negative effects of its absence) go much deeper, to include bone health. We’ve written about this before, so rather than take more space today, we’ll just drop the link:
We Are Such Stuff As Fish Are Made Of
Want to really maximize your bone health?
You might want to check out this well-sourced LiveStrong article:
Bone Health: Best and Worst Foods
(Teaser: leafy greens are in 2nd place, topped by sardines at #1—where do you think milk ranks?)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Surgery won’t fix my chronic back pain, so what will?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s ABC Four Corners episode Pain Factory highlighted that our health system is failing Australians with chronic pain. Patients are receiving costly, ineffective and risky care instead of effective, low-risk treatments for chronic pain.
The challenge is considering how we might reimagine health-care delivery so the effective and safe treatments for chronic pain are available to millions of Australians who suffer from chronic pain.
One in five Australians aged 45 and over have chronic pain (pain lasting three or more months). This costs an estimated A$139 billion a year, including $12 billion in direct health-care costs.
The most common complaint among people with chronic pain is low back pain. So what treatments do – and don’t – work?
Opioids and invasive procedures
Treatments offered to people with chronic pain include strong pain medicines such as opioids and invasive procedures such as spinal cord stimulators or spinal fusion surgery. Unfortunately, these treatments have little if any benefit and are associated with a risk of significant harm.
Spinal fusion surgery and spinal cord stimulators are also extremely costly procedures, costing tens of thousands of dollars each to the health system as well as incurring costs to the individual.
Addressing the contributors to pain
Recommendations from the latest Australian and World Health Organization clinical guidelines for low back pain focus on alternatives to drug and surgical treatments such as:
- education
- advice
- structured exercise programs
- physical, psychological or multidisciplinary interventions that address the physical or psychological contributors to ongoing pain.
Pain education is central. Monkey Business Images/Shutterstock Two recent Australian trials support these recommendations and have found that interventions that address each person’s physical and psychological contributors to pain produce large and sustained improvements in pain and function in people with chronic low back pain.
The interventions have minimal side effects and are cost-effective.
In the RESOLVE trial, the intervention consists of pain education and graded sensory and movement “retraining” aimed to help people understand that it’s safe to move.
In the RESTORE trial, the intervention (cognitive functional therapy) involves assisting the person to understand the range of physical and psychological contributing factors related to their condition. It guides patients to relearn how to move and to build confidence in their back, without over-protecting it.
Why isn’t everyone with chronic pain getting this care?
While these trials provide new hope for people with chronic low back pain, and effective alternatives to spinal surgery and opioids, a barrier for implementation is the out-of-pocket costs. The interventions take up to 12 sessions, lasting up to 26 weeks. One physiotherapy session can cost $90–$150.
In contrast, Medicare provides rebates for just five allied health visits (such as physiotherapists or exercise physiologists) for eligible patients per year, to be used for all chronic conditions.
Private health insurers also limit access to reimbursement for these services by typically only covering a proportion of the cost and providing a cap on annual benefits. So even those with private health insurance would usually have substantial out-of-pocket costs.
Access to trained clinicians is another barrier. This problem is particularly evident in regional and rural Australia, where access to allied health services, pain specialists and multidisciplinary pain clinics is limited.
Higher costs and lack of access are associated with the increased use of available and subsidised treatments, such as pain medicines, even if they are ineffective and harmful. The rate of opioid use, for example, is higher in regional Australia and in areas of socioeconomic disadvantage than metropolitan centres and affluent areas.
So what can we do about it?
We need to reform Australia’s health system, private and public, to improve access to effective treatments for chronic pain, while removing access to ineffective, costly and high-risk treatments.
Better training of the clinical workforce, and using technology such as telehealth and artificial intelligence to train clinicians or deliver treatment may also improve access to effective treatments. A recent Australian trial, for example, found telehealth delivered via video conferencing was as effective as in-person physiotherapy consultations for improving pain and function in people with chronic knee pain.
Advocacy and improving the public’s understanding of effective treatments for chronic pain may also be helpful. Our hope is that coordinated efforts will promote the uptake of effective treatments and improve the care of patients with chronic pain.
Christine Lin, Professor, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Fiona Blyth, Professor, University of Sydney; James Mcauley, Professor of Psychology, UNSW Sydney, and Mark Hancock, Professor of Physiotherapy, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: