Alzheimer’s Causative Factors To Avoid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Best Brains Bar Nun?
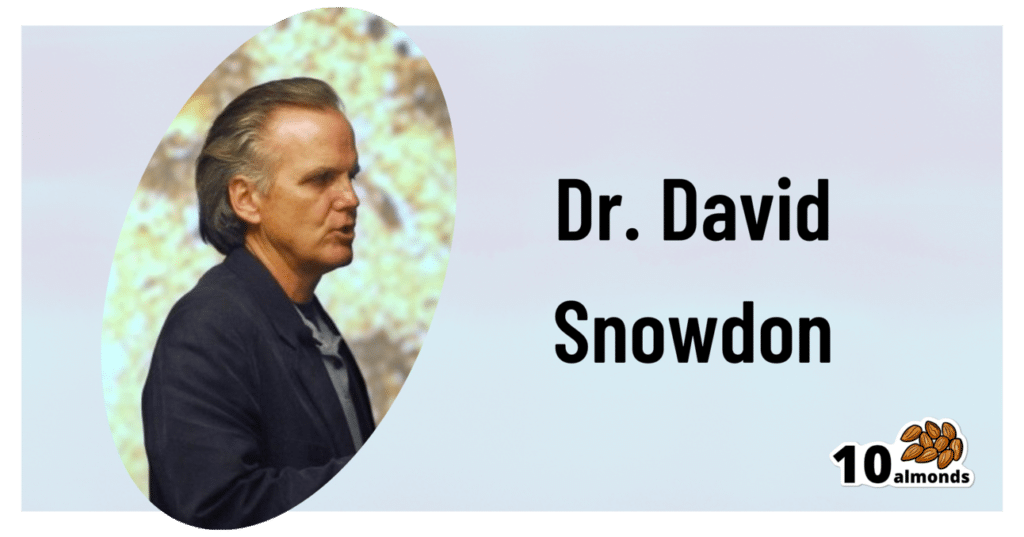
This is Dr. David Snowdon. He’s an epidemiologist, and one of the world’s foremost experts on Alzheimer’s disease. He was also, most famously, the lead researcher of what has become known as “The Nun Study”.
We recently reviewed his book about this study:
…which we definitely encourage you to check out, but we’ll do our best to summarize its key points today!
Reassurance up-front: no, you don’t have to become a nun
The Nun Study
In 1991, a large number (678) of nuns were recruited for what was to be (and until now, remains) the largest study of its kind into the impact of a wide variety of factors on aging, and in particular, Alzheimer’s disease.
Why it was so important: because the nuns were all from the same Order, had the same occupation (it’s a teaching Order), with very similar lifestyles, schedules, socioeconomic status, general background, access to healthcare, similar diets, same relationship status (celibate), same sex (female), and many other factors also similar, this meant that most of the confounding variables that confound other studies were already controlled-for here.
Enrollment in the study also required consenting to donating one’s brain for study post-mortem—and of those who have since died, indeed 98% of them have been donated (the other 2%, we presume, may have run into technical administrative issues with the donation process, due to the circumstances of death and/or delays in processing the donation).
How the study was undertaken
We don’t have enough space to describe the entire methodology here, but the gist of it is:
- Genetic testing for relevant genetic factors
- Data gathered about lives so far, including not just medical records but also autobiographies that the nuns wrote when they took their vows (at ages 19–21)
- Extensive ongoing personal interviews about habits, life choices, and attitudes
- Yearly evaluations including memory tests and physical function tests
- Brain donation upon death
What they found
Technically, The Nun Study is still ongoing. Of the original 678 nuns (aged 75–106), three are still alive (based on the latest report, at least).
However, lots of results have already been gained, including…
Genes
A year into the study, in 1992, the “apolipoprotein E” (APOE) gene was established as a likely causative factor in Alzheimer’s disease. This is probably not new to our readers in 2024, but there are interesting things being learned even now, for example:
The Alzheimer’s Gene That Varies By Race & Sex
…but watch out! Because also:
Alzheimer’s Sex Differences May Not Be What They Appear
Words
Based on the autobiographies written by the nuns in their youth upon taking their vows, there were two factors that were later correlated with not getting dementia:
- Longer sentences
- Positive outlook
- “Idea density”
That latter item means the relative linguistic density of ideas and complexity thereof, and the fluency and vivacity with which they were expressed (this was not a wishy-washy assessment; there was a hard-science analysis to determine numbers).
Want to spruce up yours? You might like to check out:
Reading, Better: Reading As A Cognitive Exercise
…for specific, evidence-based ways to tweak your reading to fight cognitive decline.
Food
While the dietary habits of the nuns were fairly homogenous, those who favored eating more and cooked greens, beans, and tomatoes, lived longer and with healthier brains.
See also: Brain Food? The Eyes Have It!
Other aspects of brain health & mental health
The study also found that nuns who avoided stroke and depression, were also less likely to get dementia.
For tending to these, check out:
- Two Things You Can Do To Improve Stroke Survival Chances
- Depression, And The Mental Health First-Aid That You’ll Hopefully Never Need
- Behavioral Activation Against Depression & Anxiety
Community & Faith
Obviously, in this matter the nuns were quite a homogenous group, scoring heavily in community and faith. What’s relevant here is the difference between the nuns, and other epidemiological studies in other groups (invariably not scoring so highly).
Community & faith are considered, separately and together, to be protective factors against dementia.
Faith may be something that “you have it or you don’t” (we’re a health science newsletter, not a theological publication, but for the interested, philosopher John Stuart Mill’s 1859 essay “On Liberty“ makes a good argument for it not being something one can choose, prompting him to argue for religious tolerance, on the grounds that religious coercion is a futile effort precisely because a person cannot choose to dis/believe something)
…but community can definitely be chosen, nurtured, and grown. We’ve written about this a bit before:
You might also like to check out this great book on the topic:
Purpose: Design A Community And Change Your Life – by Gina Bianchini
Want more?
We gave a ground-up primer on avoiding Alzheimer’s and other dementias; check it out:
How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When Age Is A Flexible Number
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aging, Counterclockwise!
In the late 1970s, Dr. Ellen Langer hypothesized that physical markers of aging could be affected by psychosomatic means.
Note: psychosomatic does not mean “it’s all in your head”.
Psychosomatic means “your body does what your brain tells it to do, for better or for worse”
She set about testing that, in what has been referred to since as…
The Counterclockwise Study
A small (n=16) sample of men in their late 70s and early 80s were recruited in what they were told was a study about reminiscing.
Back in the 1970s, it was still standard practice in the field of psychology to outright lie to participants (who in those days were called “subjects”), so this slight obfuscation was a much smaller ethical aberration than in some famous studies of the same era and earlier (cough cough Zimbardo cough Milgram cough).
Anyway, the participants were treated to a week in a 1950s-themed retreat, specifically 1959, a date twenty years prior to the experiment’s date in 1979. The environment was decorated and furnished authentically to the date, down to the food and the available magazines and TV/radio shows; period-typical clothing was also provided, and so forth.
- The control group were told to spend the time reminiscing about 1959
- The experimental group were told to pretend (and maintain the pretense, for the duration) that it really was 1959
The results? On many measures of aging, the experimental group participants became quantifiably younger:
❝The experimental group showed greater improvement in joint flexibility, finger length (their arthritis diminished and they were able to straighten their fingers more), and manual dexterity.
On intelligence tests, 63 percent of the experimental group improved their scores, compared with only 44 percent of the control group. There were also improvements in height, weight, gait, and posture.
Finally, we asked people unaware of the study’s purpose to compare photos taken of the participants at the end of the week with those submitted at the beginning of the study. These objective observers judged that all of the experimental participants looked noticeably younger at the end of the study.❞
Remember, this was after one week.
Her famous study was completed in 1979, and/but not published until eleven years later in 1990, with the innocuous title:
Higher stages of human development: Perspectives on adult growth
You can read about it much more accessibly, and in much more detail, in her book:
Counterclockwise: A Proven Way to Think Yourself Younger and Healthier – by Dr. Ellen Langer
We haven’t reviewed that particular book yet, so here’s Linda Graham’s review, that noted:
❝Langer cites other research that has made similar findings.
In one study, for instance, 650 people were surveyed about their attitudes on aging. Twenty years later, those with a positive attitude with regard to aging had lived seven years longer on average than those with a negative attitude to aging.
(By comparison, researchers estimate that we extend our lives by four years if we lower our blood pressure and reduce our cholesterol.)
In another study, participants read a list of negative words about aging; within 15 minutes, they were walking more slowly than they had before.❞
Read the review in full:
Aging in Reverse: A Review of Counterclockwise
The Counterclockwise study has been repeated since, and/but we are still waiting for the latest (exciting, much larger sample, 90 participants this time) study to be published. The research proposal describes the method in great detail, and you can read that with one click over on PubMed:
It was approved, and has now been completed (as of 2020), but the results have not been published yet; you can see the timeline of how that’s progressing over on ClinicalTrials.gov:
Clinical Trials | Ageing as a Mindset: A Counterclockwise Experiment to Rejuvenate Older Adults
Hopefully it’ll take less time than the eleven years it took for the original study, but in the meantime, there seems to be nothing to lose in doing a little “Citizen Science” for ourselves.
Maybe a week in a 20 years-ago themed resort (writer’s note: wow, that would only be 2004; that doesn’t feel right; it should surely be at least the 90s!) isn’t a viable option for you, but we’re willing to bet it’s possible to “microdose” on this method. Given that the original study lasted only a week, even just a themed date-night on a regular recurring basis seems like a great option to explore (if you’re not partnered then well, indulge yourself how best you see fit, in accord with the same premise; a date-night can be with yourself too!).
Just remember the most important take-away though:
Don’t accidentally put yourself in your own control group!
In other words, it’s critically important that for the duration of the exercise, you act and even think as though it is the appropriate date.
If you instead spend your time thinking “wow, I miss the [decade that does it for you]”, you will dodge the benefits, and potentially even make yourself feel (and thus, potentially, if the inverse hypothesis holds true, become) older.
This latter is not just our hypothesis by the way, there is an established potential for nocebo effect.
For example, the following study looked at how instructions given in clinical tests can be worded in a way that make people feel differently about their age, and impact the results of the mental and/or physical tests then administered:
❝Our results seem to suggest how manipulations by instructions appeared to be more largely used and capable of producing more clear performance variations on cognitive, memory, and physical tasks.
Age-related stereotypes showed potentially stronger effects when they are negative, implicit, and temporally closer to the test of performance. ❞
(and yes, that’s the same Dr. Francesco Pagnini whose name you saw atop the other study we cited above, with the 90 participants recreating the Counterclockwise study)
Want to know more about [the hard science of] psychosomatic health?
Check out Dr. Langer’s other book, which we reviewed recently:
The Mindful Body: Thinking Our Way to Chronic Health – by Dr. Ellen Langer
Enjoy!
Share This Post
-
Longevity for the Lazy – by Dr. Richard Malish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are some people who devote all their resources to longevity, which can become a full-time occupation, not to mention a very expensive endeavor. This book’s for those who want to get the best possible “bang for buck” by doing the things that have the most favorable cost:worth ratio.
Dr. Malish covers what can be done easily for personal longevity, as well as what technological advances can be enjoyed that those before us didn’t have as options. He also discusses the diseases that are most likely to kill us, and how to avoid those.
He preaches a proactive approach, but one that is simple and consistent and based in good science, and good statistics. Indeed, while he’s served 20 years as an army doctor and a cardiologist, he now works as a healthcare policy consultant, so he is well-placed to advise.
The style of the book is halfway between regular pop-science and a textbook; you can either read it cover-to-cover, or skim first though the key points, highlight boxes, summaries, and the like. He also provides a time-phased task list, for those who like things to be laid out like that.
Bottom line: this is a very good, methodical guide to living longer without making it a full-time occupation.
Share This Post
-
Just One Heart – by Dr. Jonathan Fisher
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this is not: a book to say eat fiber, go easy on the salt, get some exercise, and so forth.
What this rather is: a book about the connection between the heart and mind; often written poetically, the simple biological reality is that our emotional state does have a genuine impact on our heart health, and as such, any effort to look after our heart (healthwise) would be incomplete without an effort to look after our heart (emotionally).
Dr. Fisher talks about the impact of stress and uncertainty, as well as peace and security, on heart health—and then, having sorted emotional states into “heart breakers” and “heart wakers”, he goes about laying out a plan for what is, emotionally and thus also physiologically, good for our heart.
Chapter by chapter, he walks us through the 7 principles to live by:
- Steadiness: how to steady your heart amid chaos
- Wisdom: how to develop a wise heart in uncertain times
- Openness: how to safely open your heart in a threatening world
- Wholeness: how to show up with your whole heart without going to pieces
- Courage: how to lead with a courageous heart when fear surrounds you
- Lightness: how to live with a light heart in a heavy world
- Warmth: how to love with a warm heart when life feels cold
The style is anything but clinical; it’s well-written, certainly, and definitely informed in part by his medical understanding of the heart, but it’s entirely the raw human element that shines throughout, and that makes the ideas a lot more tangible.
Bottom line: if you’d like your heart to be healthy (cardiac health) and your heart to be healthy (emotional health), this book is a very worthwhile read.
Click here to check out Just One Heart, and take care of yours!
Share This Post
Related Posts
-
NADᐩ Against Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nicotinamide adenine dinucleotide, or “NAD” to its friends, is a coenzyme produced in the human body (amongst other places), and it is critical for cellular energy metabolism, but there’s more to it than that.
Today we’ll be looking mostly at NAD+, of which the + indicates the positive formal charge of one of its nitrogen atoms. We won’t get too much into the chemistry of this, but we will mention that it’s a cofactor with NADH—the former accepting electrons and the latter donating electrons.
Both NAD+ and NADH are critical to good health, but we’re going to focus on NAD+ for the simple reason that it gets depleted with aging.
Note: it gets depleted with aging.
Chronological age is not so important here, but there is a direct relationship between biological aging and NAD+ depletion.
For example, healthy centenarians tend not to have depleted NAD+ levels. Further, its depletion (in those in whom it is depleted) is then a causal factor for many age-related diseases:
❝Remarkably, ageing is accompanied by a gradual decline in tissue and cellular NAD+ levels in multiple model organisms, including rodents and humans.
This decline in NAD+ levels is linked causally to numerous ageing-associated diseases, including cognitive decline, cancer, metabolic disease, sarcopenia and frailty.
Many of these ageing-associated diseases can be slowed down and even reversed by restoring NAD+ levels.❞
~ Dr. Rosalba Perrone et al.
Read in full: NAD+ metabolism and its roles in cellular processes during ageing
As for restoring those NADᐩ levels, that does help in interventional trials, whether by supplementing directly, or with NAD precursors*:
❝NAD+ levels steadily decline with age, resulting in altered metabolism and increased disease susceptibility.
Restoration of NAD+ levels in old or diseased animals can promote health and extend lifespan, prompting a search for safe and efficacious NAD-boosting molecules that hold the promise of increasing the body’s resilience, not just to one disease, but to many, thereby extending healthy human lifespan.❞
~ Dr. David Sinclair et al.
Read more: Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
*There are actually also other NAD-boosting molecules besides NAD itself and its precursors. For example, the liver will not produce NADᐩ unless it has aminocarboxymuconate-semialdehyde decarboxylase (or “ACMSD”, to its friends), which limits the production of NADᐩ. Why, you ask? The theory is that it is a kind of evolutionary conservativism, much like not lighting a fire without the ability to put it out. In any case, taking ACMSD-blockers will thus result in an increased endogenous production of NADᐩ.
You can read about this here:
De novo NAD+ synthesis enhances mitochondrial function and improves health
Nor is taking supplements or drugs the only way to get more of it; there’s an enzyme nicotinamide phosphoribosyltransferase (“NAMPT”, to its friends) involved in the synthesis of NADᐩ, and exercise boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
And to underline that point, another study found that resistance training (so, a different kind of exercise from that of the previous study) boosts levels of NADᐩ itself by the same 127%:
One way to get more out of NADᐩ
We’ll get straight to the point: it works very well paired with a senolytic agent, i.e. something that kills aging cells so that they get recycled sooner:
NAD+, Senolytics, or Pyruvate for Healthy Aging?
To read more about senolytics, check out:
Fisetin: The Anti-Aging Assassin
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fix Chronic Fatigue & Regain Your Energy, By Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Chronic fatigue is on the rise. A lot of it appears to be Long COVID-related, but whether that’s the case for you or not, one thing that will make a big difference to your energy levels is something that French biochemist Jessie Inchauspé is here to explain:
Mitochondrial management
Inchauspé explains it in terms of a steam train; to keep running, it must have coal burning in its furnace. However, if more coal is delivered to the engine room faster than it can be put in the furnace and burned, and the coal just keeps on coming, the worker there will soon be overwhelmed trying to find places to put it all; the engine room will be full of coal, and the furnace will sputter and go out because the worker can’t even reach it on account of being buried in coal.
So it is with our glucose metabolism also. If we get spikes of glucose faster than our body can deal with them, it will overload the body’s ability to process that energy at all. Just like the steam train worker, our body will try! It’ll stuff that extra glucose wherever it can (storing as glycogen in the liver is a readily available option that’s easy to do and/but also gives you non-alcoholic fatty liver disease and isn’t quickly broken down into useable energy), and meanwhile, your actual mitochondria aren’t getting what they need (which is: a reliable, but gentle, influx of glucose).
You can imagine that the situation we described in the steam train isn’t good for the engine’s longevity, and the corresponding situation in the human body isn’t good for our mitochondria either (or our pancreas, or our liver, or… the list goes on). Indeed, damaged mitochondria affect exercise capacity and stress resilience—as well as being a long-term driver of cancer.
The remedy, of course, is blood sugar management. Specifically, avoiding glucose spikes. She has a list of 10 ways to do this (small changes to how we eat; what things to eat with what, in which order, etc) that make a huge measurable difference. For your convenience, we’ve linked those ten ways below; first though, if you’d like to hear it from Inchauspé directly (her style is very pleasant), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- 10 Ways To Balance Your Blood Sugars ← this is the longer list she’s referring to in the video!
- How To Unfatty A Fatty Liver ← also relevant
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Families including someone with mental illness can experience deep despair. They need support
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the aftermath of the tragic Bondi knife attack, Joel Cauchi’s parents have spoken about their son’s long history of mental illness, having been diagnosed with schizophrenia at age 17. They said they were “devastated and horrified” by their son’s actions. “To you he’s a monster,” said his father. “But to me he was a very sick boy.”
Globally, one out of every eight people report a mental illness. In Australia, one in five people experience a mental illness in their lifetime.
Mental illness and distress affects not only the person living with the condition, but family members and communities. As the prevalence of mental health problems grows, the flow-on effect to family members, including caregivers, and the impact on families as a unit, is also rising.
While every family is different, the words of the Cauchis draw attention to how families can experience distress, stress, fear, powerlessness, and still love, despite the challenges and trauma. How can they help a loved one? And who can they turn to for support?
The role of caregivers
Informal caregivers help others within the context of an existing relationship, such as a family member. The care they provide goes beyond the usual expectations or demands of such relationships.
Around 2.7 million Australians provide informal care. For almost a third of these the person’s primary medical diagnosis is psychological or psychiatric.
It has long been acknowledged that those supporting a family member with ongoing mental illness need support themselves.
In the 1980s, interest grew in caregiving dynamics within families of people grappling with mental health issues. Subsequent research recognised chronic health conditions not only affect the quality of life and wellbeing of the people experiencing them, but also impose burdens that reverberate within relationships, caregiving roles, and family dynamics over time.
Past studies have shown families of those diagnosed with chronic mental illness are increasingly forced to manage their own depression, experience elevated levels of emotional stress, negative states of mind and decreased overall mental health.
Conditions such as depression, anxiety disorders, bipolar disorder, and schizophrenia can severely impact daily functioning, relationships, and overall quality of life. Living with mental illness is often accompanied by a myriad of challenges. From stigma and discrimination to difficulty accessing adequate health care and support services. Patients and their families navigate a complex and often isolating journey.
The family is a system
The concept of family health acknowledges the physical and psychological wellbeing of a person is significantly affected by the family.
Amid these challenges, family support emerges as a beacon of hope. Research consistently demonstrates strong familial relationships and support systems play a pivotal role in mitigating the adverse effects of mental illness. Families provide emotional support, practical assistance, and a sense of belonging that are vital for people struggling with mental illness.
My recent research highlights the profound impact of mental illness on family dynamics, emphasising the resilience and endurance shown by participants. Families struggling with mental illness often experience heightened emotional fluctuations, with extreme highs and lows. The enduring nature of family caregiving entails both stress and adaptation over an extended period. Stress associated with caregiving and the demands on personal resources and coping mechanisms builds and builds.
Yet families I’ve interviewed find ways to live “a good life”. They prepare for the peaks and troughs, and show endurance and persistence. They make space for mental illness in their daily lives, describing how it spurs adaptation, acceptance and inner strength within the family unit.
When treating a person with mental illness, health practitioners need to consider the entire family’s needs and engage with family members. By fostering open and early dialogue and providing comprehensive support, health-care professionals can empower families to navigate the complexities of mental illness while fostering resilience and hope for the future. Family members express stories of an inner struggle, isolation and exhaustion.
Family bonds can be a cornerstone of wellbeing. Gorodenkoff/Shutterstock Shifting the focus
There is a pressing need for a shift in research priorities, from illness-centered perspectives to a strengths-based focus when considering families “managing” mental illness.
There is transformative potential in harnessing strengths to respond to challenges posed by mental illnesses, while also supporting family members.
For people facing mental health challenges, having loved ones who listen without judgement and offer empathy can alleviate feelings of despair. Beyond emotional support, families often serve as crucial caregivers, assisting with daily tasks, medication management and navigating the health-care system.
As the Cauchi family so painfully articulated, providing support for a family member with mental illness is intensely challenging. Research shows caregiver burnout, financial strain and strained relationships are common.
Health-care professionals should prioritise support for family members at an early stage. In Australia, there are various support options available for families living with mental illness. Carer Gateway provides information, support and access to services. Headspace offers mental health services and supports to young people and their families.
Beyond these national services, GPs, nurses, nurse practitioners and local community health centres are key to early conversations. Mental health clinics and hospitals often target family involvement in treatment plans.
While Australia has made strides in recognising the importance of family support, challenges persist. Access to services can vary based on geographic location and demand, leaving some families under-served or facing long wait times. And the level of funding and resources allocated to family-oriented mental health support often does not align with the demand or complexity of need.
In the realm of mental illness, family support serves as a lifeline for people navigating the complexities of their conditions.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Amanda Cole, Lead, Mental Health, Edith Cowan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: