Sometimes, Perfect Isn’t Practical!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝10 AM breakfast is not realistic for most. What’s wrong with 8 AM and Evening me at 6. Don’t quite understand the differentiation.❞
(for reference, this is about our “Breakfasting For Health?” main feature)
It’s not terrible to do it the way you suggest It’s just not optimal, either, that’s all!
Breakfasting at 08:00 and then dining at 18:00 is ten hours apart, so no fasting benefits between those. Let’s say you take half an hour to eat dinner, then eat nothing again until breakfast, that’s 18:30 to 08:00, so that’s 13½ hours fasting. You’ll recall that fasting benefits start at 12 hours into the fast, so that means you’d only get 1½ hours of fasting benefits.
As for breakfasting at 08:00 regardless of intermittent fasting considerations, the reason for the conclusion of around 10:00 being optimal, is based on when our body is geared up to eat breakfast and get the most out of that, which the body can’t do immediately upon waking. So if you wake and get sunlight at 08:30, get a little moderate exercise, then by 10:00 your digestive system will be perfectly primed to get the most out of breakfast.
However! This is entirely based on you waking and getting sunlight at 08:30.
So, iff you wake and get sunlight at 06:30, then in that case, breakfasting at 08:00 would give the same benefits as described above. What’s important is the 1½ hour priming-time.
Writer’s note: our hope here is always to be informational, not prescriptive. Take what works for you; ignore what doesn’t fit your lifestyle.
I personally practice intermittent fasting for about 21hrs/day. I breakfast (often on nuts and perhaps a little salad) around 16:00, and dine at around 18:00ish, giving myself a little wiggleroom. I’m not religious about it and will slide it if necessary.
As you can see: that makes what is nominally my breakfast practically a pre-dinner snack, and I clearly ignore the “best to eat in the morning” rule because that’s not consistent with my desire to have a family dinner together in the evening while still practicing the level of fasting that I prefer.
Science is science, and that’s what we report here. How we apply it, however, is up to us all as individuals!
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Knit for Health & Wellness – by Betsan Corkhill
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Betsan Corkhill, a physiotherapist, has more than just physiotherapy in mind when it comes to the therapeutic potential of knitting (although yes, also physiotherapy!), and much of this book is about the more psychological benefits that go way beyond “it’s a relaxing pastime”.
She makes the case for how knitting (much like good mental health) requires planning, action, organization, persistence, focus, problem-solving, and flexibility—and thus the hobby develops and maintains all the appropriate faculties for those things, which will then be things you get to keep in the rest of your life, too.
Fun fact: knitting, along with other similar needlecrafts, was the forerunner technology for modern computer programming! And indeed, early computers, the kind with hole-punch data streams, used very similar pattern-storing methods to knitting patterns.
So, for something often thought of as a fairly mindless activity for those not in the know, knitting has a lot to offer for what’s between your ears, as well as potentially something for keeping your ears warm later.
One thing this book’s not, by the way: a “how to” guide for learning to knit. It assumes you either have that knowledge already, or will gain it elsewhere (there are many tutorials online).
Bottom line: if you’re in the market for a new hobby that’s good for your brain, this book will give you great motivation to give knitting a go!
Click here to check out Knit For Health & Wellness, and get knitting!
Share This Post
-
Caffeine: Cognitive Enhancer Or Brain-Wrecker?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Two Sides Of Caffeine
We asked you for your health-related opinions on caffeine itself, not necessarily the coffee, tea, energy drinks, etc that might contain it.
We have, by the way previously written about the health effects of coffee and tea specifically:
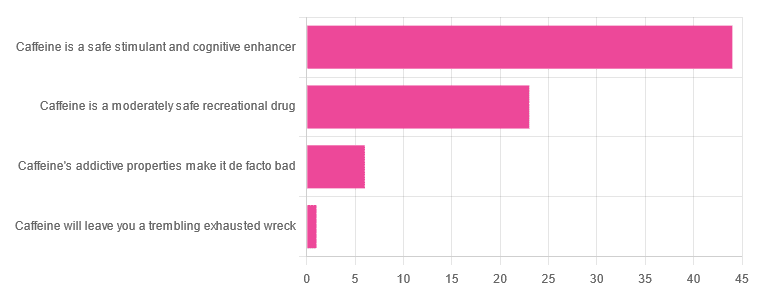
As for our question about caffeine itself, though, we got the above-depicted, below-described, set of results:
- About 59% said “caffeine is a safe stimulant and cognitive enhancer”
- About 31% said “caffeine is a moderately safe recreational drug”
- About 8% said “caffeine’s addictive properties make it de facto bad”
- One (1) person said “caffeine will leave you a trembling exhausted wreck”
But what does the science say?
Caffeine is addictive: True or False?
True, though one will find occasional academics quibbling the definition. Most of the studies into the mechanisms of caffeine addiction have been conducted on rats, but human studies exist too and caffeine is generally considered addictive for humans, for example:
See also:
Notwithstanding its addictive status, caffeine is otherwise safe: True or False?
True-ish, for most people. Some people with heart conditions or a hypersensitivity to caffeine may find it is not safe for them at all, and for the rest of us, the dose makes the poison. For example:
❝Can too much caffeine kill you? Although quite rare, caffeine can be fatal in cases of overdose; such circumstances are generally not applicable to healthy individuals who typically consume caffeine via beverages such as tea or coffee.❞
this paper, by the way, also includes a good example of academics quibbling the definition of addiction!
Caffeine is a cognitive enhancer: True or False?
True, but only in the case of occasional use. If you are using it all the time, your physiology will normalize it and you will require caffeine in order to function at your normal level. To attain higher than that, once addicted to caffeine, would now require something else.
Read more: Caffeine: benefits and drawbacks for technical performance
Caffeine will leave you a trembling exhausted wreck: True or False?
True or False depending on usage:
- The famously moderate 3–5 cups per day will not, for most people, cause any such problems.
- Using/abusing it to make up for lost sleep (or some other source of fatigue, such as physical exhaustion from exertion), however, is much more likely to run into problems.
In the latter case, caffeine really is the “payday loan” of energy! It’ll give you an adrenal boost now (in return, you must suffer the adrenal dumping later, along with lost energy expended in the adrenaline surge), and also, the tiredness that you thought was gone, was just caffeine’s adenosine-blocking activities temporarily preventing you from being able to perceive the tiredness. So you’ll have to pay that back later, with interest, because of the extra time/exertion too.
Want to make caffeine a little more gentle on your system?
Taking l-theanine alongside caffeine can ameliorate some of caffeine’s less wonderful effects—and as a bonus, l-theanine has some nifty benefits of its own, too:
Enjoy!
Share This Post
-
How To Unchoke Yourself If You Are Dying Alone
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The first things that most people think of, won’t work. This firefighter advises on how to actually do it:
Steps to take
Zero’th step: he doesn’t mention this, but try coughing first. You might think coughing will be a natural reaction anyway, but that tends only to happen automatically with small partial obstructions, not a complete blockage. Either way, try to cough forcefully to see if it dislodges whatever you’re choking on. If that doesn’t work…
Firstly: don’t rely on calling for help if you’re alone and cannot speak; you’re unlikely to be able to communicate and you will just waste time (when you don’t have time to waste). Even if you call emergency services and they trace your location, chances are that, at most, a cop car will show up some hours later to see what it was about. They will not dispatch an ambulance on the strength of “someone called and said nothing”.
Secondly, it is probable that will not be able to perform an abdominal thrust (also called Heimlich maneuvre in the US) on yourself the way you could on another person, and hitting your chest with your hand will produce insufficient force even if you’re quite strong. Nor are you likely to be able to slap yourself on the back to way you might another person.
Instead, he advises:
- Find a sturdy object: use a chair, table, countertop, or another firm surface that has an edge.
- Use gravity to perform self-Heimlich: position yourself with the edge of the object just below your sternum (he says ribcage, but the visuals show he clearly means the bottom of the sternum, where the diaphragm is, not the lower ribs). Fall onto the object forcefully to create pressure and dislodge the obstruction. This will not be fun.
- If it doesn’t work indoors: move to a visible outdoor location like your yard or a neighbor’s lawn. Falling visibly on the ground will likely alert someone to call for help.
While doing the above, remain as calm as possible, as this will not only increase the length of time you have before passing out, but will also help avoid your throat muscles tightening even more, worsening the choking.
After doing the above, seek medical attention now that you can communicate; you’ve probably broken some ribs and you might have organ damage.
For more on all this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Survive A Heart Attack When You’re Alone ← very different advice for this scenario!
Take care!
Share This Post
Related Posts
-
Cacao vs Carob – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cacao to carob, we picked the cacao.
Why?
It’s close, and may depend a little on your priorities!
In terms of macros, the cacao has more protein and fat, while the carob has more carbohydrates, mostly sugar. Since people will not generally eat this by the spoonful, and will instead either make drinks or cook with it, we can’t speak for the glycemic index or general health impact of the sugars. As for the fats, on the one hand the cacao does contain saturated fat; on the other, this merely means that different saturated fat will usually be added to the carob if making something with it. Still, slight win for the carob on the fat front. Protein, of course, is entirely in cacao’s favor.
In the category of vitamins and minerals, they’re about equal on vitamins, while cacao wins easily on the mineral front, boasting more copper, iron, magnesium, manganese, and phosphorus.
While both have a generous antioxidant content, this one’s another win for cacao, with about 3x the active polyphenols and flavonoids.
In short: both are good, consumed in moderation and before adding unhealthy extra ingredients—but we say cacao comes out the winner.
If you’re looking specifically for the above-depicted products, by the way, here they are:
Want to learn more?
You might like to read:
- Enjoy Bitter Foods For Your Heart & Brain
- Chocolate & Health
- The Truth About Chocolate & Skin Health
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Could ADHD drugs reduce the risk of early death? Unpacking the findings from a new Swedish study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Attention-deficit hyperactivity disorder (ADHD) can have a considerable impact on the day-to-day functioning and overall wellbeing of people affected. It causes a variety of symptoms including difficulty focusing, impulsivity and hyperactivity.
For many, a diagnosis of ADHD, whether in childhood or adulthood, is life changing. It means finally having an explanation for these challenges, and opens up the opportunity for treatment, including medication.
Although ADHD medications can cause side effects, they generally improve symptoms for people with the disorder, and thereby can significantly boost quality of life.
Now a new study has found being treated for ADHD with medication reduces the risk of early death for people with the disorder. But what can we make of these findings?
A large study from Sweden
The study, published this week in JAMA (the prestigious journal of the American Medical Association), was a large cohort study of 148,578 people diagnosed with ADHD in Sweden. It included both adults and children.
In a cohort study, a group of people who share a common characteristic (in this case a diagnosis of ADHD) are followed over time to see how many develop a particular health outcome of interest (in this case the outcome was death).
For this study the researchers calculated the mortality rate over a two-year follow up period for those whose ADHD was treated with medication (a group of around 84,000 people) alongside those whose ADHD was not treated with medication (around 64,000 people). The team then determined if there were any differences between the two groups.
What did the results show?
The study found people who were diagnosed and treated for ADHD had a 19% reduced risk of death from any cause over the two years they were tracked, compared with those who were diagnosed but not treated.
In understanding this result, it’s important – and interesting – to look at the causes of death. The authors separately analysed deaths due to natural causes (physical medical conditions) and deaths due to unnatural causes (for example, unintentional injuries, suicide, or accidental poisonings).
The key result is that while no significant difference was seen between the two groups when examining natural causes of death, the authors found a significant difference for deaths due to unnatural causes.
So what’s going on?
Previous studies have suggested ADHD is associated with an increased risk of premature death from unnatural causes, such as injury and poisoning.
On a related note, earlier studies have also suggested taking ADHD medicines may reduce premature deaths. So while this is not the first study to suggest this association, the authors note previous studies addressing this link have generated mixed results and have had significant limitations.
In this new study, the authors suggest the reduction in deaths from unnatural causes could be because taking medication alleviates some of the ADHD symptoms responsible for poor outcomes – for example, improving impulse control and decision-making. They note this could reduce fatal accidents.
The authors cite a number of studies that support this hypothesis, including research showing ADHD medications may prevent the onset of mood, anxiety and substance use disorders, and lower the risk of accidents and criminality. All this could reasonably be expected to lower the rate of unnatural deaths.
Strengths and limitations
Scandinavian countries have well-maintained national registries that collect information on various aspects of citizens’ lives, including their health. This allows researchers to conduct excellent population-based studies.
Along with its robust study design and high-quality data, another strength of this study is its size. The large number of participants – almost 150,000 – gives us confidence the findings were not due to chance.
The fact this study examined both children and adults is another strength. Previous research relating to ADHD has often focused primarily on children.
One of the important limitations of this study acknowledged by the authors is that it was observational. Observational studies are where the researchers observe and analyse naturally occurring phenomena without intervening in the lives of the study participants (unlike randomised controlled trials).
The limitation in all observational research is the issue of confounding. This means we cannot be completely sure the differences between the two groups observed were not either partially or entirely due to some other factor apart from taking medication.
Specifically, it’s possible lifestyle factors or other ADHD treatments such as psychological counselling or social support may have influenced the mortality rates in the groups studied.
Another possible limitation is the relatively short follow-up period. What the results would show if participants were followed up for longer is an interesting question, and could be addressed in future research.
What are the implications?
Despite some limitations, this study adds to the evidence that diagnosis and treatment for ADHD can make a profound difference to people’s lives. As well as alleviating symptoms of the disorder, this study supports the idea ADHD medication reduces the risk of premature death.
Ultimately, this highlights the importance of diagnosing ADHD early so the appropriate treatment can be given. It also contributes to the body of evidence indicating the need to improve access to mental health care and support more broadly.
Hassan Vally, Associate Professor, Epidemiology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Carrot vs Sweet Potato – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrot to sweet potato, we picked the sweet potato.
Why?
Both are great! But there’s a winner in the end:
Looking at the macros first, sweet potato has more protein carbs, and fiber, and is thus the “more food per food” item. If they are both cooked the same, then the glycemic index is comparable, despite the carrot’s carbs having more sucrose and the sweet potato’s carbs having more starch. We’ll call this category a tie.
In terms of vitamins, carrots have more of vitamins B9 and K, while sweet potatoes have more of vitamins B1, B2, B3, B5, B6. B7, C, E, and choline. Both are equally high in vitamin A. Thus, the vitamins category is an overwhelming win for sweet potato.
When it comes to minerals, carrots are not higher in any minerals (unless we count that they are slightly higher in sodium, but that is not generally considered a plus for most people in most places most of the time), while sweet potato is higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Another easy win for sweet potato.
Adding up the sections makes for a clear win for the sweet potato as the more nutritionally dense option, but as ever, enjoy either or both!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: