The Mental Health Dangers Of Oversharing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oversharers can be fun and amiable; the life of the party. In and of itself, this something that can be considered “pro-social” and thus healthy.
But the problem for one’s mental health in the long-run lies in the “over” part of oversharing. Sometimes, if not checking in with the other person’s comfort, oversharing can be “trauma-dumping”, and push people away. Alternatively, if the oversharing exposes an unmet need, it can make the other person feel obliged to try to help in some fashion, which in the long run may also cause awkwardness and withdrawal.
Some potential problems are purely internal, such the feelings of shame or anxiety that can come afterwards; “I should not have been so vulnerable”, “What if my friends think badly of me now?”, etc.
And of course, sometimes those fears are then validated by reality, if “friends” indeed take advantage of that, or withdraw their friendship. That’s a minority occurrence, but it doesn’t make it any less of a crushing thing if it happens.
Sometimes people overshare because of being a bad judge of what’s a socially-approved appropriate amount of sharing; sometimes people overshare out of a need for closeness, and perhaps the hope of hearing what one needed to hear previously.
The dangers of oversharing don’t mean that we should never speak about our experiences and feelings; in fact sometimes, it is the most healthy thing to do—be it because it’s something that needs communicating to a specific person, or because it’s something we just need to “get off our chest”.
In short, it can be good to share! It can also be good to do so judiciously, by conscious decision and not in response to a spur-of-the-moment impulse, and remember to prioritize our own safety.
Below, Alain de Botton explains more of the psychodynamics of this:
Click Here If The Embedded Video Doesn’t Load Automatically!
10almonds tip, not included in the video: unsure whether your urge to share is too impulsive or not? Write a letter/email, and wait until the next day to decide whether or not to send it.
Want to read more?
Check out:
Breathe; Don’t Vent (At Least In The Moment)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Head hair comes in many colours, shapes and sizes, and hairstyles are often an expression of personal style or cultural identity.
Many different genes determine our hair texture, thickness and colour. But some people’s hair changes around the time of puberty, pregnancy or after chemotherapy.
So, what can cause hair to become curlier, thicker, thinner or grey?
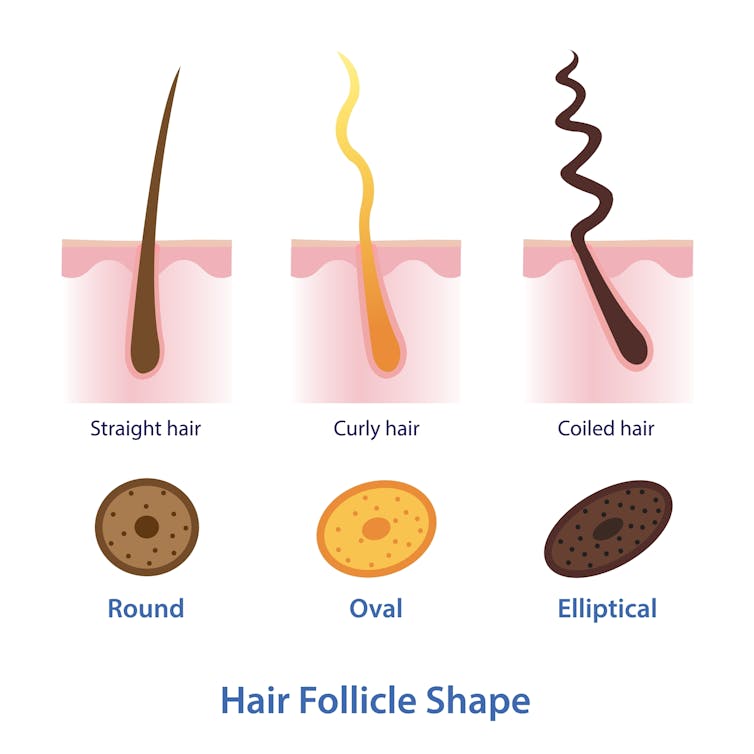
Curly or straight? How hair follicle shape plays a role
Hair is made of keratin, a strong and insoluble protein. Each hair strand grows from its own hair follicle that extends deep into the skin.
Curly hair forms due to asymmetry of both the hair follicle and the keratin in the hair.
Follicles that produce curly hair are asymmetrical and curved and lie at an angle to the surface of the skin. This kinks the hair as it first grows.
The asymmetry of the hair follicle also causes the keratin to bunch up on one side of the hair strand. This pulls parts of the hair strand closer together into a curl, which maintains the curl as the hair continues to grow.
Follicles that are symmetrical, round and perpendicular to the skin surface produce straight hair.

Each hair strand grows from its own hair follicle.
Mosterpiece/ShutterstockLife changes, hair changes
Our hair undergoes repeated cycles throughout life, with different stages of growth and loss.
Each hair follicle contains stem cells, which multiply and grow into a hair strand.
Head hairs spend most of their time in the growth phase, which can last for several years. This is why head hair can grow so long.
Let’s look at the life of a single hair strand. After the growth phase is a transitional phase of about two weeks, where the hair strand stops growing. This is followed by a resting phase where the hair remains in the follicle for a few months before it naturally falls out.
The hair follicle remains in the skin and the stems cells grow a new hair to repeat the cycle.
Each hair on the scalp is replaced every three to five years.

Each hair on the scalp is replaced every three to five years.
Just Life/ShutterstockHormone changes during and after pregnancy alter the usual hair cycle
Many women notice their hair is thicker during pregnancy.
During pregnancy, high levels of oestrogen, progesterone and prolactin prolong the resting phase of the hair cycle. This means the hair stays in the hair follicle for longer, with less hair loss.
A drop in hormones a few months after delivery causes increased hair loss. This is due to all the hairs that remained in the resting phase during pregnancy falling out in a fairly synchronised way.
Hair can change around puberty, pregnancy or after chemotherapy
This is related to the genetics of hair shape, which is an example of incomplete dominance.
Incomplete dominance is when there is a middle version of a trait. For hair, we have curly hair and straight hair genes. But when someone has one curly hair gene and one straight hair gene, they can have wavy hair.
Hormonal changes that occur around puberty and pregnancy can affect the function of genes. This can cause the curly hair gene of someone with wavy hair to become more active. This can change their hair from wavy to curly.
Researchers have identified that activating specific genes can change hair in pigs from straight to curly.
Chemotherapy has very visible effects on hair. Chemotherapy kills rapidly dividing cells, including hair follicles, which causes hair loss. Chemotherapy can also have genetic effects that influence hair follicle shape. This can cause hair to regrow with a different shape for the first few cycles of hair regrowth.

Your hair can change at different stages of your life.
Igor Ivakhno/ShutterstockHormonal changes as we age also affect our hair
Throughout life, thyroid hormones are essential for production of keratin. Low levels of thyroid hormones can cause dry and brittle hair.
Oestrogen and androgens also regulate hair growth and loss, particularly as we age.
Balding in males is due to higher levels of androgens. In particular, high dihydrotestosterone (sometimes shortened to DHT), which is produced in the body from testosterone, has a role in male pattern baldness.
Some women experience female pattern hair loss. This is caused by a combination of genetic factors plus lower levels of oestrogen and higher androgens after menopause. The hair follicles become smaller and smaller until they no longer produce hairs.
Reduced function of the cells that produce melanin (the pigment that gives our hair colour) is what causes greying.

Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Cold Medicines & Heart Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold Medicines & Heart Health
In the wake of many decongestants disappearing from a lot of shelves after a common active ingredient being declared useless*, you may find yourself considering alternative decongestants at this time of year.
*In case you missed it:
It doesn’t seem to be dangerous, by the way, just also not effective:
FDA Panel Says Common OTC Decongestant, Phenylephrine, Is Useless
Good for your nose, bad for your heart?
With products based on phenylephrine out of the running, products based on pseudoephedrine, a competing drug, are enjoying a surge in popularity.
Good news: pseudoephedrine works!
Bad news: pseudoephedrine works because it is a vasoconstrictor, and that vasoconstriction reduces nasal swelling. That same vasoconstriction also raises overall blood pressure, potentially dangerously, depending on an assortment of other conditions you might have.
Further reading: Can decongestants spike your blood pressure? What to know about hypertension and cold medicine
Who’s at risk?
The warning label, unread by many, reads:
❝Do not use this product if you have heart disease, high blood pressure, thyroid disease, diabetes, or difficulty in urination due to enlargement of the prostate gland, unless directed by a doctor❞
Source: Harvard Health | Don’t let decongestants squeeze your heart
What are the other options?
The same source as above recommends antihistamines as an option to be considered, citing:
❝Antihistamines such as […] cetirizine (Zyrtec) and loratadine (Claritin) can help with a stuffy nose and are safe for the heart.❞
But we’d be remiss not to mention drug-free options too, for example:
- Saline rinse with a neti pot or similar
- Use of a humidifier in your house/room
- Steam inhalation, with or without eucalyptus etc
See also: Inhaled Eucalyptus’s Immunomodulatory and Antimicrobial Effects
Take care!
Share This Post

Crispy Tofu Pad Thai
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Easy to make, delicious to enjoy, and packed with phytonutrients, this dish is a great one to add to your repertoire:
You will need
- 10 oz ready-to-wok rice noodles, or 6 oz dry
- 5 oz silken tofu
- 5 oz firm or extra firm tofu, cut into small cubes
- 1 oz arrowroot (or cornstarch if you don’t have arrowroot)
- 4 scallions, sliced
- ¼ bulb garlic, finely chopped
- 1″ piece fresh ginger, grated
- 1 red chili, chopped (multiply per your heat preferences)
- 1 red bell pepper, deseeded and thinly sliced
- 4 oz bok choi, thinly sliced
- 4 oz mung bean sprouts
- 1 tbsp tamari (or other, but tamari is traditional) soy sauce
- 1 tbsp sweet chili sauce
- Juice of ½ lime
- ½ tsp MSG or 1 tsp low-sodium salt
- Avocado oil, or your preferred oil for stir-frying
- To serve: lime wedges
- Optional garnish: crushed roasted peanuts (if allergic, substitute sesame seeds; peanuts are simply traditional, that’s all)
Method
(we suggest you read everything at least once before doing anything)
1) Scramble the silken tofu. For guidance and also additional seasoning pointers, see our Tasty Tofu Scramble recipe, but omit the thyme.
2) Cook the noodles if necessary (i.e. if they are the dry type and need boiling, as opposed to “ready-to-wok” noodles that don’t), drain, and set aside.
4) Prepare the tofu cubes: if the tofu cubes are dry to the touch, toss them gently in a little oil to coat. If they’re wet to the touch, no need. Dust the tofu cubes with the arrowroot and MSG/salt; you can do this in a bowl, tossing gently to distribute the coating evenly.
4) Heat some oil in a wok over a high heat, and fry the tofu on each side until golden and crispy all over, and set aside.
5) Stir-fry the scallions, garlic, ginger, chili, and bell pepper for about 2 minutes.
6) Add the bean sprouts and bok choi, and keep stir-frying for another 2 minutes.
7) Add everything that’s not already in the pan except the lime wedges and peanuts (i.e., add the things you set aside, plus the remaining as-yet-untouched ingredients) and stir-fry for a further 2 minutes.
8) Serve hot, garnished with the crushed peanuts if using, and with the lime wedges on the side:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Sprout Your Seeds, Grains, Beans, Etc
- Which Bell Peppers To Pick? A Spectrum Of Specialties
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
Related Posts

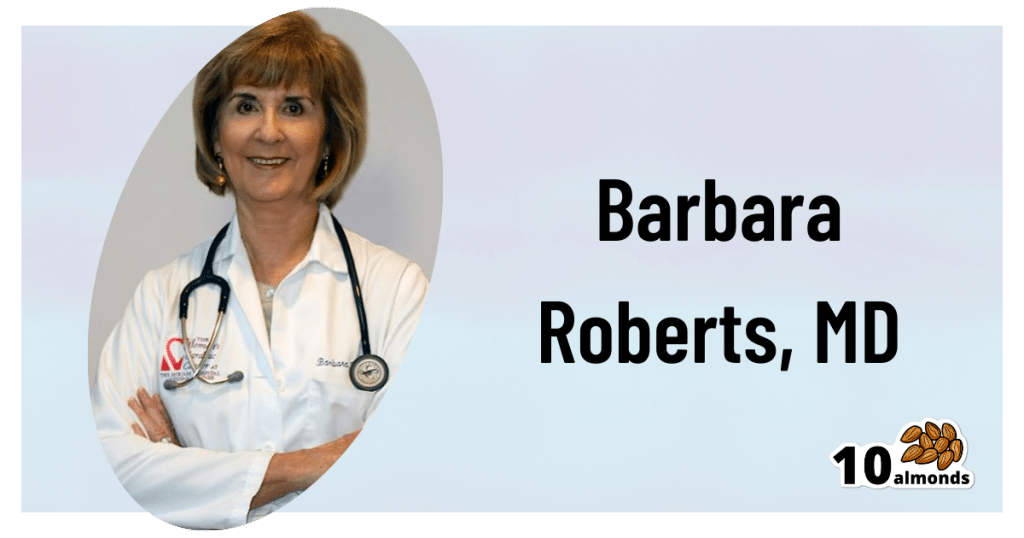
Statins: His & Hers?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Hidden Complexities of Statins and Cardiovascular Disease (CVD)

This is Dr. Barbara Roberts. She’s a cardiologist and the Director of the Women’s Cardiac Center at one of the Brown University Medical School teaching hospitals. She’s an Associate Clinical Professor of Medicine and takes care of patients, teaches medical students, and does clinical research. She specializes in gender-specific aspects of heart disease, and in heart disease prevention.
We previously reviewed Dr. Barbara Roberts’ excellent book “The Truth About Statins: Risks and Alternatives to Cholesterol-Lowering Drugs”. It prompted some requests to do a main feature about Statins, so we’re doing it today. It’s under the auspices of “Expert Insights” as we’ll be drawing almost entirely from Dr. Roberts’ work.
So, what are the risks of statins?
According to Dr. Roberts, one of the biggest risks is not just drug side-effects or anything like that, but rather, what they simply won’t treat. This is because statins will lower LDL (bad) cholesterol levels, without necessarily treating the underlying cause.
Imagine you got Covid, and it’s one of the earlier strains that’s more likely deadly than “merely” debilitating.
You’re coughing and your throat feels like you gargled glass.
Your doctor gives you a miracle cough medicine that stops your coughing and makes your throat feel much better.
(Then a few weeks later, you die, because this did absolutely nothing for the underlying problem)
You see the problem?
Are there problematic side-effects too, though?
There can be. But of course, all drugs can have side effects! So that’s not necessarily news, but what’s relevant here is the kind of track these side-effects can lead one down.
For example, Dr. Roberts cites a case in which a woman’s LDL levels were high and she was prescribed simvastatin (Zocor), 20mg/day. Here’s what happened, in sequence:
- She started getting panic attacks. So, her doctor prescribed her sertraline (Zoloft) (a very common SSRI antidepressant) and when that didn’t fix it, paroxetine (Paxil). This didn’t work either… because the problem was not actually her mental health. The panic attacks got worse…
- Then, while exercising, she started noticing progressive arm and leg weakness. Her doctor finally took her off the simvastatin, and temporarily switched to ezetimibe (Zetia), a less powerful nonstatin drug that blocks cholesterol absorption, which change eased her arm and leg problem.
- As the Zetia was a stopgap measure, the doctor put her on atorvastatin (Lipitor). Now she got episodes of severe chest pressure, and a skyrocketing heart rate. She also got tremors and lost her body temperature regulation.
- So the doctor stopped the atorvastatin and tried rosovastatin (Crestor), on which she now suffered exhaustion (we’re not surprised, by this point) and muscle pains in her arms and chest.
- So the doctor stopped the rosovastatin and tried lovastatin (Mevacor), and now she had the same symptoms as before, plus light-headedness.
- So the doctor stopped the lovastatin and tried fluvastatin (Lescol). Same thing happened.
- So he stopped the fluvastatin and tried pravastatin (Pravachol), without improvement.
- So finally he took her off all these statins because the high LDL was less deleterious to her life than all these things.
- She did her own research, and went back to the doctor to ask for cholestyramine (Questran), which is a bile acid sequestrent and nothing to do with statins. She also asked for a long-acting niacin. In high doses, niacin (one of the B-vitamins) raises HDL (good) cholesterol, lowers LDL, and lowers tryglycerides.
- Her own non-statin self-prescription (with her doctor’s signature) worked, and she went back to her life, her work, and took up running.
Quite a treatment journey! Want to know more about the option that actually worked?
Read: Bile Acid Resins or Sequestrants
What are the gender differences you/she mentioned?
A lot of this is still pending more research—basically it’s a similar problem in heart disease to one we’ve previously talked about with regard to diabetes. Diabetes disproportionately affects black people, while diabetes research disproportionately focuses on white people.
In this case, most heart disease research has focused on men, with women often not merely going unresearched, but also often undiagnosed and untreated until it’s too late. And the treatments, if prescribed? Assumed to be the same as for men.
Dr. Roberts tells of how medicine is taught:
❝When I was in medical school, my professors took the “bikini approach” to women’s health: women’s health meant breasts and reproductive organs. Otherwise the prototypical patient was presented as a man.❞
There has been some research done with statins and women, though! Just, still not a lot. But we do know for example that some statins can be especially useful for treating women’s atherosclerosis—with a 50% success rate, rather than 31% for men.
For lowering LDL, it can work but is generally not so hot in women.
Fun fact:
In men:
- High total cholesterol
- High non-HDL cholesterol
- High LDL cholesterol
- Low HDL cholesterol
…are all significantly associated with an increased risk of death from CVD.
In women:
…levels of LDL cholesterol even more than 190 were associated with only a small, statistically insignificant increased risk of dying from CVD.
So…
The fact that women derive less benefit from a medicine that mainly lowers LDL cholesterol, may be because elevated LDL cholesterol is less harmful to women than it is to men.
And also: Treatment and Response to Statins: Gender-related Differences
And for that matter: Women Versus Men: Is There Equal Benefit and Safety from Statins?*
Definitely a case where Betteridge’s Law of Headlines applies!
What should women do to avoid dying of CVD, then?
First, quick reminder of our general disclaimer: we can’t give medical advice and nothing here comprises such. However… One particularly relevant thing we found illuminating in Dr. Roberts’ work was this observation:
The metabolic syndrome is diagnosed if you have three (or more) out of five of the following:
- Abdominal obesity (waist >35″ if a woman or >40″ if a man)
- Fasting blood sugars of 100mg/dl or more
- Fasting triglycerides of 150mg/dl or more
- Blood pressure of 130/85 or higher
- HDL <50 if a woman or <40 if a man
And yet… because these things can be addressed with exercise and a healthy diet, which neither pharmaceutical companies nor insurance companies have a particular stake in, there’s a lot of focus instead on LDL levels (since there are a flock of statins that can be sold be lower them)… Which, Dr. Roberts says, is not nearly as critical for women.
So women end up getting prescribed statins that cause panic attacks and all those things we mentioned earlier… To lower our LDL, which isn’t nearly as big a factor as the other things.
In summary:
Statins do have their place, especially for men. They can, however, mask underlying problems that need treatment—which becomes counterproductive.
When it comes to women, statins are—in broad terms—statistically not as good. They are a little more likely to be helpful specifically in cases of atherosclerosis, whereby they have a 50/50 chance of helping.
For women in particular, it may be worthwhile looking into alternative non-statin drugs, and, for everyone: diet and exercise.
Further reading: How Can I Safely Come Off Statins?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Slowing the Progression of Cataracts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Understanding Cataracts
Cataracts are natural and impact everyone.
That’s a bit of a daunting opening line, but as Dr. Michele Lee, a board-certified ophthalmologist, explains, cataracts naturally develop with age, and can be accelerated by factors such as trauma, certain medications, and specific eye conditions.
We know how important your vision is to you (we’ve had great feedback about the book Vision for Life) as well as our articles on how glasses impact your eyesight and the effects of using eye drops.
While complete prevention isn’t possible, steps such as those mentioned below can be taken to slow their progression.
Here is an overview of the video’s first 3 takeaways. You can watch the whole video below.
Protect Your Eyes from Sunlight
Simply put, UV light damages lens proteins, which (significantly) contributes to cataracts. Wearing sunglasses can supposedly prevent up to 20% of cataracts caused by UV exposure.
Moderate Alcohol Consumption
We all, at some level, know that alcohol consumption doesn’t do us any good. Your eye health isn’t an exception to the rule; alcohol has been shown to contribute to cataract development.
If you’re looking at reducing your alcohol use, try reading this guide on lowering, or eradicating, alcohol consumption.
Avoid Smoking
Smokers are 2-3 times more likely to develop cataracts. Additionally, ensure good ventilation while cooking to avoid exposure to harmful indoor smoke.
See all 5 steps in the below video:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
First things first… How much fiber should we be eating?
- The World Health Organization recommends we each get at least 25g of fiber per day:
- A more recent meta-review of studies, involving thousands of people and decades of time, suggests 25–29g is ideal:
- The British Nutritional Foundation gives 30g as the figure:
- The US National Academy of Sciences’ Institute of Medicine recommends 21g–38g per day, depending on age and sex:
- A large study last year gave 30–40g as the figure:
*This one is also a great read to understand more about the “why” of fiber
Meanwhile, the average American gets 16g of fiber per day.
So, how to get more fiber, without piling on too many carbs?
Foods that contain fiber generally contain carbs (there’s a limit to how much celery most people want to eat), so there are two key ideas here:
- Getting a good carb:fiber ratio
- Making substitutions that boost fiber without overdoing (or in some case, even changing) carbs
Meat → Lentils
Well-seasoned lentils can be used to replaced ground beef or similar. A cup of boiled lentils contains 18g of fiber, so you’re already outdoing the average American’s daily total.
Meat → Beans
Black beans are a top-tier option here (15g per cup, cooked weight), but many kinds of beans are great.
Chicken/Fish → Chickpeas
Yes, chicken/fish is already meat, but we’re making a case for chickpeas here. Cooked and seasoned appropriately, they do the job, and pack in 12g of fiber per cup. Also… Hummus!
Bonus: Hummus, eaten with celery sticks.
White pasta/bread → Wholewheat pasta/bread
This is one where “moderation is key”, but if you’re going to eat pasta/bread, then wholewheat is the way to go. Fiber amounts vary, so read labels, but it will always have far more than white.
Processed salty snacks → Almonds and other nuts
Nuts in general are great, but almonds are top-tier for fiber, amongst other things. A 40g handful of almonds contains about 10g of fiber.
Starchy vegetables → Non-starchy vegetables
Potatoes, parsnips, and their friends have their place. But they cannot compete with broccoli, peas, cabbage, and other non-starchy vegetables for fiber content.
Bonus: if you’re going to have starchy vegetables though, leave the skins on!
Fruit juice → Fruit
Fruit juice has had most, if not all, of its fiber removed. Eat an actual juicy fruit, instead. Apples and bananas are great options; berries such as blackberries and raspberries are even better (at around 8g per cup, compared to the 5g or so depending on the size of an apple/banana)
Processed cereals → Oats
5g fiber per cup. Enough said.
Summary
Far from being a Herculean task, getting >30g of fiber per day can be easily accomplished by a lentil ragù with wholewheat pasta.
If your breakfast is overnight oats with fruit and some chopped almonds, you can make it to >20g already by the time you’ve finished your first meal of the day.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: