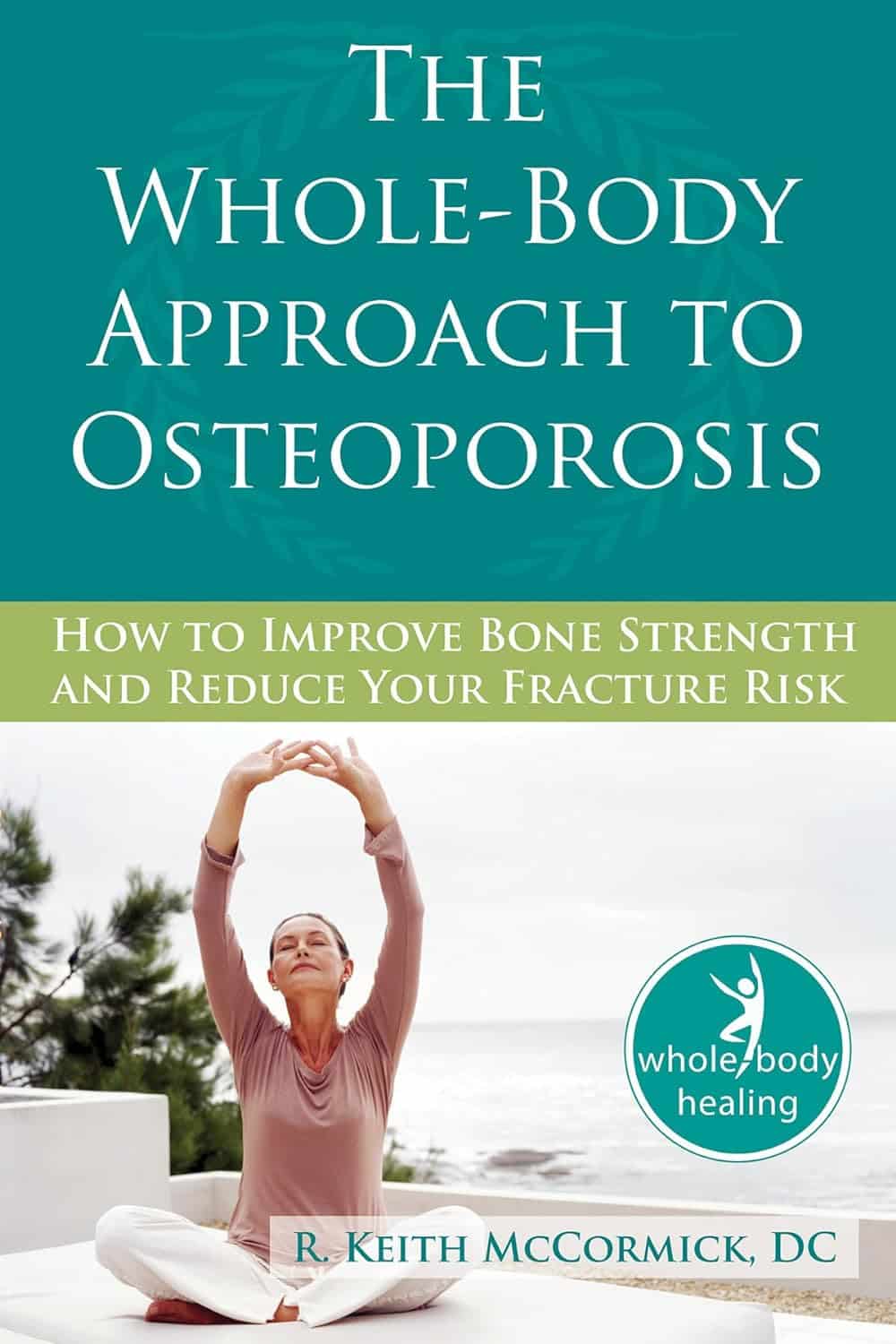
The Whole-Body Approach to Osteoporosis – by Keith McCormick
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably already know to get enough calcium and vitamin D, and do some resistance training. What does this book offer beyond that advice?
It’s pretty comprehensive, as it turns out. It covers the above, plus the wide range of medications available, what supplements help or harm or just don’t have enough evidence either way yet, things like that.
Amongst the most important offerings are the signs and symptoms that can help monitor your bone health (things you can do at home! Like examinations of your fingernails, hair, skin, tongue, and so forth, that will reveal information about your internal biochemical make-up), as well as what lab tests to ask for. Which is important, as osteoporosis is one of those things whereby we often don’t learn something is wrong until it’s too late.
The author is a chiropractor, which doesn’t always have a reputation as the most robustly science-based of physical therapy options, but he…
- doesn’t talk about chiropractic
- did confer with a flock of experts (osteopaths, nutritionists, etc) to inform/check his work
- does refer consistently to good science, and explains it well
- includes 16 pages of academic references, and yes, they are very reputable publications
Bottom line: this one really does give what the subtitle promises: a whole body approach to avoiding (or reversing) osteoporosis.
Click here to check out The Whole Body Approach To Osteoporosis; sooner is better than later!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Long-Covid Patients Are Frustrated That Federal Research Hasn’t Found New Treatments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Erica Hayes, 40, has not felt healthy since November 2020 when she first fell ill with covid.
Hayes is too sick to work, so she has spent much of the last four years sitting on her beige couch, often curled up under an electric blanket.
“My blood flow now sucks, so my hands and my feet are freezing. Even if I’m sweating, my toes are cold,” said Hayes, who lives in Western Pennsylvania. She misses feeling well enough to play with her 9-year-old son or attend her 17-year-old son’s baseball games.
Along with claiming the lives of 1.2 million Americans, the covid-19 pandemic has been described as a mass disabling event. Hayes is one of millions of Americans who suffer from long covid. Depending on the patient, the condition can rob someone of energy, scramble the autonomic nervous system, or fog their memory, among many other http://symptoms.in/ addition to the brain fog and chronic fatigue, Hayes’ constellation of symptoms includes frequent hives and migraines. Also, her tongue is constantly swollen and dry.
“I’ve had multiple doctors look at it and tell me they don’t know what’s going on,” Hayes said about her tongue.
Estimates of prevalence range considerably, depending on how researchers define long covid in a given study, but the Centers for Disease Control and Prevention puts it at 17 million adults.
Despite long covid’s vast reach, the federal government’s investment in researching the disease — to the tune of $1.15 billion as of December — has so far failed to bring any new treatments to market.
This disappoints and angers the patient community, who say the National Institutes of Health should focus on ways to stop their suffering instead of simply trying to understand why they’re suffering.
“It’s unconscionable that more than four years since this began, we still don’t have one FDA-approved drug,” said Meighan Stone, executive director of the Long COVID Campaign, a patient-led advocacy organization. Stone was among several people with long covid who spoke at a workshop hosted by the NIH in September where patients, clinicians, and researchers discussed their priorities and frustrations around the agency’s approach to long-covid research.
Some doctors and researchers are also critical of the agency’s research initiative, called RECOVER, or Researching COVID to Enhance Recovery. Without clinical trials, physicians specializing in treating long covid must rely on hunches to guide their clinical decisions, said Ziyad Al-Aly, chief of research and development with the VA St Louis Healthcare System.
“What [RECOVER] lacks, really, is clarity of vision and clarity of purpose,” said Al-Aly, saying he agrees that the NIH has had enough time and money to produce more meaningful progress.
Now the NIH is starting to determine how to allocate an additional $662 million of funding for long-covid research, $300 million of which is earmarked for clinical trials. These funds will be allocated over the next four http://years.at/ the end of October, RECOVER issued a request for clinical trial ideas that look at potential therapies, including medications, saying its goal is “to work rapidly, collaboratively, and transparently to advance treatments for Long COVID.”
This turn suggests the NIH has begun to respond to patients. This has stirred cautious optimism among those who say that the agency’s approach to long covid has lacked urgency in the search for effective treatments.Stone calls this $300 million a down payment. She warns it’s going to take a lot more money to help people like Hayes regain some degree of health.“There really is a burden to make up this lost time now,” Stone said.
The NIH told KFF Health News and NPR via email that it recognizes the urgency in finding treatments. But to do that, there needs to be an understanding of the biological mechanisms that are making people sick, which is difficult to do with post-infectious conditions.
That’s why it has funded research into how long covid affects lung function, or trying to understand why only some people are afflicted with the condition.
Good Science Takes Time
In December 2020, Congress appropriated $1.15 billion for the NIH to launch RECOVER, raising hopes in the long-covid patient community.
Then-NIH Director Francis Collins explained that RECOVER’s goal was to better understand long covid as a disease and that clinical trials of potential treatments would come later.
According to RECOVER’s website, it has funded eight clinical trials to test the safety and effectiveness of an experimental treatment or intervention. Just one of those trials has published results.
On the other hand, RECOVER has supported more than 200 observational studies, such as research on how long covid affects pulmonary function and on which symptoms are most common. And the initiative has funded more than 40 pathobiology studies, which focus on the basic cellular and molecular mechanisms of long covid.
RECOVER’s website says this research has led to crucial insights on the risk factors for developing long covid and on understanding how the disease interacts with preexisting conditions.
It notes that observational studies are important in helping scientists to design and launch evidence-based clinical trials.
Good science takes time, said Leora Horwitz, the co-principal investigator for the RECOVER-Adult Observational Cohort at New York University. And long covid is an “exceedingly complicated” illness that appears to affect nearly every organ system, she said.
This makes it more difficult to study than many other diseases. Because long covid harms the body in so many ways, with widely variable symptoms, it’s harder to identify precise targets for treatment.
“I also will remind you that we’re only three, four years into this pandemic for most people,” Horwitz said. “We’ve been spending much more money than this, yearly, for 30, 40 years on other conditions.”
NYU received nearly $470 million of RECOVER funds in 2021, which the institution is using to spearhead the collection of data and biospecimens from up to 40,000 patients. Horwitz said nearly 30,000 are enrolled so far.
This vast repository, Horwitz said, supports ongoing observational research, allowing scientists to understand what is happening biologically to people who don’t recover after an initial infection — and that will help determine which clinical trials for treatments are worth undertaking.
“Simply trying treatments because they are available without any evidence about whether or why they may be effective reduces the likelihood of successful trials and may put patients at risk of harm,” she said.
Delayed Hopes or Incremental Progress?
The NIH told KFF Health News and NPR that patients and caregivers have been central to RECOVER from the beginning, “playing critical roles in designing studies and clinical trials, responding to surveys, serving on governance and publication groups, and guiding the initiative.”But the consensus from patient advocacy groups is that RECOVER should have done more to prioritize clinical trials from the outset. Patients also say RECOVER leadership ignored their priorities and experiences when determining which studies to fund.
RECOVER has scored some gains, said JD Davids, co-director of Long COVID Justice. This includes findings on differences in long covid between adults and kids.But Davids said the NIH shouldn’t have named the initiative “RECOVER,” since it wasn’t designed as a streamlined effort to develop treatments.
“The name’s a little cruel and misleading,” he said.
RECOVER’s initial allocation of $1.15 billion probably wasn’t enough to develop a new medication to treat long covid, said Ezekiel J. Emanuel, co-director of the University of Pennsylvania’s Healthcare Transformation Institute.
But, he said, the results of preliminary clinical trials could have spurred pharmaceutical companies to fund more studies on drug development and test how existing drugs influence a patient’s immune response.
Emanuel is one of the authors of a March 2022 covid roadmap report. He notes that RECOVER’s lack of focus on new treatments was a problem. “Only 15% of the budget is for clinical studies. That is a failure in itself — a failure of having the right priorities,” he told KFF Health News and NPR via email.
And though the NYU biobank has been impactful, Emanuel said there needs to be more focus on how existing drugs influence immune response.
He said some clinical trials that RECOVER has funded are “ridiculous,” because they’ve focused on symptom amelioration, for example to study the benefits of over-the-counter medication to improve sleep. Other studies looked at non-pharmacological interventions, such as exercise and “brain training” to help with cognitive fog.
People with long covid say this type of clinical research contributes to what many describe as the “gaslighting” they experience from doctors, who sometimes blame a patient’s symptoms on anxiety or depression, rather than acknowledging long covid as a real illness with a physiological basis.
“I’m just disgusted,” said long-covid patient Hayes. “You wouldn’t tell somebody with diabetes to breathe through it.”
Chimére L. Sweeney, director and founder of the Black Long Covid Experience, said she’s even taken breaks from seeking treatment after getting fed up with being told that her symptoms were due to her diet or mental health.
“You’re at the whim of somebody who may not even understand the spectrum of long covid,” Sweeney said.
Insurance Battles Over Experimental Treatments
Since there are still no long-covid treatments approved by the Food and Drug Administration, anything a physician prescribes is classified as either experimental — for unproven treatments — or an off-label use of a drug approved for other conditions. This means patients can struggle to get insurance to cover prescriptions.
Michael Brode, medical director for UT Health Austin’s Post-COVID-19 Program — said he writes many appeal letters. And some people pay for their own treatment.
For example, intravenous immunoglobulin therapy, low-dose naltrexone, and hyperbaric oxygen therapy are all promising treatments, he said.
For hyperbaric oxygen, two small, randomized controlled studies show improvements for the chronic fatigue and brain fog that often plague long-covid patients. The theory is that higher oxygen concentration and increased air pressure can help heal tissues that were damaged during a covid infection.
However, the out-of-pocket cost for a series of sessions in a hyperbaric chamber can run as much as $8,000, Brode said.
“Am I going to look a patient in the eye and say, ‘You need to spend that money for an unproven treatment’?” he said. “I don’t want to hype up a treatment that is still experimental. But I also don’t want to hide it.”
There’s a host of pharmaceuticals that have promising off-label uses for long covid, said microbiologist Amy Proal, president and chief scientific officer at the Massachusetts-based PolyBio Research Foundation. For instance, she’s collaborating on a clinical study that repurposes two HIV drugs to treat long covid.
Proal said research on treatments can move forward based on what’s already understood about the disease. For instance, she said that scientists have evidence — partly due to RECOVER research — that some patients continue to harbor small amounts of viral material after a covid infection. She has not received RECOVER funds but is researching antivirals.
But to vet a range of possible treatments for the millions suffering now — and to develop new drugs specifically targeting long covid — clinical trials are needed. And that requires money.
Hayes said she would definitely volunteer for an experimental drug trial. For now, though, “in order to not be absolutely miserable,” she said she focuses on what she can do, like having dinner with her http://family.at/ the same time, Hayes doesn’t want to spend the rest of her life on a beige couch.
RECOVER’s deadline to submit research proposals for potential long-covid treatments is Feb. 1.
This article is from a partnership that includes NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
The Mental Health Dangers Of Oversharing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oversharers can be fun and amiable; the life of the party. In and of itself, this something that can be considered “pro-social” and thus healthy.
But the problem for one’s mental health in the long-run lies in the “over” part of oversharing. Sometimes, if not checking in with the other person’s comfort, oversharing can be “trauma-dumping”, and push people away. Alternatively, if the oversharing exposes an unmet need, it can make the other person feel obliged to try to help in some fashion, which in the long run may also cause awkwardness and withdrawal.
Some potential problems are purely internal, such the feelings of shame or anxiety that can come afterwards; “I should not have been so vulnerable”, “What if my friends think badly of me now?”, etc.
And of course, sometimes those fears are then validated by reality, if “friends” indeed take advantage of that, or withdraw their friendship. That’s a minority occurrence, but it doesn’t make it any less of a crushing thing if it happens.
Sometimes people overshare because of being a bad judge of what’s a socially-approved appropriate amount of sharing; sometimes people overshare out of a need for closeness, and perhaps the hope of hearing what one needed to hear previously.
The dangers of oversharing don’t mean that we should never speak about our experiences and feelings; in fact sometimes, it is the most healthy thing to do—be it because it’s something that needs communicating to a specific person, or because it’s something we just need to “get off our chest”.
In short, it can be good to share! It can also be good to do so judiciously, by conscious decision and not in response to a spur-of-the-moment impulse, and remember to prioritize our own safety.
Below, Alain de Botton explains more of the psychodynamics of this:
Click Here If The Embedded Video Doesn’t Load Automatically!
10almonds tip, not included in the video: unsure whether your urge to share is too impulsive or not? Write a letter/email, and wait until the next day to decide whether or not to send it.
Want to read more?
Check out:
Breathe; Don’t Vent (At Least In The Moment)
Take care!
Share This Post
-
Ramadan is almost here. 5 tips to boost your wellbeing and energy levels if you’re fasting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ramadan is one of the most significant months of the Islamic lunar calendar. It marks the time when the Quran was revealed to Prophet Mohammed (peace be upon him).
Almost 2 billion Muslims worldwide observe this month of prayer and reflection, which includes fasting between two prayers, Fajr at dawn and Maghrib at sunset.
Ramadan is about purifying the mind, body and soul, and practising self-restraint. It’s a time for spiritual growth and dedication to God (or Allah in Arabic). Ramadan also brings people together for meals and celebrations, with a focus on helping those less fortunate.
Depending on where you live, Ramadan can mean going 12 to 19 hours without eating or drinking anything, including water.
Our research shows choosing balanced, nutrient-dense foods and drinks can result in better wellbeing and greater energy levels than following your usual diet during Ramadan.
Here’s what to consider if you’re fasting for Ramadan.
Drazen Zigic/Shutterstock Do you have any health issues?
Healthy Muslims are expected to fast during Ramadan once they have reached puberty.
Frail older adults are exempt from fasting, as are pregnant, breastfeeding and menstruating women. Anyone who cannot participate in fasting can make up for the missed fasting days later.
People with chronic illness or mental health may be exempt if fasting poses a risk to their health. If you suffer from chronic illness, such as diabetes, heart disease or kidney problems, and want to fast, consult your GP first.
Fasting can have severe health consequences for people with certain medical conditions and those who rely on prescription medication. Some medications need to be taken at a specific time (and some with food) to be safe and effective.
If you’re not drinking enough water during Ramadan, your body might also handle some medications differently: they may not work as well or cause side effects.
For people who can safely fast, here are five tips to maintain your wellbeing during Ramadan.
1. Plan ahead
In preparation for Ramadan, stock up on essentials. Plan your meals and hydration in advance, to stay on top of your nutritional intake.
Start reducing your caffeine gradually in the week leading to Ramadan, so your body can adjust. This can help prevent or reduce the fasting headaches that many experience at the beginning of Ramadan.
Move your meals gradually towards Suhoor and Iftar times, so your body gets used to the new mealtimes.
Plan your meals ahead of time. Ground Picture/Shutterstock 2. Stay hydrated
Staying hydrated is important during Ramadan. Women should aim to drink 2.1 litres of water or fluids (such as coconut water, clear soups, broths or herbal teas) each day. Men should aim for 2.6 litres.
Limit the intake of sugary or artificially sweetened drinks and enjoy fresh fruit juice only in moderation. Sugary drinks cause a rapid increase in blood sugar levels. The body responds by releasing insulin, causing a drop in blood sugar, which can leave you feeling fatigued, irritable and hungry.
Increase your hydration by including water-rich foods, such as cucumbers and watermelon, in your diet.
3. Get your nutrients early
Before dawn, have a nutrient-rich, slow-digesting meal, along with plenty of water.
Select healthy nutrient-dense food with proteins and fats from lean meats, fish, chickpeas, tofu, nuts and seeds.
Choose whole grain products, a variety of vegetables and fruits, and fermented foods, such as kimchi and pickles, which can support your digestion.
When you prepare your meals, consider grilling, steaming or air frying instead of deep frying.
Stay away from processed foods such as cakes, ice cream, chips and chocolates, as they often lack essential nutrients and are high in sugar, salt and fat. Processed foods also tend to be low in fibre and protein, which are crucial for maintaining a feeling of fullness.
4. Avoid the temptation to overeat in the evening
At sunset, many Muslims come together with family and friends for the fast-breaking evening meal (Iftar). During these occasions, it may be tempting to overindulge in sweets, salty snacks and fatty dishes.
But overeating can strain the digestive system, cause discomfort and disrupt sleep.
Start with something small. Tekkol/Shutterstock Instead, listen to your body’s signals, control your portions, and eat mindfully – this means slowly and without distractions.
Start with something small, such as a date and a glass of water. You may choose to complete the Maghrib prayer before returning for your main meal and more fluids.
5. Keep moving
Finally, try to include some light exercise into your schedule, to maintain your fitness and muscle mass, and promote sleep.
But avoid heavy workouts, sauna and intensive sports while fasting, as these may increase dehydration, which can increase your risk of feeling faint and falling.
Romy Lauche, Deputy Director (Research), National Centre for Naturopathic Medicine, Southern Cross University; Fatima El-Assaad, Senior Research Fellow, Microbiome Research Centre, UNSW Sydney, and Jessica Bayes, Postdoctoral Research Fellow at the National Centre for Naturopathic Medicine, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
7 Ways To Boost Mitochondrial Health To Fight Disease
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fatigue and a general lack of energy can be symptoms of many things, and for most of them, looking after our mitochondrial health can at least help, if not outright fix the issue.
The Seven Ways
Dr. Jonas Kuene suggests that we…
- Enjoy a good diet: especially, limiting simple sugars, reducing overall carbohydrate intake, and swapping seed oils for healthier oils like avocado oil and olive oil.
- Take supplements: including coenzyme Q10, alpha-lipoic acid, and vitamins
- Decrease exposure to toxins: limit alcohol consumption (10almonds tip: limit it to zero if you can), avoid foods that are likely high in heavy metals or pesticides, and check you’re not being overmedicated (there can be a bit of a “meds creep” over time if left unchecked, so it’s good to periodically do a meds review in case something is no longer needed)
- Practice intermittent fasting: Dr. Kuene suggests a modest 16–18 hours fast per week; doing so daily is generally considered good advice, for those for whom this is a reasonable option
- Build muscle: exercise in general is good for mitochondria, but body composition itself counts for a lot too
- Sleep: aiming for 7–9 hours, and if that’s not possible at night, add a nap during the day to make up the lost time
- Get near-infrared radiation: from the sun, and/or made-for-purpose IR health devices.
For more info on these (including the referenced science), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Coenzyme Q10 From Foods & Supplements
- How To Reduce Or Quit Alcohol
- Intermittent Fasting: What’s the truth?
- Build Muscle (Healthily!)
- Red Light, Go!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Psychology Sunday: Family Estrangement & How To Fix It
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Estrangement, And How To Heal It
We’ve written before about how deleterious to the health loneliness and isolation can be, and what things can be done about it. Today, we’re tackling a related but different topic.
We recently had a request to write about…
❝Reconciliation of relationships in particular estrangement mother adult daughter❞
And, this is not only an interesting topic, but a very specific one that affects more people than is commonly realized!
In fact, a recent 800-person study found that more than 43% of people experienced family estrangement of one sort or another, and a more specific study of more than 2,000 mother-child pairs found that more than 11% of mothers were estranged from at least one adult child.
So, if you think of the ten or so houses nearest to you, probably at least one of them contains a parent estranged from at least one adult child. Maybe it’s yours. Either way, we hope this article will give you some pause for thought.
Which way around?
It makes a difference to the usefulness of this article whether any given reader experiencing estrangement is the parent or the adult child. We’re going to assume the reader is the parent. It also makes a difference who did the estranging. That’s usually the adult child.
So, we’re broadly going to write with that expectation.
Why does it happen?
When our kids are small, we as parents hold all the cards. It may not always feel that way, but we do. We control our kids’ environment, we influence their learning, we buy the food they eat and the clothes they wear. If they want to go somewhere, we probably have to take them. We can even set and enforce rules on a whim.
As they grow, so too does their independence, and it can be difficult for us as parents to relinquish control, but we’re going to have to at some point. Assuming we are good parents, we just hope we’ve prepared them well enough for the world.
Once they’ve flown the nest and are living their own adult lives, there’s an element of inversion. They used to be dependent on us; now, not only do they not need us (this is a feature not a bug! If we have been good parents, they will be strong without us, and in all likelihood one day, they’re going to have to be), but also…
We’re more likely to need them, now. Not just in the “oh if we have kids they can look after us when we’re old” sense, but in that their social lives are growing as ours are often shrinking, their family growing, while ours, well, it’s the same family but they’re the gatekeepers to that now.
If we have a good relationship, this goes fine. However, it might only take one big argument, one big transgression, or one “final straw”, when the adult child decides the parent is more trouble than they’re worth.
And, obviously, that’s going to hurt. But it’s pretty much how it pans out, according to studies:
Here be science: Tensions in the Parent and Adult Child Relationship: Links to Solidarity and Ambivalence
How to fix it, step one
First, figure out what went wrong.
Resist any urge to protect your own feelings with a defensive knee-jerk “I don’t know; I was a good, loving parent”. That’s a very natural and reasonable urge and you’re quite possibly correct, but it won’t help you here.
Something pushed them away. And, it will almost certainly have been a push factor from you, not a pull factor from whoever is in their life now. It’s easy to put the blame externally, but that won’t fix anything.
And, be honest with yourself; this isn’t a job interview where we have to present a strength dressed up as a “greatest weakness” for show.
You can start there, though! If you think “I was too loving”, then ok, how did you show that love? Could it have felt stifling to them? Controlling? Were you critical of their decisions?
It doesn’t matter who was right or wrong, or even whether or not their response was reasonable. It matters that you know what pushed them away.
How to fix it, step two
Take responsibility, and apologize. We’re going to assume that your estrangement is such that you can, at least, still get a letter to them, for example. Resist the urge to argue your case.
Here’s a very good format for an apology; please consider using this template:
The 10-step (!) apology that’s so good, you’ll want to make a note of it
You may have to do some soul-searching to find how you will avoid making the same mistake in the future, that you did in the past.
If you feel it’s something you “can’t change”, then you must decide what is more important to you. Only you can make that choice, but you cannot expect them to meet you halfway. They already made their choice. In the category of negotiation, they hold all the cards now.
How to fix it, step three
Now, just wait.
Maybe they will reply, forgiving you. If they do, celebrate!
Just be aware that once you reconnect is not the time to now get around to arguing your case from before. It will never be the time to get around to arguing your case from before. Let it go.
Nor should you try to exact any sort of apology from them for estranging you, or they will at best feel resentful, wonder if they made a mistake in reconnecting, and withdraw.
Instead, just enjoy what you have. Many people don’t get that.
If they reply with anger, maybe it will be a chance to reopen a dialogue. If so, family therapy could be an approach useful for all concerned, if they are willing. Chances are, you all have things that you’d all benefit from talking about in a calm, professional, moderated, neutral environment.
You might also benefit from a book we reviewed previously, “Parent Effectiveness Training”. This may seem like “shutting the stable door after the horse has bolted”, but in fact it’s a very good guide to relationship dynamics in general, and extensively covers relations between parents and adult children.
If they don’t reply, then, you did your part. Take solace in knowing that much.
Some final thoughts:
At the end of the day, as parents, our kids living well is (hopefully) testament to that we prepared them well for life, and sometimes, being a parent is a thankless task.
But, we (hopefully) didn’t become parents for the plaudits, after all.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pine Bark’s Next-Level Antioxidant Properties
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pine Bark’s Next-Level Antioxidant Properties
Pine bark extract has been used by the indigenous peoples of N. America for a very long time, to treat a variety of ailments.
This one falls into the category of “things from traditional medicine that eventually got investigated and their scientific worth noticed by people from outside of those cultures”.
Not all pine trees!
If you happen to have pine trees near you, be aware that without sufficient botanical knowledge, you could find yourself bark-harvesting from the wrong tree—but many species of pine do have these qualities.
Useful (for this purpose) pine trees include, but are not limited to:
- Pinus banksiana
- Pinus massoniana
- Pinus pinaster
- Pinus radiata
- Pinus resinosa
- Pinus strobus
…which is already a fair list, but there are dozens more that have not been studied, and/or found lacking in medicinal qualities, and/or just didn’t make our list here today.
What does it do & How does it work?
We sneakily put those two questions together today because it’s easiest to explain in one:
The Pinus family in general has powerful antioxidant qualities, and not just like blueberries or coffee (wonderful as those are).
Rather, it has:
- Phenolic acids: these are the polyphenols found in many plant foods rich in antioxidants. These are great, but they aren’t the exciting part here.
- Catechins: these aren’t classified as antioxidants, but they are flavonoids that do the same job in a slightly different way
- Procyanidins: another class of flavonoids, and this is where pine bark really comes into its own
And yes, as ever, “those three things that always seem to come together”, it having these antioxidant properties means it is also anti-inflammatory and anti-cancer:
…and anti-aging:
Pleiotropic Effects of French Maritime Pine Bark Extract to Promote Healthy Aging
…which does of course mean that it almost certainly fights age-related cognitive decline, though studies for that have been animal studies so far, such as:
- Pine Bark Polyphenolic Extract Attenuates Amyloid-β and Tau Misfolding in a Model System of Alzheimer’s Disease Neuropathology
- Neuroprotective and Anti-Inflammatory Effects of Pinus densiflora Bark Extract in Gerbil Hippocampus Following Transient Forebrain Ischemia
- Neuroprotective Effects of Korean Red Pine ( Pinus densiflora) Bark Extract and Its Phenolics
- Pine bark treatment decelerates plaque development and improves spatial memory in Alzheimer’s disease mice
Where to get it?
As ever, we don’t sell it, but here’s an example product on Amazon for your convenience; we recommend shopping around though, as prices vary a lot!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: