What’s the difference between autism and Asperger’s disorder?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Swedish climate activist Greta Thunberg describes herself as having Asperger’s while others on the autism spectrum, such as Australian comedian Hannah Gatsby, describe themselves as “autistic”. But what’s the difference?
Today, the previous diagnoses of “Asperger’s disorder” and “autistic disorder” both fall within the diagnosis of autism spectrum disorder, or ASD.
Autism describes a “neurotype” – a person’s thinking and information-processing style. Autism is one of the forms of diversity in human thinking, which comes with strengths and challenges.
When these challenges become overwhelming and impact how a person learns, plays, works or socialises, a diagnosis of autism spectrum disorder is made.
Where do the definitions come from?
The Diagnostic and Statistical Manual of Mental Disorders (DSM) outlines the criteria clinicians use to diagnose mental illnesses and behavioural disorders.
Between 1994 and 2013, autistic disorder and Asperger’s disorder were the two primary diagnoses related to autism in the fourth edition of the manual, the DSM-4.
In 2013, the DSM-5 collapsed both diagnoses into one autism spectrum disorder.
How did we used to think about autism?
The two thinkers behind the DSM-4 diagnostic categories were Baltimore psychiatrist Leo Kanner and Viennese paediatrician Hans Asperger. They described the challenges faced by people who were later diagnosed with autistic disorder and Asperger’s disorder.
Kanner and Asperger observed patterns of behaviour that differed to typical thinkers in the domains of communication, social interaction and flexibility of behaviour and thinking. The variance was associated with challenges in adaptation and distress.

Roman Nerud/Shutterstock
Between the 1940s and 1994, the majority of those diagnosed with autism also had an intellectual disability. Clinicians became focused on the accompanying intellectual disability as a necessary part of autism.
The introduction of Asperger’s disorder shifted this focus and acknowledged the diversity in autism. In the DSM-4 it superficially looked like autistic disorder and Asperger’s disorder were different things, with the Asperger’s criteria stating there could be no intellectual disability or delay in the development of speech.
Today, as a legacy of the recognition of the autism itself, the majority of people diagnosed with autism spectrum disorder – the new term from the DSM-5 – don’t a have an accompanying intellectual disability.
What changed with ‘autism spectrum disorder’?
The move to autism spectrum disorder brought the previously diagnosed autistic disorder and Asperger’s disorder under the one new diagnostic umbrella term.
It made clear that other diagnostic groups – such as intellectual disability – can co-exist with autism, but are separate things.
The other major change was acknowledging communication and social skills are intimately linked and not separable. Rather than separating “impaired communication” and “impaired social skills”, the diagnostic criteria changed to “impaired social communication”.
The introduction of the spectrum in the diagnostic term further clarified that people have varied capabilities in the flexibility of their thinking, behaviour and social communication – and this can change in response to the context the person is in.
Why do some people prefer the old terminology?
Some people feel the clinical label of Asperger’s allowed a much more refined understanding of autism. This included recognising the achievements and great societal contributions of people with known or presumed autism.
The contraction “Aspie” played an enormous part in the shift to positive identity formation. In the time up to the release of the DSM-5, Tony Attwood and Carol Gray, two well known thinkers in the area of autism, highlighted the strengths associated with “being Aspie” as something to be proud of. But they also raised awareness of the challenges.
What about identity-based language?
A more recent shift in language has been the reclamation of what was once viewed as a slur – “autistic”. This was a shift from person-first language to identity-based language, from “person with autism spectrum disorder” to “autistic”.
The neurodiversity rights movement describes its aim to push back against a breach of human rights resulting from the wish to cure, or fundamentally change, people with autism.

Alex and Maria photo/Shutterstock
The movement uses a “social model of disability”. This views disability as arising from societies’ response to individuals and the failure to adjust to enable full participation. The inherent challenges in autism are seen as only a problem if not accommodated through reasonable adjustments.
However the social model contrasts itself against a very outdated medical or clinical model.
Current clinical thinking and practice focuses on targeted supports to reduce distress, promote thriving and enable optimum individual participation in school, work, community and social activities. It doesn’t aim to cure or fundamentally change people with autism.
A diagnosis of autism spectrum disorder signals there are challenges beyond what will be solved by adjustments alone; individual supports are also needed. So it’s important to combine the best of the social model and contemporary clinical model.
Andrew Cashin, Professor of Nursing, School of Health and Human Sciences, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Can a drug like Ozempic help treat addictions to alcohol, opioids or other substances?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (sold as Ozempic, Wegovy and Rybelsus) was initially developed to treat diabetes. It works by stimulating the production of insulin to keep blood sugar levels in check.
This type of drug is increasingly being prescribed for weight loss, despite the fact it was initially approved for another purpose. Recently, there has been growing interest in another possible use: to treat addiction.
Anecdotal reports from patients taking semaglutide for weight loss suggest it reduces their appetite and craving for food, but surprisingly, it also may reduce their desire to drink alcohol, smoke cigarettes or take other drugs.
But does the research evidence back this up?
Animal studies show positive results
Semaglutide works on glucagon-like peptide-1 receptors and is known as a “GLP-1 agonist”.
Animal studies in rodents and monkeys have been overwhelmingly positive. Studies suggest GLP-1 agonists can reduce drug consumption and the rewarding value of drugs, including alcohol, nicotine, cocaine and opioids.
Out team has reviewed the evidence and found more than 30 different pre-clinical studies have been conducted. The majority show positive results in reducing drug and alcohol consumption or cravings. More than half of these studies focus specifically on alcohol use.
However, translating research evidence from animal models to people living with addiction is challenging. Although these results are promising, it’s still too early to tell if it will be safe and effective in humans with alcohol use disorder, nicotine addiction or another drug dependence.
What about research in humans?
Research findings are mixed in human studies.
Only one large randomised controlled trial has been conducted so far on alcohol. This study of 127 people found no difference between exenatide (a GLP-1 agonist) and placebo (a sham treatment) in reducing alcohol use or heavy drinking over 26 weeks.
In fact, everyone in the study reduced their drinking, both people on active medication and in the placebo group.
However, the authors conducted further analyses to examine changes in drinking in relation to weight. They found there was a reduction in drinking for people who had both alcohol use problems and obesity.
For people who started at a normal weight (BMI less than 30), despite initial reductions in drinking, they observed a rebound increase in levels of heavy drinking after four weeks of medication, with an overall increase in heavy drinking days relative to those who took the placebo.
There were no differences between groups for other measures of drinking, such as cravings.
Some studies show a rebound increase in levels of heavy drinking. Deman/Shutterstock In another 12-week trial, researchers found the GLP-1 agonist dulaglutide did not help to reduce smoking.
However, people receiving GLP-1 agonist dulaglutide drank 29% less alcohol than those on the placebo. Over 90% of people in this study also had obesity.
Smaller studies have looked at GLP-1 agonists short-term for cocaine and opioids, with mixed results.
There are currently many other clinical studies of GLP-1 agonists and alcohol and other addictive disorders underway.
While we await findings from bigger studies, it’s difficult to interpret the conflicting results. These differences in treatment response may come from individual differences that affect addiction, including physical and mental health problems.
Larger studies in broader populations of people will tell us more about whether GLP-1 agonists will work for addiction, and if so, for whom.
How might these drugs work for addiction?
The exact way GLP-1 agonists act are not yet well understood, however in addition to reducing consumption (of food or drugs), they also may reduce cravings.
Animal studies show GLP-1 agonists reduce craving for cocaine and opioids.
This may involve a key are of the brain reward circuit, the ventral striatum, with experimenters showing if they directly administer GLP-1 agonists into this region, rats show reduced “craving” for oxycodone or cocaine, possibly through reducing drug-induced dopamine release.
Using human brain imaging, experimenters can elicit craving by showing images (cues) associated with alcohol. The GLP-1 agonist exenatide reduced brain activity in response to an alcohol cue. Researchers saw reduced brain activity in the ventral striatum and septal areas of the brain, which connect to regions that regulate emotion, like the amygdala.
In studies in humans, it remains unclear whether GLP-1 agonists act directly to reduce cravings for alcohol or other drugs. This needs to be directly assessed in future research, alongside any reductions in use.
Are these drugs safe to use for addiction?
Overall, GLP-1 agonists have been shown to be relatively safe in healthy adults, and in people with diabetes or obesity. However side effects do include nausea, digestive troubles and headaches.
And while some people are OK with losing weight as a side effect, others aren’t. If someone is already underweight, for example, this drug might not be suitable for them.
In addition, very few studies have been conducted in people with addictive disorders. Yet some side effects may be more of an issue in people with addiction. Recent research, for instance, points to a rare risk of pancreatitis associated with GLP-1 agonists, and people with alcohol use problems already have a higher risk of this disorder.
Other drugs treatments are currently available
Although emerging research on GLP-1 agonists for addiction is an exciting development, much more research needs to be done to know the risks and benefits of these GLP-1 agonists for people living with addiction.
In the meantime, existing effective medications for addiction remain under-prescribed. Only about 3% of Australians with alcohol dependence, for example, are prescribed medication treatments such as like naltrexone, acamprosate or disulfiram. We need to ensure current medication treatments are accessible and health providers know how to prescribe them.
Continued innovation in addiction treatment is also essential. Our team is leading research towards other individualised and effective medications for alcohol dependence, while others are investigating treatments for nicotine addiction and other drug dependence.
Read the other articles in The Conversation’s Ozempic series here.
Shalini Arunogiri, Addiction Psychiatrist, Associate Professor, Monash University; Leigh Walker, , Florey Institute of Neuroscience and Mental Health, and Roberta Anversa, , The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Mythbusting Moldy Food
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most Food Should Not Be Fuzzy
In yesterday’s newsletter, we asked you for your policy when it comes to mold on food (aside from intentional mold, e.g. blue cheese etc), and the responses were interesting:
- About 49% said “throw the whole thing away no matter what it is; it is dangerous”
- About 24% said “cut the mold off and eat the rest of whatever it is”
- The remainder were divided equally between “eat it all; keep the immune system on its toes” and “cut the mold off bread, but moldy animal products are dangerous”
So what does the science say?
Some molds are safe to eat: True or False?
True! We don’t think this is contentious so we’ll not spend much time on it, but just for the sake of being methodical: foods that are supposed to have mold on, including many kinds of cheese and even some kinds of cured meat (salami is an example; that powdery coating is mold).
We could give a big list of safe and unsafe molds, but that would be a list of names and let’s face it, they don’t introduce themselves by name.
However! The litmus test of “is it safe to eat” is:
Did you acquire it with this mold already in place and exactly as expected and advertised?
- If so, it is safe to eat (unless you have an allergy or such)
- If not, it is almost certainly not safe to eat
(more on why, later)
The “sniff test” is a good way to tell if moldy food is bad: True or False?
False. Very false. Because of how the sense of smell works.
You may feel like smell is a way of knowing about something at a distance, but the only way you can smell something is if particles of it are physically connecting with your olfactory receptors inside you. Yes, that has unfortunate implications about bathroom smells, but for now, let’s keep our attention in the kitchen.
If you sniff a moldy item of food, you will now have its mold spores inside your respiratory system. You absolutely do not want them there.
If we cut off the mold, the rest is safe to eat: True or False?
True or False, depending on what it is:
- Hard vegetables (e.g carrots, cabbage), and hard cheeses (e.g. Gruyère, Gouda) – cut off with an inch margin, and it should be safe
- Soft vegetables (e.g. tomatoes, and any vegetables that were hard but are now soft after cooking) – discard entirely; it is unsafe
- Anything else – discard entirely; it is unsafe
The reason for this is because in the case of the hard products mentioned, the mycelium roots of the mold cannot penetrate far.
In the case of the soft products mentioned, the surface mold is “the tip of the iceberg”, and the mycelium roots, which you will not usually be able to see, will penetrate the rest of it.
“Anything else” seems like quite a sweeping statement, but fruits, soft cheeses, yogurt, liquids, jams and jellies, cooked grains and pasta, meats, and yes, bread, are all things where the roots can penetrate deeply and easily. Regardless of you only being able to see a small amount, the whole thing is probably moldy.
The USDA has a handy downloadable factsheet:
Molds On Food: Are They Dangerous?
Eating a little mold is good for the immune system: True or False?
False, generally. There are of course countless types of mold, but not only are many of them pathogenic (mycotoxins), but also, a food that has mold will usually also have pathogenic bacteria along with the mold.
See for example: Occurrence, Toxicity, and Analysis of Major Mycotoxins in Food
Food poisoning will never make you healthier.
But penicillin is safe to eat: True or False?
False, and also penicillin is not the mold on your bread (or other foods).
Penicillin, an antibiotic* molecule, is produced by some species of Penicillium sp., a mold. There are hundreds of known species of Penicillium sp., and most of them are toxic, usually in multiple ways. Take for example:
Penicillium roqueforti PR toxin gene cluster characterization
*it is also not healthy to consume antibiotics unless it is seriously necessary. Antibiotics will wipe out most of your gut’s “good bacteria”, leaving you vulnerable. People have died from C. diff infections for this reason. So obviously, if you really need to take antibiotics, take them as directed, but if not, don’t.
See also: Four Ways Antibiotics Can Kill You
One last thing…
It may be that someone reading this is thinking “I’ve eaten plenty of mold, and I’m fine”. Or perhaps someone you tell about this will say that.
But there are two reasons this logic is flawed:
- Survivorship bias (like people who smoke and live to 102; we just didn’t hear from the 99.9% of people who smoke and die early)
- Being unaware of illness is not being absent of illness. Anyone who’s had an alarming diagnosis of something that started a while ago will know this, of course. It’s also possible to be “low-level ill” often and get used to it as a baseline for health. It doesn’t mean it’s not harmful for you.
Stay safe!
Share This Post
-
Is Cutting Calories The Key To Healthy Long Life?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Caloric Restriction with Optimal Nutrition
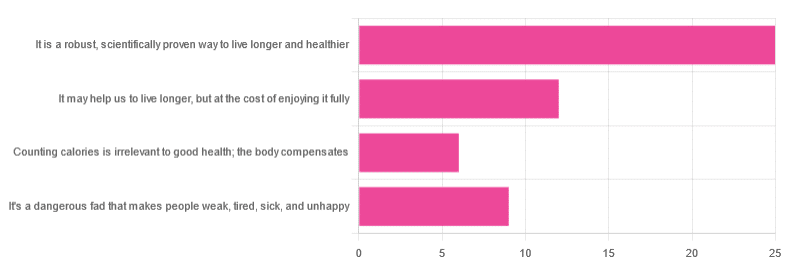
Yesterday, we asked you “What is your opinion of caloric restriction as a health practice?” and got the above-depicted, below-described spread of responses:
- 48% said “It is a robust, scientifically proven way to live longer and healthier”
- 23% said “It may help us to live longer, but at the cost of enjoying it fully”
- 17% said “It’s a dangerous fad that makes people weak, tired, sick, and unhealthy”
- 12% said “Counting calories is irrelevant to good health; the body compensates”
So… What does the science say?
A note on terms, first
“Caloric restriction” (henceforth: CR), as a term, sees scientific use to mean anything from a 25% reduction to a 50% reduction, compared to metabolic base rate.
This can also be expressed the other way around, “dropping to 60% of the metabolic base rate” (i.e., a 40% reduction).
Here we don’t have the space to go into much depth, so our policy will be: if research papers consider it CR, then so will we.
A quick spoiler, first
The above statements about CR are all to at least some degree True in one way or another.
However, there are very important distinctions, so let’s press on…
CR is a robust, scientifically proven way to live longer and healthier: True or False?
True! This has been well-studied and well-documented. There’s more science for this than we could possibly list here, but here’s a good starting point:
❝Calorie restriction (CR), a nutritional intervention of reduced energy intake but with adequate nutrition, has been shown to extend healthspan and lifespan in rodent and primate models.
Accumulating data from observational and randomized clinical trials indicate that CR in humans results in some of the same metabolic and molecular adaptations that have been shown to improve health and retard the accumulation of molecular damage in animal models of longevity.
In particular, moderate CR in humans ameliorates multiple metabolic and hormonal factors that are implicated in the pathogenesis of type 2 diabetes, cardiovascular diseases, and cancer, the leading causes of morbidity, disability and mortality❞
Source: Ageing Research Reviews | Calorie restriction in humans: an update
See also: Caloric restriction in humans reveals immunometabolic regulators of health span
We could devote a whole article (or a whole book, really) to this, but the super-short version is that it lowers the metabolic “tax” on the body and allows the body to function better for longer.
CR may help us to live longer, but at the cost of enjoying it fully: True or False?
True or False, contingently, depending on what’s important to you. And that depends on psychology as much as physiology, but it’s worth noting that there is often a selection bias in the research papers; people ill-suited to CR drop out of the studies and are not counted in the final data.
Also, relevant for a lot of our readers, most (human-based) studies recruit people over 18 and under 60. So while it is reasonable to assume the same benefits will be carried over that age, there is not nearly as much data for it.
Studies into CR and Health-Related Quality of Life (HRQoL) have been promising, and/but have caveats:
❝In non-obese adults, CR had some positive effects and no negative effects on HRQoL.❞
❝We do not know what degree of CR is needed to achieve improvements in HRQoL, but we do know it requires an extraordinary amount of support.
Therefore, the incentive to offer this intervention to a low-risk, normal or overweight individual is lacking and likely not sustainable in practice.❞
CR a dangerous fad that makes people weak, tired, sick, and unhealthy: True or False?
True if it is undertaken improperly, and/or without sufficient support. Many people will try CR and forget that the idea is to reduce metabolic load while still getting good nutrition, and focus solely on the calorie-counting.
So for example, if a person “saves” their calories for the day to have a night out in a bar where they drink their calories as alcohol, then this is going to be abysmal for their health.
That’s an extreme example, but lesser versions are seen a lot. If you save your calories for a pizza instead of a night of alcoholic drinks, then it’s not quite so woeful, but for example the nutrition-to-calorie ratio of pizza is typically not great. Multiply that by doing it as often as not, and yes, someone’s health is going to be in ruins quite soon.
Counting calories is irrelevant to good health; the body compensates: True or False?
True if by “good health” you mean weight loss—which is rarely, if ever, what we mean by “good health” here at 10almonds (unless we clarify such), but it’s a very common association and indeed, for some people it’s a health goal. You cannot sustainably and healthily lose weight by CR alone, especially if you’re not getting optimal nutrition.
Your body will notice that you are starving, and try to save you by storing as much fat as it can, amongst other measures that will similarly backfire (cortisol running high, energy running low, etc).
For short term weight loss though, yes, it’ll work. At a cost. That we don’t recommend.
❝By itself, decreasing calorie intake will have a limited short-term influence.❞
Source: Reducing Calorie Intake May Not Help You Lose Body Weight
See also…
❝Caloric restriction is a commonly recommended weight-loss method, yet it may result in short-term weight loss and subsequent weight regain, known as “weight cycling”, which has recently been shown to be associated with both poor sleep and worse cardiovascular health❞
Source: Dieting Behavior Characterized by Caloric Restriction
In summary…
Caloric restriction is a well-studied area of health science. We know:
- Practised well, it can extend not only lifespan, but also healthspan
- Practised well, it can improve mood, energy, sexual function, and the other things people fear losing
- Practised badly, it can be ruinous to the health—it is critical to practise caloric restriction with optimal nutrition.
- Practised badly, it can lead to unhealthy weight loss and weight regain
One final note…
If you’ve tried CR and hated it, and you practised it well (e.g., with optimal nutrition), then we recommend just not doing it.
You could also try intermittent fasting instead, for similar potential benefits. If that doesn’t work out either, then don’t do that either!
Sometimes, we’re just weird. It can often be because of a genetic or epigenetic quirk. There are usually workarounds, and/but not everything that’s right for most people will be right for all of us.
Take care!
Share This Post
Related Posts
-
Over-50s Physio: What My 5 Oldest Patients (Average Age 92) Do Right
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oftentimes, people of particularly advanced years will be asked their secret to longevity, and sometimes the answers aren’t that helpful because they don’t actually know, and ascribe it to some random thing. Will Harlow, the over-50s specialist physio, talks about the top 5 science-based things that his 5 oldest patients do, that enhances the healthy longevity that they are enjoying:
The Top 5’s Top 5
Here’s what they’re doing right:
Daily physical activity: all five patients maintain a consistent habit of daily exercise, which includes activities like exercise classes, home workouts, playing golf, or taking daily walks. They prioritize movement even when it’s difficult, rarely skipping a day unless something serious happened. A major motivator was the fear of losing mobility, as they had seen spouses, friends, or family members stop exercising and never start again.
Stay curious: a shared trait among the patients was their curiosity and eagerness to learn. They enjoy meeting new people, exploring new experiences, and taking on new challenges. Two of them attended the University of the Third Age to learn new skills, while another started playing bridge as a new hobby. The remaining two have recently made new friends. They all maintain a playful attitude, a good sense of humor, and aren’t afraid to fail or laugh at themselves.
Prioritize sleep (but not too much): the patients each average seven hours of sleep per night, aligning with research suggesting that 7–9 hours of sleep is ideal for health. They maintain consistent sleep and wake-up times, which contributes to their well-being. While they allow themselves short naps when needed, they avoid long afternoon naps to avoid disrupting their sleep patterns.
Spend time in nature: spending time outdoors is a priority for all five individuals. Whether through walking, gardening, or simply sitting on a park bench, they make it a habit to connect with nature. This aligns with studies showing that time spent in natural environments, especially near water, significantly reduces stress. When water isn’t accessible, green spaces still provide a beneficial boost to mental health.
Stick to a routine: the patients all value simple daily routines, such as enjoying an evening cup of tea, taking a daily walk, or committing to small gardening tasks. These routines offer mental and physical grounding, providing stability even when life becomes difficult sometimes. They emphasized the importance of keeping routines simple and manageable to ensure they could stick to them regardless of life’s challenges.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Top 8 Habits Of The Top 1% Healthiest Over-50s ← another approach to the same question, this time with a larger sample size, and/but many younger (than 90s) respondents.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
General Tso’s Chickpeas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A fiber-rich, heart-healthy take on a classic:
You will need
- 1 can chickpeas, drained
- ¾ cup vegetable stock; ideally you made this yourself from vegetable cuttings that you kept in the freezer for this purpose, but failing that, you should be able to get low-sodium stock cubes at your local supermarket.
- ¼ cup arrowroot starch (cornstarch will do at a pinch, but arrowroot is better and has no flavor of its own)
- 3 tbsp coconut oil
- 2 tbsp grated fresh ginger
- ¼ bulb garlic, minced
- 2 tbsp honey (or maple syrup if you prefer, and if you don’t like sweetness, reduce this to 1 tbsp or even omit entirely, though it won’t be quite so “General Tso” if you do, but it’s your meal!)
- 2 tbsp tomato paste
- 2 tsp hot sauce
- 1 tsp black pepper, coarse ground
- 3 green onions, sliced
Method
(we suggest you read everything at least once before doing anything)
1) Coat the chickpeas in the arrowroot starch by tossing them together in a bowl
2) Heat the coconut oil in a skillet on a medium-high heat, and when hot, add the chickpeas, stirring for 3 minutes
3) Add the remaining ingredients in the order we gave (except the vegetable stock, which goes in last), stirring for 5 more minutes, or until the sauce thickens
4) Serve with the carb of your choice; we recommend our Tasty Versatile Rice Recipe
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Honey vs Maple Syrup – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Easy Quinoa Falafel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Falafel is a wonderful snack or accompaniment to a main, and if you’ve only had shop-bought, you’re missing out. Plus, with this quinoa-based recipe, it’s almost impossible to accidentally make them dry.
You will need
- 1 cup cooked quinoa
- 1 cup chopped fresh parsley
- ½ cup wholewheat breadcrumbs (or rye breadcrumbs if you’re avoiding wheat/gluten)
- 1 can chickpeas, drained
- 4 green onions, chopped
- ½ bulb garlic, minced
- 2 tbsp extra virgin olive oil, plus more for frying
- 2 tbsp tomato paste
- 1 tbsp apple cider vinegar
- 2 tsp nutritional yeast
- 2 tsp ground cumin
- 1 tsp red pepper flakes
- 1 tsp black pepper, coarse ground
- 1 tsp dried thyme
- ½ tsp MSG or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Blend all the ingredients in a food processor until it has an even, but still moderately coarse, texture.
2) Shape into 1″ balls, and put them in the fridge to chill for about 20 minutes.
3) Fry the balls over a medium-high heat until evenly browned—just do a few at a time, taking care to not overcrowd the pan.
4) Serve! Great with salad, hummus, and other such tasty healthy snack items:
Enjoy!
Want to learn more?
For those interested in more of what we have going on today:
- Cilantro vs Parsley – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
- What Matters Most For Your Heart?
- An Apple (Cider Vinegar) A Day…
- Hero Homemade Hummus Recipe ← perfect accompaniment!
- Tasty Tabbouleh with Tahini Recipe ← also a great option!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: