You, Happier – by Dr. Daniel Amen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The implicit question “what’s your brain type?” makes this book sound a little like a horoscope for science-enjoyers, but really, the “brain type” in question is simply a way of expressing which neurochemicals one’s brain makes most and/or least easily.
That’s something that a) really does differ from one person to another b) isn’t necessarily fixed forever, but will tend to remain mostly the same most of the time for most people.
And yes, the book does cover figuring out which neurotransmitter(s) it might be for you. On a secondary level, it also talks about more/less active parts of the brain for each of us, but the primary focus is on neurotransmitters.
It’s easy to assume “everyone wants more [your favorite neurotransmitter here]” but in fact, most people most of the time have most of what they need.
For those of us who don’t, those of us who perhaps have to work more to keep our level(s) of one or more neurotransmitters where they should be, this book is a great guide to optimizing aspects of our diet and lifestyle to compensate for what our brains might lack—potentially reducing the need to go for pharmaceutical approaches.
The style of the book is very much pop-science, but it is all well-informed and well-referenced.
Bottom line: if you sometimes (or often!) think “if only my brain would just make/acknowledge more [neurotransmitter], this book is for you.
Click here to check out You, Happier, and discover a happier you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Olive Oil vs Coconut Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing extra virgin olive oil to cold-pressed coconut oil, we picked the olive oil.
Why?
While the cold-pressed coconut oil may offer some health benefits due to its lauric acid content, its 80–90% saturated fat content isn’t great for most people. It’s a great oil when applied topically for healthy skin and hair, though!
The extra virgin olive oil has a much more uncontroversially healthy blend of triglycerides, and (in moderation) is universally recognized as very heart-healthy.
Your local supermarket, most likely, has a good extra virgin olive oil, but if you’d like to get some online, here’s an example product on Amazon for your convenience.
Share This Post
-
What You Should Have Been Told About The Menopause Beforehand
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What You Should Have Been Told About Menopause Beforehand
This is Dr. Jen Gunter. She’s a gynecologist, specializing in chronic pain and vulvovaginal disorders. She’s also a woman on a mission to demystify things that popular culture, especially in the US, would rather not talk about.
When was the last time you remember the menopause being referenced in a movie or TV show? If you can think of one at all, was it just played for laughs?
And of course, the human body can be funny, so that’s not necessarily the problem, but it sure would be nice if that weren’t all that there is!
So, what does Dr. Gunter want us to know?
It’s a time of changes, not an end
The name “menopause” is misleading. It’s not a “pause”, and those menses aren’t coming back.
And yet, to call it a “menostop” would be differently misleading, because there’s a lot more going on than a simple cessation of menstruation.
Estrogen levels will drop a lot, testosterone levels may rise slightly, mood and sleep and appetite and sex drive will probably be affected (progesterone can improve all these things!) and
not to mention butwe’re going to mention: vaginal atrophy, which is very normal and very treatable with a topical estrogen cream. Untreated menopause can also bring a whole lot of increased health risks (for example, heart disease, osteoporosis, and, counterintuitively given the lower estrogen levels, breast cancer).However, with a little awareness and appropriate management, all these things can usually be navigated with minimal adverse health outcomes.
Dr Gunter, for this reason, refers to it interchangeably as “the menopausal transition”. She describes it as being less like a cliff edge we fall off, and more like a bridge we cross.
Bridges can be dangerous to cross! But they can also get us safely where we’re going.
Ok, so how do we manage those things?
Dr. Gunter is a big fan of evidence-based medicine, so we’ll not be seeing any yonic crystals or jade eggs. Or “goop”.
See also: Meet Goop’s Number One Enemy
For most people, she recommends Menopausal Hormone Therapy (MHT), which falls under the more general category of Hormone Replacement Therapy (HRT).
This is the most well-evidenced, science-based way to avoid most of the risks associated with menopause.
Nevertheless, there are scare-stories out there, ranging from painful recommencement of bleeding, to (once again) increased risk of breast cancer. However, most of these are either misunderstandings, or unrelated to menopause and MHT, and are rather signs of other problems that should not be ignored.
To get a good grounding in this, you might want to read her Hormone Therapy Guide, freely available as a standalone section on her website. This series of posts is dedicated to hormone therapy. It starts with some basics and builds on that knowledge with each post:
Dr. Gunter’s Guide To The Hormone Menoverse
What about natural therapies?
There are some non-hormonal things that work, but these are mostly things that:
- give a statistically significant reduction in symptoms
- give the same statistically significant reduction in symptoms as placebo
As Dr. Gunter puts it:
❝While most of the studies of prescription medications for hot flashes have an appropriate placebo arm, this is rarely the case with so-called alternative therapies.
In fact, the studies here are almost always low quality, so it’s often not possible to conclude much.
Many reviews that look at these studies often end with a line that goes something like, “Randomized trials with a placebo arm, a low risk of bias, and adequate sample sizes are urgently needed.”
You should interpret this kind of conclusion as the polite way of saying, “We need studies that aren’t BS to say something constructive.”❞
However, if it works, it works, whatever its mechanism. It’s just good, when making medical decisions, to do so with the full facts!
For that matter, even Dr. Gunter acknowledges that while MHT can be lifechanging (in a positive way) for many, it’s not for everyone:
Informed Decisions: When Menopause Hormone Therapy Isn’t Recommended
Want to know more?
Dr. Gunter also has an assortment of books available, including The Menopause Manifesto (which we’ve reviewed previously), and some others that we haven’t, such as “Blood” and “The Vagina Bible”.
Enjoy!
Share This Post
-
Discipline is Destiny – by Ryan Holiday
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another of Holiday’s books, The Daily Stoic, and here is another excellent work from the same author.
We’re not a philosophy newsletter, but there are some things that make a big difference to physical and mental health, the habits we build, and the path we take in life for better or for worse.
Self-discipline is one of those things. A lot of the time, we know what we need to do, but knowing isn’t the problem. We need to actually do it! This applies to diet, exercise, sleep, and more.
Holiday gives us, in a casual easy-reading style, timeless principles to lock in strong discipline and good habits for life.
The book’s many small chapters, by the way, are excellent for reading a chapter-per-day as a healthy dose of motivation each morning, if you’re so inclined.
Bottom line: if you’ve noticed that one of the biggest barriers between you and your goals is actually doing the necessary things in a disciplined fashion, then this book will help you become more efficient, and actually get there.
Click here to check out Discipline is Destiny, and upgrade yours!
Share This Post
Related Posts
-
Mental Health Courts Can Struggle to Fulfill Decades-Old Promise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GAINESVILLE, Ga. — In early December, Donald Brown stood nervously in the Hall County Courthouse, concerned he’d be sent back to jail.
The 55-year-old struggles with depression, addiction, and suicidal thoughts. He worried a judge would terminate him from a special diversion program meant to keep people with mental illness from being incarcerated. He was failing to keep up with the program’s onerous work and community service requirements.
“I’m kind of scared. I feel kind of defeated,” Brown said.
Last year, Brown threatened to take his life with a gun and his family called 911 seeking help, he said. The police arrived, and Brown was arrested and charged with a felony of firearm possession.
After months in jail, Brown was offered access to the Health Empowerment Linkage and Possibilities, or HELP, Court. If he pleaded guilty, he’d be connected to services and avoid prison time. But if he didn’t complete the program, he’d possibly face incarceration.
“It’s almost like coercion,” Brown said. “‘Here, sign these papers and get out of jail.’ I feel like I could have been dealt with a lot better.”
Advocates, attorneys, clinicians, and researchers said courts such as the one Brown is navigating can struggle to live up to their promise. The diversion programs, they said, are often expensive and resource-intensive, and serve fewer than 1% of the more than 2 million people who have a serious mental illness and are booked into U.S. jails each year.
People can feel pressured to take plea deals and enter the courts, seeing the programs as the only route to get care or avoid prison time. The courts are selective, due in part to political pressures on elected judges and prosecutors. Participants must often meet strict requirements that critics say aren’t treatment-focused, such as regular hearings and drug screenings.
And there is a lack of conclusive evidence on whether the courts help participants long-term. Some legal experts, like Lea Johnston, a professor of law at the University of Florida, worry the programs distract from more meaningful investments in mental health resources.
Jails and prisons are not the place for individuals with mental disorders, she said. “But I’m also not sure that mental health court is the solution.”
The country’s first mental health court was established in Broward County, Florida, in 1997, “as a way to promote recovery and mental health wellness and avoid criminalizing mental health problems.” The model was replicated with millions in funding from such federal agencies as the Substance Abuse and Mental Health Services Administration and the Department of Justice.
More than 650 adult and juvenile mental health courts were operational as of 2022, according to the National Treatment Court Resource Center. There’s no set way to run them. Generally, participants receive treatment plans and get linked to services. Judges and mental health clinicians oversee their progress.
Researchers from the center found little evidence that the courts improve participants’ mental health or keep them out of the criminal justice system. “Few studies … assess longer-term impacts” of the programs “beyond one year after program exit,” said a 2022 policy brief on mental health courts.
The courts work best when paired with investments in services such as clinical treatment, recovery programs, and housing and employment opportunities, said Kristen DeVall, the center’s co-director.
“If all of these other supports aren’t invested in, then it’s kind of a wash,” she said.
The courts should be seen as “one intervention in that larger system,” DeVall said, not “the only resource to serve folks with mental health needs” who get caught up in the criminal justice system.
Resource limitations can also increase the pressures to apply for mental health court programs, said Lisa M. Wayne, executive director of the National Association of Criminal Defense Lawyers. People seeking help might not feel they have alternatives.
“It’s not going to be people who can afford mental health intervention. It’s poor people, marginalized folks,” she said.
Other court skeptics wonder about the larger costs of the programs.
In a study of a mental health court in Pennsylvania, Johnston and a University of Florida colleague found participants were sentenced to longer time under government supervision than if they’d gone through the regular criminal justice system.
“The bigger problem is they’re taking attention away from more important solutions that we should be investing in, like community mental health care,” Johnston said.
When Melissa Vergara’s oldest son, Mychael Difrancisco, was arrested on felony gun charges in Queens in May 2021, she thought he would be an ideal candidate for the New York City borough’s mental health court because of his diagnosis of autism spectrum disorder and other behavioral health conditions.
She estimated she spent tens of thousands of dollars to prepare Difrancisco’s case for consideration. Meanwhile, her son sat in jail on Rikers Island, where she said he was assaulted multiple times and had to get half a finger amputated after it was caught in a cell door.
In the end, his case was denied diversion into mental health court. Difrancisco, 22, is serving a prison sentence that could be as long as four years and six months.
“There’s no real urgency to help people with mental health struggles,” Vergara said.
Critics worry such high bars to entry can lead the programs to exclude people who could benefit the most. Some courts don’t allow those accused of violent or sexual crimes to participate. Prosecutors and judges can face pressure from constituents that may lead them to block individuals accused of high-profile offenses.
And judges often aren’t trained to make decisions about participants’ care, said Raji Edayathumangalam, senior policy social worker with New York County Defender Services.
“It’s inappropriate,” she said. “We’re all licensed to practice in our different professions for a reason. I can’t show up to do a hernia operation just because I read about it or sat next to a hernia surgeon.”
Mental health courts can be overly focused on requirements such as drug testing, medication compliance, and completing workbook assignments, rather than progress toward recovery and clinical improvement, Edayathumangalam said.
Completing the programs can leave some participants with clean criminal records. But failing to meet a program’s requirements can trigger penalties — including incarceration.
During a recent hearing in the Clayton County Behavioral Health Accountability Court in suburban Atlanta, one woman left the courtroom in tears when Judge Shana Rooks Malone ordered her to report to jail for a seven-day stay for “being dishonest” about whether she was taking court-required medication.
It was her sixth infraction in the program — previous consequences included written assignments and “bench duty,” in which participants must sit and think about their participation in the program.
“I don’t like to incarcerate,” Malone said. “That particular participant has had some challenges. I’m rooting for her. But all the smaller penalties haven’t worked.”
Still, other participants praised Malone and her program. And, in general, some say such diversion programs provide a much-needed lifeline.
Michael Hobby, 32, of Gainesville was addicted to heroin and fentanyl when he was arrested for drug possession in August 2021. After entry into the HELP Court program, he got sober, started taking medication for anxiety and depression, and built a stable life.
“I didn’t know where to reach out for help,” he said. “I got put in handcuffs, and it saved my life.”
Even as Donald Brown awaited his fate, he said he had started taking medication to manage his depression and has stayed sober because of HELP Court.
“I’ve learned a new way of life. Instead of getting high, I’m learning to feel things now,” he said.
Brown avoided jail that early December day. A hearing to decide his fate could happen in the next few weeks. But even if he’s allowed to remain in the program, Brown said, he’s worried it’s only a matter of time before he falls out of compliance.
“To try to improve myself and get locked up for it is just a kick in the gut,” he said. “I tried really hard.”
KFF Health News senior correspondent Fred Clasen-Kelly contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Unprocess Your Life – by Rob Hobson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rob Hobson is not a doctor, but he is a nutritionist with half the alphabet after his name (BSc, PGDip, MSc, AFN, SENR) and decades of experience in the field.
The book covers, in jargon-free fashion, the science of ultra-processed foods, and why for example that pack of frozen chicken nuggets are bad but a pack of tofu (which obviously also took some processing, because it didn’t grow on the plant like that) isn’t.
This kind of explanation puts to rest a lot of the “does this count?” queries that a reader might have when giving the shopping list a once-over.
He also covers practical considerations such as kitchen equipment that’s worth investing in if you don’t already have it, and an “unprocessed pantry” shopping list.
The recipes (yes, there are recipes, nearly a hundred of them) are not plant-based by default, but there is a section of vegan and vegetarian recipes. Given that the theme of the book is replacing ultra-processed foods, it doesn’t mean a life of abstemiousness—there are recipes for all manner of things from hot sauce to cakes. Just, healthier unprocessed ones! There are classically healthy recipes too, of course.
Bottom line: if you’ve been wishing for a while that you could get rid of those processed products that are just so convenient that you haven’t got around to replacing them with healthier options, this book can indeed help you do just that.
Click here to check out Unprocess Your Life, and unprocess your life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
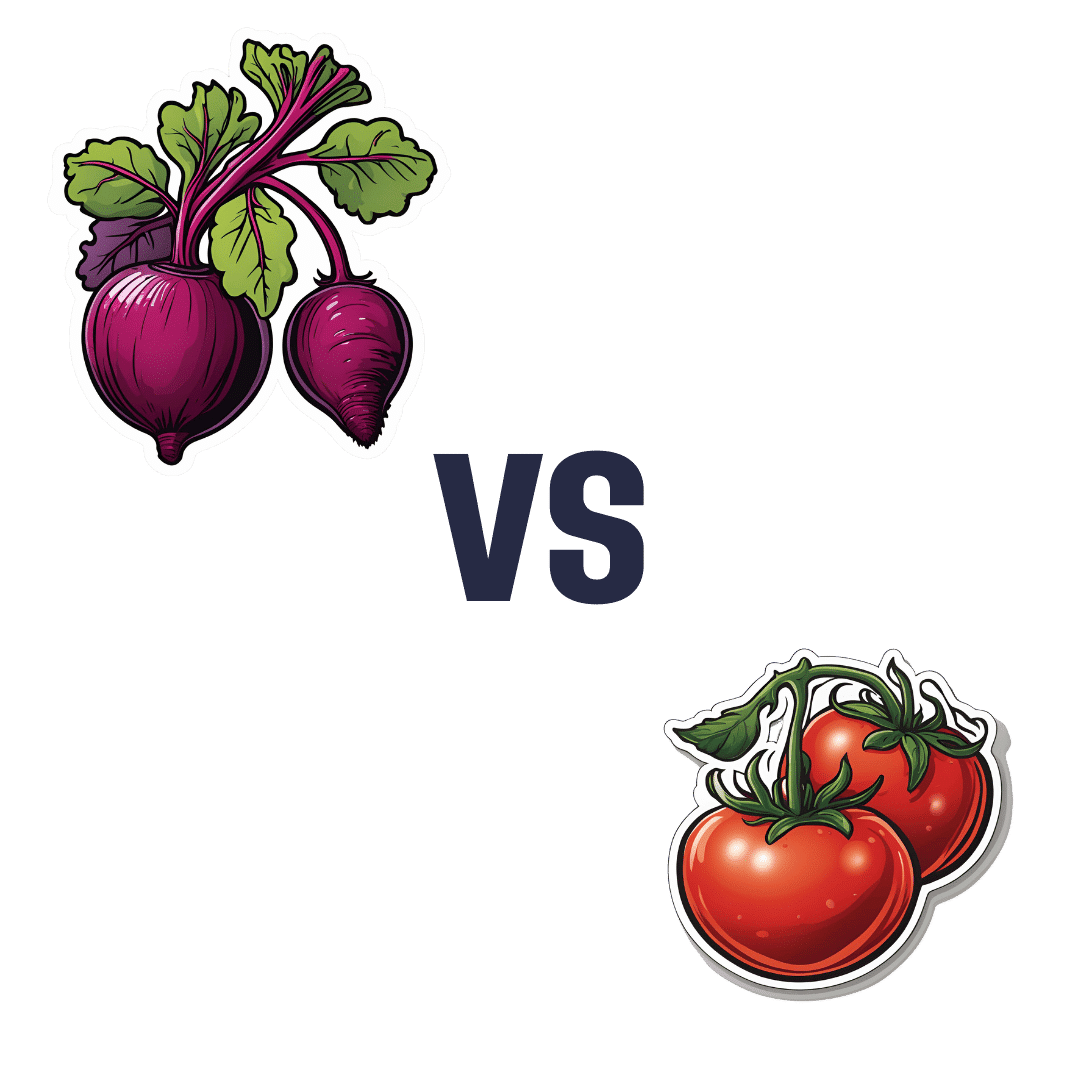
Beetroot vs Tomato – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to tomato, we picked the beetroot.
Why?
Both are great! But we say beetroot comes out on top:
In terms of macros, beetroot has more protein, carbs, and fiber, making it the more nutritionally dense option. It has a slightly higher glycemic index, but also has specific phytochemicals that lower blood sugars and increase insulin sensitivity, more than cancelling that out. So, a clear win for beetroot in this regard.
In the category of vitamins, beetroot has more of vitamins B2, B5, B7, and B9, while tomato has more of vitamins A, C, E, and K. We’d call that a 4:4 tie, but tomato’s margins of difference are greater, so we say tomato wins this round.
When it comes to minerals, beetroot has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while tomatoes are not higher in any mineral. An easy win for beetroot here.
Looking at polyphenols and other remaining phytochemicals, beetroot has most, and especially its betalain content goes a long way. Tomatoes, meanwhile, have a famously high lycopene content (a highly beneficial carotenoid). All in all, it could swing either way based on subjective factors, so we’re saying it’s a tie this time.
Adding up the sections makes for an overall win for beetroot, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
- Beetroot For More Than Just Your Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: