How they did it: STAT reporters expose how ailing seniors suffer when Medicare Advantage plans use algorithms to deny care
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a call with a long-time source, what stood out most to STAT reporters Bob Herman and Casey Ross was just how viscerally frustrated and angry the source was about an algorithm used by insurance companies to decide how long patients should stay in a nursing home or rehab facility before being sent home.
The STAT stories had a far-reaching impact:
- The U.S. Senate Committee on Homeland Security and Government Affairs took a rare step of launching a formal investigation into the use of algorithms by the country’s three largest Medicare Advantage insurers.
- Thirty-two House members urged the Centers for Medicare and Medicaid Services to increase the oversight of algorithms that health insurers use to make coverage decisions.
- In a rare step, CMS launched its own investigation into UnitedHealth. It also stiffened its regulations on the use of proprietary algorithms and introduced plans to audit denials across Medicare Advantage plans in 2024.
- Based on STAT’s reporting, Medicare Advantage beneficiaries filed two class-action lawsuits against UnitedHealth and its NaviHealth subsidiary, the maker of the algorithm, and against Humana, another major health insurance company that was also using the algorithm.
- Amid scrutiny, UnitedHealth renamed NaviHealth.
The companies never allowed an on-the-record interview with their executives, but they acknowledged that STAT’s reporting was true, according to the news organization.
Ross and Herman spoke with The Journalist’s Resource about their project and shared the following eight tips.
1. Search public comments on proposed federal rules to find sources.
Herman and Ross knew that the Centers for Medicare and Medicaid Services had put out a request for public comments, asking stakeholders within the Medicare Advantage industry how the system could improve.
There are two main ways to get Medicare coverage: original Medicare, which is a fee-for-service health plan, and Medicare Advantage, which is a type of Medicare health plan offered by private insurance companies that contract with Medicare. Medicare Advantage plans have increasingly become popular in recent years.
Under the Social Security Act, the public has the opportunity to submit comments on Medicare’s proposed national coverage determinations. CMS uses public comments to inform its proposed and final decisions. It responds in detail to all public comments when issuing a final decision.
The reporters began combing through hundreds of public comments attached to a proposed Medicare Advantage rule that was undergoing federal review. NaviHealth, the UnitedHealth subsidiary and the maker of the algorithm, came up in many of the comments, which include the submitters’ information.
“These are screaming all-caps comments to federal regulators about YOU NEED TO SOMETHING ABOUT THIS BECAUSE IT’S DISGUSTING,” Ross says.
“The federal government is proposing rules and regulations all the time,” adds Herman, STAT’s business of health care reporter. “If someone’s going to take the time and effort to comment on them, they must have at least some knowledge of what’s going on. It’s just a great tool for any journalist to use to figure out more and who to contact.”
The reporters also found several attorneys who had complained in the comments. They began reaching out to them, eventually gaining access to confidential documents and intermediaries who put them in touch with patients to show the human impact of the algorithm.
2. Harness the power of the reader submission box.
At the suggestion of an editor, the reporters added a reader submission box at the bottom of their first story, asking them to share their own experiences with Medicare Advantage denials.
The floodgates opened. Hundreds of submissions arrived.
By the end of their first story, Herman and Ross had confidential records and some patients, but they had no internal sources in the companies they were investigating, including Navihealth. The submission box led them to their first internal source.
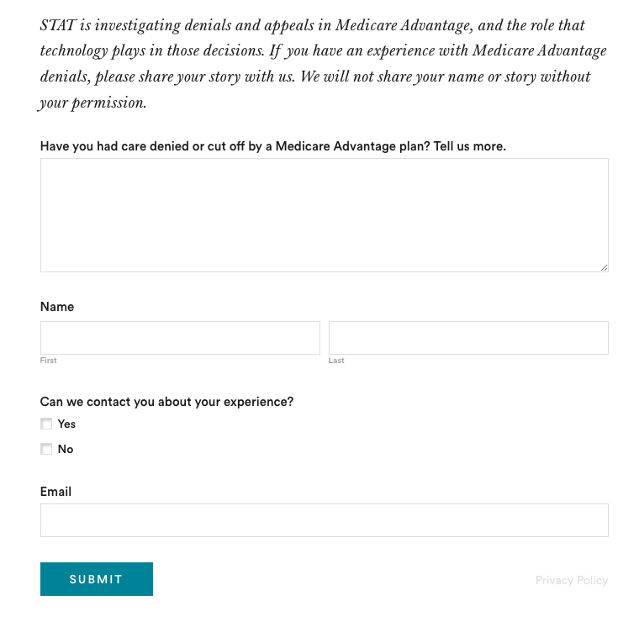
The journalists also combed through LinkedIn and reached out to former and current employees, but the response rate was much lower than what they received via the submission box.
The submission box “is just right there,” Herman says. “People who would want to reach out to us can do it right then and there after they read the story and it’s fresh in their minds.”
3. Mine podcasts relevant to your story.
The reporters weren’t sure if they could get interviews with some of the key figures in the story, including Tom Scully, the former head of the Centers for Medicare and Medicaid Services who drew up the initial plans for NaviHealth years before UnitedHealth acquired it.
But Herman and another colleague had written previously about Scully’s private equity firm and they had found a podcast where he talked about his work. So Herman went back to the podcast — where he discovered Scully had also discussed NaviHealth.
The reporters also used the podcast to get Scully on the phone for an interview.
“So we knew we had a good jumping off point there to be like, ‘OK, you’ve talked about NaviHealth on a podcast, let’s talk about this,’” Herman says. “I think that helped make him more willing to speak with us.”
4. When covering AI initiatives, proceed with caution.
“A source of mine once said to me, ‘AI is not magic,’” Ross says. “People need to just ask questions about it because AI has this aura about it that it’s objective, that it’s accurate, that it’s unquestionable, that it never fails. And that is not true.”
AI is not a neutral, objective machine, Ross says. “It’s based on data that’s fed into it and people need to ask questions about that data.”
He suggests several questions to ask about the data behind AI tools:
- Where does the data come from?
- Who does it represent?
- How is this tool being applied?
- Do the people to whom the tool is being applied match the data on which it was trained? “If racial groups or genders or age of economic situations are not adequately represented in the training set, then there can be an awful lot of bias in the output of the tool and how it’s applied,” Ross says.
- How is the tool applied within the institution? Are people being forced to forsake their judgment and their own ability to do their jobs to follow the algorithm?
5. Localize the story.
More than half of all Medicare beneficiaries have Medicare Advantage and there’s a high likelihood that there are multiple Medicare Advantage plans in every county across the nation.
“So it’s worth looking to see how Medicare Advantage plans are growing in your area,” Herman says.
Finding out about AI use will most likely rely on shoe-leather reporting of speaking with providers, nursing homes and rehab facilities, attorneys and patients in your community, he says. Another source is home health agencies, which may be caring for patients who were kicked out of nursing homes and rehab facilities too soon because of a decision by an algorithm.
The anecdote that opens their first story involves a small regional health insurer in Wisconsin, which was using NaviHealth and a contractor to manage post-acute care services, Ross says.
“It’s happening to people in small communities who have no idea that this insurer they’ve signed up with is using this tool made by this other company that operates nationally,” Ross says.
There are also plenty of other companies like NaviHealth that are being used by Medicare Advantage plans, Herman says. “So it’s understanding which Medicare Advantage plans are being sold in your area and then which post-acute management companies they’re using,” he adds.
Some regional insurers have online documents that show which contractors they use to evaluate post-acute care services.
6. Get familiar with Medicare’s appeals databases
Medicare beneficiaries can contest Medicare Advantage denials through a five-stage process, which can last months to years. The appeals can be filed via the Office of Medicare Hearings and Appeals.
“Between 2020 and 2022, the number of appeals filed to contest Medicare Advantage denials shot up 58%, with nearly 150,000 requests to review a denial filed in 2022, according to a federal database,” Ross and Herman write in their first story. “Federal records show most denials for skilled nursing care are eventually overturned, either by the plan itself or an independent body that adjudicates Medicare appeals.”
There are several sources to find appeals data. Be mindful that the cases themselves are not public to protect patient privacy, but you can find the number of appeals filed and the rationale for decisions.
CMS has two quality improvement organizations, or QIOs, Livanta and Kepro, which are required to file free, publicly-available annual reports, about the cases they handle, Ross says.
Another company, Maximus, a Quality Improvement Contractor, also files reports on prior authorization cases it adjudicates for Medicare. The free annual reports include data on raw numbers of cases and basic information about the percentage denials either overturned or upheld on appeal, Ross explains.
CMS also maintains its own database on appeals for Medicare Part C (Medicare Advantage plans) and Part D, which covers prescription drugs, although the data is not complete, Ross explains.
7. Give your editor regular updates.
“Sprinkle the breadcrumbs in front of your editors,” Ross says.
“If you wrap your editors in the process, you’re more likely to be able to get to the end of [the story] before they say, ‘That’s it! Give me your copy,’” Ross says.
8. Get that first story out.
“You don’t have to know everything before you write that first story,” Ross says. “Because with that first story, if it has credibility and it resonates with people, sources will come forward and sources will continue to come forward.”
Read the stories
Denied by AI: How Medicare Advantage plans use algorithms to cut off care for seniors in need
UnitedHealth pushed employees to follow an algorithm to cut off Medicare patients’ rehab care
UnitedHealth used secret rules to restrict rehab care for seriously ill Medicare Advantage patients
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Relieve GERD and Acid Reflux with Stretches and Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Looking for relief from GERD or acid reflux? Today we’re featuring an amazing video by Dr. Jo, packed with stretches and exercises designed to ease those symptoms.
Here’s a quick rundown, in case you don’t have time to watch the whole video.
If you’re not familiar with GERD, you can find our simple explanation of GERD here. Or, if you’re on the other end of the spectrum and want to do a deeper dive on the topic, we reviewed a great book on the topic).
1. Mobilize Your SEM Muscle
The sternocleidomastoid (SEM) muscle, if tight, can aggravate acid reflux. Dr. Jo shows how to gently mobilize this muscle by turning your head while holding the SEM in place. It’s simple but effective.
2. Portrait Pose Stretch
Stretch out that SEM with the Portrait Pose. Place your hand on your collarbone, turn your head away, side bend, and look up. Hold for 30 seconds. You’ll feel the tension melting away.
3. Seated Cat-Cow Motion
Open up your stomach area with this easy exercise. Sit down, roll your body forward, arch your back (Cow), then curl your spine and tuck your chin (Cat). Alternate for 30 seconds and feel the difference.
4. Quadruped Cat-Cow with Breathing
Similar to the seated cat-cow, the quadruped cat-cow focuses on flexing the lower spine whilst on all fours. Bonus tip: focus on deep belly breathing during the exercise. This helps improve digestion and ease reflux symptoms.
5. Exaggerated Pelvic Tilt
Lie on your back and tilt your pelvis back and forth. This loosens up the abdominal area and helps everything flow better.
6. Trunk Rotation
Lie down, bend your knees, and rotate them to one side. Hold for 30 seconds, then switch sides. It’s a great way to relax and stretch your abdominal muscles.
We know this is a quick overview (sorry if it seems rushed!), but if you have a few more minutes on your hand you can watch the whole video below.
Feel better soon! And if you have any favorite tips or videos to share, email us at 10almonds.
Share This Post
-
How we diagnose and define obesity is set to change – here’s why, and what it means for treatment
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Obesity is linked to many common diseases, such as type 2 diabetes, heart disease, fatty liver disease and knee osteoarthritis.
Obesity is currently defined using a person’s body mass index, or BMI. This is calculated as weight (in kilograms) divided by the square of height (in metres). In people of European descent, the BMI for obesity is 30 kg/m² and over.
But the risk to health and wellbeing is not determined by weight – and therefore BMI – alone. We’ve been part of a global collaboration that has spent the past two years discussing how this should change. Today we publish how we think obesity should be defined and why.
As we outline in The Lancet, having a larger body shouldn’t mean you’re diagnosed with “clinical obesity”. Such a diagnosis should depend on the level and location of body fat – and whether there are associated health problems.
World Obesity Federation What’s wrong with BMI?
The risk of ill health depends on the relative percentage of fat, bone and muscle making up a person’s body weight, as well as where the fat is distributed.
Athletes with a relatively high muscle mass, for example, may have a higher BMI. Even when that athlete has a BMI over 30 kg/m², their higher weight is due to excess muscle rather than excess fatty tissue.
Some athletes have a BMI in the obesity category. Tima Miroshnichenko/Pexels People who carry their excess fatty tissue around their waist are at greatest risk of the health problems associated with obesity.
Fat stored deep in the abdomen and around the internal organs can release damaging molecules into the blood. These can then cause problems in other parts of the body.
But BMI alone does not tell us whether a person has health problems related to excess body fat. People with excess body fat don’t always have a BMI over 30, meaning they are not investigated for health problems associated with excess body fat. This might occur in a very tall person or in someone who tends to store body fat in the abdomen but who is of a “healthy” weight.
On the other hand, others who aren’t athletes but have excess fat may have a high BMI but no associated health problems.
BMI is therefore an imperfect tool to help us diagnose obesity.
What is the new definition?
The goal of the Lancet Diabetes & Endocrinology Commission on the Definition and Diagnosis of Clinical Obesity was to develop an approach to this definition and diagnosis. The commission, established in 2022 and led from King’s College London, has brought together 56 experts on aspects of obesity, including people with lived experience.
The commission’s definition and new diagnostic criteria shifts the focus from BMI alone. It incorporates other measurements, such as waist circumference, to confirm an excess or unhealthy distribution of body fat.
We define two categories of obesity based on objective signs and symptoms of poor health due to excess body fat.
1. Clinical obesity
A person with clinical obesity has signs and symptoms of ongoing organ dysfunction and/or difficulty with day-to-day activities of daily living (such as bathing, going to the toilet or dressing).
There are 18 diagnostic criteria for clinical obesity in adults and 13 in children and adolescents. These include:
- breathlessness caused by the effect of obesity on the lungs
- obesity-induced heart failure
- raised blood pressure
- fatty liver disease
- abnormalities in bones and joints that limit movement in children.
2. Pre-clinical obesity
A person with pre-clinical obesity has high levels of body fat that are not causing any illness.
People with pre-clinical obesity do not have any evidence of reduced tissue or organ function due to obesity and can complete day-to-day activities unhindered.
However, people with pre-clinical obesity are generally at higher risk of developing diseases such as heart disease, some cancers and type 2 diabetes.
What does this mean for obesity treatment?
Clinical obesity is a disease requiring access to effective health care.
For those with clinical obesity, the focus of health care should be on improving the health problems caused by obesity. People should be offered evidence-based treatment options after discussion with their health-care practitioner.
Treatment will include management of obesity-associated complications and may include specific obesity treatment aiming at decreasing fat mass, such as:
- support for behaviour change around diet, physical activity, sleep and screen use
- obesity-management medications to reduce appetite, lower weight and improve health outcomes such as blood glucose (sugar) and blood pressure
- metabolic bariatric surgery to treat obesity or reduce weight-related health complications.
Treatment for clinical obesity may include support for behaviour change. Shutterstock/shurkin_son Should pre-clinical obesity be treated?
For those with pre-clinical obesity, health care should be about risk-reduction and prevention of health problems related to obesity.
This may require health counselling, including support for health behaviour change, and monitoring over time.
Depending on the person’s individual risk – such as a family history of disease, level of body fat and changes over time – they may opt for one of the obesity treatments above.
Distinguishing people who don’t have illness from those who already have ongoing illness will enable personalised approaches to obesity prevention, management and treatment with more appropriate and cost-effective allocation of resources.
What happens next?
These new criteria for the diagnosis of clinical obesity will need to be adopted into national and international clinical practice guidelines and a range of obesity strategies.
Once adopted, training health professionals and health service managers, and educating the general public, will be vital.
Reframing the narrative of obesity may help eradicate misconceptions that contribute to stigma, including making false assumptions about the health status of people in larger bodies. A better understanding of the biology and health effects of obesity should also mean people in larger bodies are not blamed for their condition.
People with obesity or who have larger bodies should expect personalised, evidence-based assessments and advice, free of stigma and blame.
Louise Baur, Professor, Discipline of Child and Adolescent Health, University of Sydney; John B. Dixon, Adjunct Professor, Iverson Health Innovation Research Institute, Swinburne University of Technology; Priya Sumithran, Head of the Obesity and Metabolic Medicine Group in the Department of Surgery, School of Translational Medicine, Monash University, and Wendy A. Brown, Professor and Chair, Monash University Department of Surgery, School of Translational Medicine, Alfred Health, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Sugar, Hazelnuts, Books & Brains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Each Thursday, we respond to subscriber questions and requests! If it’s something small, we’ll answer it directly; if it’s something bigger, we’ll do a main feature in a follow-up day instead!
So, no question/request to big or small; they’ll just get sorted accordingly
Remember, you can always hit reply to any of our emails, or use the handy feedback widget at the bottom. We always look forward to hearing from you!
Q: Interesting info, however, I drink hazelnut milk LOL so would have liked a review of that. But now I want to give hemp and pea milks a try. Thanks
Aww! Here then just for you, is a quick rundown…
- Pros: high in protein¹, vitamin B, and vitamin E
- Cons: high in fat², low in calcium
¹Compared head-to-head with almond milk for example, it has double the protein (but also double the calories)
²However, is also has been found to lower LDL (bad) cholesterol (and incidentally, also reduce inflammation), and in a later systematic review, it was found to not correlate to weight gain, despite its high calorie-content.
If you don’t already, and would like to try making your own…
Click here for step-by-step instructions to make your own hazelnut milk! (very simple)
Q: Wondering if you can evaluate CLA and using it to assist with weight loss. Thanks
Will do! (Watch this space)
Q: What’s the process behind the books you recommend? You seem to have a limitless stream of recommendations
We do our best!
The books we recommend are books that…
- are on Amazon—it makes things tidy, consistent, and accessible. And if you end up buying one of the books, we get a small affiliate commission*.
- we have read—we would say “obviously”, but you might be surprised how many people write about books without having read them.
- pertain in at least large part to health and/or productivity.
- are written by humans—bookish people (and especially Kindle Unlimited users) may have noticed lately that there are a lot of low quality AI-written books flooding the market, sometimes with paid 5-star reviews to bolster them. It’s frustrating, but we can tell the difference and screen those out.
- are of a certain level of quality. They don’t have to be “top 5 desert-island books”, because well, there’s one every day and the days keep coming. But they do have to genuinely deliver the value that we describe, and merit a sincere recommendation.
- are varied—we try to not give a run of “samey” books one after another. We will sometimes review a book that covers a topic another previously-reviewed book did, but it must have something about it that makes it different. It may be a different angle or a different writing style, but it needs something to set it apart.
*this is from Amazon and isn’t product-specific, so this is not affecting our choice of what books to review at all—just that they will be books that are available on Amazon.
Q: Great video on dopamine. Thumbs up on the book recommendation. Would you please consider doing a piece or two on inflammation? I live with Lupus and it is a constant struggle. Thanks for the awesome work you do. Have an excellent day.
Great suggestion! We will do that, and thank you for the kind words!
Q: Why is your newsletter called 10almonds? Maybe I missed it in the intro email, but my curiosity wants to know the significance. Thanks!”
It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was online… So, calling ourselves 10almonds was a bit of a tongue-in-cheek reference to that story… but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
Related Posts
-
Freekeh Tomato Feast
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fiber-dense freekeh stars in this traditional Palestinian dish, and the whole recipe is very gut-healthy, not to mention delicious and filling, as well as boasting generous amounts of lycopene and other phytonutrients:
You will need
- 1 cup dried freekeh (if avoiding gluten, substitute a gluten-free grain, or pseudograin such as buckwheat; if making such a substitution, then also add 1 tbsp nutritional yeast—for the flavor as well as the nutrients)
- 1 medium onion, thinly sliced
- 1 2oz can anchovies (if vegan/vegetarian, substitute 1 can kimchi)
- 1 14oz can cherry tomatoes
- 1 cup halved cherry tomatoes, fresh
- ½ cup black olives, pitted
- 1 5oz jar roasted peppers, chopped
- ½ bulb garlic, thinly sliced
- 2 tsp black pepper
- 1 tsp chili flakes
- 1 sprig fresh thyme
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Place a heavy-based (cast iron, if you have it) sauté pan over a medium heat. Add some olive oil, then the onion, stirring for about 5 minutes.
2) Add the anchovies, herbs and spices (including the garlic), and stir well to combine. The anchovies will probably soon melt into the onion; that’s fine.
3) Add the canned tomatoes (but not the fresh), followed by the freekeh, stirring well again to combine.
4) Add 2 cups boiling water, and simmer with the lid on for about 40 minutes. Stir occasionally and check the water isn’t getting too low; top it up if it’s getting dry and the freekeh isn’t tender yet.
5) Add the fresh chopped cherry tomatoes and the chopped peppers from the jar, as well as the olives. Stir for just another 2 minutes, enough to let the latest ingredients warm through.
6) Serve, adding a garnish if you wish:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Eat More (Of This) For Lower Blood Pressure
- Making Friends With Your Gut (You Can Thank Us Later)
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What will aged care look like for the next generation? More of the same but higher out-of-pocket costs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged care financing is a vexed problem for the Australian government. It is already underfunded for the quality the community expects, and costs will increase dramatically. There are also significant concerns about the complexity of the system.
In 2021–22 the federal government spent A$25 billion on aged services for around 1.2 million people aged 65 and over. Around 60% went to residential care (190,000 people) and one-third to home care (one million people).
The final report from the government’s Aged Care Taskforce, which has been reviewing funding options, estimates the number of people who will need services is likely to grow to more than two million over the next 20 years. Costs are therefore likely to more than double.
The taskforce has considered what aged care services are reasonable and necessary and made recommendations to the government about how they can be paid for. This includes getting aged care users to pay for more of their care.
But rather than recommending an alternative financing arrangement that will safeguard Australians’ aged care services into the future, the taskforce largely recommends tidying up existing arrangements and keeping the status quo.
No Medicare-style levy
The taskforce rejected the aged care royal commission’s recommendation to introduce a levy to meet aged care cost increases. A 1% levy, similar to the Medicare levy, could have raised around $8 billion a year.
The taskforce failed to consider the mix of taxation, personal contributions and social insurance which are commonly used to fund aged care systems internationally. The Japanese system, for example, is financed by long-term insurance paid by those aged 40 and over, plus general taxation and a small copayment.
Instead, the taskforce puts forward a simple, pragmatic argument that older people are becoming wealthier through superannuation, there is a cost of living crisis for younger people and therefore older people should be required to pay more of their aged care costs.
Separating care from other services
In deciding what older people should pay more for, the taskforce divided services into care, everyday living and accommodation.
The taskforce thought the most important services were clinical services (including nursing and allied health) and these should be the main responsibility of government funding. Personal care, including showering and dressing were seen as a middle tier that is likely to attract some co-payment, despite these services often being necessary to maintain independence.
The task force recommended the costs for everyday living (such as food and utilities) and accommodation expenses (such as rent) should increasingly be a personal responsibility.
Aged care users will pay more of their share for cooking and cleaning.
Lizelle Lotter/ShutterstockMaking the system fairer
The taskforce thought it was unfair people in residential care were making substantial contributions for their everyday living expenses (about 25%) and those receiving home care weren’t (about 5%). This is, in part, because home care has always had a muddled set of rules about user co-payments.
But the taskforce provided no analysis of accommodation costs (such as utilities and maintenance) people meet at home compared with residential care.
To address the inefficiencies of upfront daily fees for packages, the taskforce recommends means testing co-payments for home care packages and basing them on the actual level of service users receive for everyday support (for food, cleaning, and so on) and to a lesser extent for support to maintain independence.
It is unclear whether clinical and personal care costs and user contributions will be treated the same for residential and home care.
Making residential aged care sustainable
The taskforce was concerned residential care operators were losing $4 per resident day on “hotel” (accommodation services) and everyday living costs.
The taskforce recommends means tested user contributions for room services and everyday living costs be increased.
It also recommends that wealthier older people be given more choice by allowing them to pay more (per resident day) for better amenities. This would allow providers to fully meet the cost of these services.
Effectively, this means daily living charges for residents are too low and inflexible and that fees would go up, although the taskforce was clear that low-income residents should be protected.
Moving from buying to renting rooms
Currently older people who need residential care have a choice of making a refundable up-front payment for their room or to pay rent to offset the loans providers take out to build facilities. Providers raise capital to build aged care facilities through equity or loan financing.
However, the taskforce did not consider the overall efficiency of the private capital market for financing aged care or alternative solutions.
Instead, it recommended capital contributions be streamlined and simplified by phasing out up-front payments and focusing on rental contributions. This echoes the royal commission, which found rent to be a more efficient and less risky method of financing capital for aged care in private capital markets.
It’s likely that in a decade or so, once the new home care arrangements are in place, there will be proportionally fewer older people in residential aged care. Those who do go are likely to be more disabled and have greater care needs. And those with more money will pay more for their accommodation and everyday living arrangements. But they may have more choice too.
Although the federal government has ruled out an aged care levy and changes to assets test on the family home, it has yet to respond to the majority of the recommendations. But given the aged care minister chaired the taskforce, it’s likely to provide a good indication of current thinking.
Hal Swerissen, Emeritus Professor, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fruit, Fiber, & Leafy Greens… On A Low-FODMAP Diet!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fiber For FODMAP-Avoiders
First, let’s quickly cover: what are FODMAPs?
FODMAPs are fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
In plainer English: they’re carbohydrates that are resistant to digestion.
This is, for most people most of the time, a good thing, for example:
When Is A Fiber Not A Fiber? When It’s A Resistant Starch.
Not for everyone…
However, if you have inflammatory bowel syndrome (IBS), including ulcerative colitis, Crohn’s disease, or similar, then suddenly a lot of common dietary advice gets flipped on its head:
While digestion-resistant carbohydrates making it to the end parts of our digestive tract are good for our bacteria there, in the case of people with IBS or similar, it can be a bit too good for our bacteria there.
Which can mean gas (a natural by-product of bacterial respiration) accumulation, discomfort, water retention (as the pseudo-fiber draws water in and keeps it), and other related symptoms, causing discomfort, and potentially disease such as diarrhea.
Again: for most people this is not so (usually: quite the opposite; resistant starches improve things down there), but for those for whom it’s a thing, it’s a Big Bad Thing™.
Hold the veg? Hold your horses.
A common knee-jerk reaction is “I will avoid fruit and veg, then”.
Superficially, this can work, as many fruit & veg are high in FODMAPs (as are fermented dairy products, by the way).
However, a diet free from fruit and veg is not going to be healthy in any sustainable fashion.
There are, however, options for low-FODMAP fruit & veg, such as:
Fruits: bananas (if not overripe), kiwi, grapefruit, lemons, limes, melons, oranges, passionfruit, strawberries
Vegetables: alfalfa, bell peppers, bok choy, carrots, celery, cucumbers, eggplant, green beans, kale, lettuce, olives, parsnips, potatoes (and sweet potatoes, yams etc), radishes, spinach, squash, tomatoes*, turnips, zucchini
*our stance: botanically it’s a fruit, but culinarily it’s a vegetable.
For more on the science of this, check out:
Strategies for Producing Low FODMAPs Foodstuffs: Challenges and Perspectives ← table 2 is particularly informative when it comes to the above examples, and table 3 will advise about…
Bonus
Grains: oats, quinoa, rice, tapioca
…and wheat if the conditions in table 3 (linked above) are satisfied
(worth mentioning since grains also get a bad press when it comes to IBS, but that’s mostly because of wheat)
See also: Gluten: What’s The Truth?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: