Shame and blame can create barriers to vaccination
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Understanding the stigma surrounding infectious diseases like HIV and mpox may help community health workers break down barriers that hinder access to care.
Looking back in history can provide valuable lessons to confront stigma in health care today, especially toward Black, Latine, LGBTQ+, and other historically underserved communities disproportionately affected by COVID-19 and HIV.
Public Good News spoke with Sam Brown, HIV prevention and wellness program manager at Civic Heart, a community-based organization in Houston’s historic Third Ward, to understand the effects of stigma around sexual health and vaccine uptake.
Brown shared more about Civic Heart’s efforts to provide free confidential testing for sexually transmitted infections, counseling and referrals, and information about COVID-19, flu, and mpox vaccinations, as well as the lessons they’re learning as they strive for vaccine equity.
Here’s what Brown said.
[Editor’s note: This content has been edited for clarity and length.]
PGN: Some people on social media have spread the myth that vaccines cause AIDS or other immune deficiencies when the opposite is true: Vaccines strengthen our immune systems to help protect against disease. Despite being frequently debunked, how do false claims like these impact the communities you serve?
Sam Brown: Misinformation like that is so hard to combat. And it makes the work and the path to overall community health hard because people will believe it. In the work that we do, 80 percent of it is changing people’s perspective on something they thought they knew.
You know, people don’t even transmit AIDS. People transmit HIV. So, a vaccine causing immunodeficiency doesn’t make sense.
With the communities we serve, we might have a person that will believe the myth, and because they believe it, they won’t get vaccinated. Then later, they may test positive for COVID-19.
And depending on social determinants of health, it can impact them in a whole heap of ways: That person is now missing work, they’re not able to provide for their family—if they have a family. It’s this mindset that can impact a person’s life, their income, their ability to function.
So, to not take advantage of something like a vaccine that’s affordable, or free for the most part, just because of misinformation or a misunderstanding—that’s detrimental, you know.
For example, when we talk to people in the community, many don’t know that they can get mpox from their pet, or that it’s zoonotic—that means that it can be transferred between different species or different beings, from animals to people. I see a lot of surprise and shock [when people learn this].
It’s difficult because we have to fight the misinformation and the stigma that comes with it. And it can be a big barrier.
People misunderstand. [They] think that “this is something that gay people or the LGBTQ+ community get,” which is stigmatizing and comes off as blaming. And blaming is the thing that leads us to be misinformed.
PGN: In the last couple years, your organization’s HIV Wellness program has taken on promoting COVID-19, flu, and mpox vaccines to the communities you serve. How do you navigate conversations between sexual health and infectious diseases? Can you share more about your messaging strategies?
S.B.: As we promoted positive sexual health and HIV prevention, we saw people were tired of hearing about HIV. They were tired of hearing about how PrEP works, or how to prevent HIV.
But, when we had an outbreak of syphilis in Houston just last year, people were more inclined to test because of the severity of the outbreak.
So, what our team learned is that sometimes you have to change the message to get people what they need.
We changed our message to highlight more syphilis information and saw that we were able to get more people tested for HIV because we correlated how syphilis and HIV are connected and how a person can be susceptible to both.
Using messages that the community wants and pairing them with what the community needs has been better for us. And we see that same thing with COVID-19, the flu, and RSV. Sometimes you just can’t be married to a message. We’ve had to be flexible to meet our clients where they are to help them move from unsafe practices to practices that are healthy and good for them and their communities.
PGN: You’ve mentioned how hard it is to combat stigma in your work. How do you effectively address it when talking to people one-on-one?
S.B.: What I understand is that no one wants to feel shame. What I see people respond to is, “Here’s an opportunity to do something different. Maybe there was information that you didn’t know that caused you to make a bad decision. And now here’s an opportunity to gain information so that you can make a better decision.”
People want to do what they want to do; they want to live how they want to live. And we all should be able to do that as long as it’s not hurting anyone, but also being responsible enough to understand that, you know, COVID-19 is here.
So, instead of shaming and blaming, it’s best to make yourself aware and understand what it is and how to treat it. Because the real enemy is the virus—it’s the infection, not the people.
When we do our work, we want to make sure that we come from a strengths-based approach. We always look at what a client can do, what that client has. We want to make sure that we’re empowering them from that point. So, even if they choose not to prioritize our message right now, we can’t take that personally. We’ll just use it as a chance to try a new way of framing it to help people understand what we’re trying to say.
And sometimes that can be difficult, even for organizations. But getting past that difficulty comes with a greater opportunity to impact someone else.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat to Beat Disease – by Dr. William Li
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. William Li asks the important question: is your diet feeding disease, or defeating it?
Because everything we put in our bodies makes our health just a little better—or just a little worse. Ok, sometimes a lot worse.
But for most people, when it comes to diet, it’s a death of a thousand cuts of unhealthy food. And that’s what he looks to fix with this book.
The good news: Dr. Li (while not advocating for unhealthy eating, of course), focuses less on what to restrict, and more on what to include. This book covers hundreds of such healthy foods, and ideas (practical, useful ones!) on incorporating them daily, including dozens of recipes.
He mainly looks at five ways our food can help us with…
- Angiogenesis (blood vessel replacement)
- Regeneration (of various bodily organs and systems)
- Microbiome health (and all of its knock-on effects)
- DNA protection (and thus slower cellular aging)
- Immunity (defending the body while also reducing autoimmune problems)
The style is simple and explanatory; Dr. Li is a great educator. Reading this isn’t a difficult read, but you’ll come out of it feeling like you just did a short course in health science.
Bottom line: if you’d like an easy way to improve your health in an ongoing and sustainable way, then this book can help you do just that.
Click here to check out Eat To Beat Disease, and eat to beat disease!
Share This Post
-
Rise And (Really) Shine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q&A with 10almonds Subscribers!
Q: Would love to hear more ideas about effective first thing in the morning time management to get a great start on your day.
A: There are a lot of schools of thought about what’s best in this regard! Maybe we’ll do a main feature sometime. But some things that are almost universally agreed upon are:
- Prepare your to-do list the night before
- Have some sort of buffer between waking up and getting to productivity.
- For me (hi, your writer here) it’s my first coffee of the day. It’s not even about the caffeine, it’s about the ritual of it, it’s a marker that separates my night from the day and tells my brain what gear to get into.
- Others may like to exercise first thing in the morning
- For still yet others, it could be a shower, cold or otherwise
- Some people like a tall glass of lemon water to rehydrate after sleeping!
- If you take drinkable morning supplements such as this pretty awesome nootropic stack, it’s a great time for that and an excellent way to get the brain-juices flowing!
- When you do get to productivity: eat the frog first! What this means is: if eating a frog is the hardest thing you’ll have to do all day, do that first. Basically, tackle the most intimidating task first. That way, you won’t spend your day stressed/anxious and/or subconsciously wasting time in order to procrastinate and avoid it.
- Counterpart to the above: a great idea is to also plan something to look forward to when your working day is done. It doesn’t matter much what it is, provided it’s rewarding to you, that makes you keen to finish your tasks to get to it.
Have a question you’d like to see answered here? Hit reply to this email, or use the feedback widget at the bottom! We always love to hear from you
Share This Post
-
Ice Baths: To Dip Or Not To Dip?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
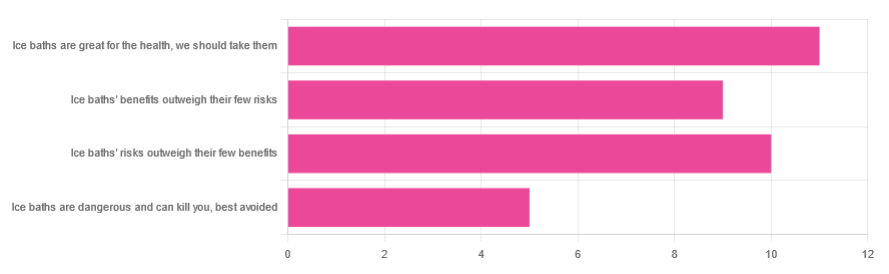
We asked you for your (health-related) view of ice baths, and got the above-depicted, below-described, set of responses:
- About 31% said “ice baths are great for the health; we should take them”
- About 29% said “ice baths’ risks outweigh their few benefits”
- About 26% said “ice baths’ benefits outweigh their few risks”
- About 14% said “ice baths are dangerous and can kill you; best avoided”
So what does the science say?
Freezing water is very dangerous: True or False?
True! Water close to freezing point is indeed very dangerous, and can most certainly kill you.
Fun fact, though: many such people are still saveable with timely medical intervention, in part because the same hypothermia that is killing them also slows down the process* of death
Source (and science) for both parts of that:
Cold water immersion: sudden death and prolonged survival
*and biologically speaking, death is a process, not an event, by the way. But we don’t have room for that today!
(unless you die in some sudden violent way, such as a powerful explosion that destroys your brain instantly; then it’s an event)
Ice baths are thus also very dangerous: True or False?
False! Assuming that they are undertaken responsibly and you have no chronic diseases that make it more dangerous for you.
What does “undertaken responsibly” mean?
Firstly, the temperature should not be near freezing. It should be 10–15℃, which for Americans is 50–59℉.
You can get a bath thermometer to check this, by the way. Here’s an example product on Amazon.
Secondly, your ice bath should last no more than 10–15 minutes. This is not a place to go to sleep.
What chronic diseases would make it dangerous?
Do check with your doctor if you have any doubts, as no list we make can be exhaustive and we don’t know your personal medical history, but the main culprits are:
- Cardiovascular disease
- Hypertension
- Diabetes (any type)
The first two are for heart attack risk; the latter is because diabetes can affect core temperature regulation.
Ice baths are good for the heart: True or False?
True or False depending on how they’re done, and your health before starting.
For most people, undertaking ice baths responsibly, repeated ice bath use causes the cardiovascular system to adapt to better maintain homeostasis when subjected to thermal shock (i.e. sudden rapid changes in temperature).
For example: Respiratory and cardiovascular responses to cold stress following repeated cold water immersion
And because that was a small study, here’s a big research review with a lot of data; just scroll to where it has the heading“Specific thermoregulative adaptations to regular exposure to cold air and/or cold water exposure“ for many examples and much discussion:
Health effects of voluntary exposure to cold water: a continuing subject of debate
Ice baths are good against inflammation: True or False?
True! Here’s one example:
Uric acid and glutathione levels (important markers of chronic inflammation) are also significantly affected:
Uric acid and glutathione levels during short-term whole body cold exposure
Want to know more?
That’s all we have room for today, but check out our previous “Expert Insights” main feature looking at Wim Hof’s work in cryotherapy:
A Cold Shower A Day Keeps The Doctor Away?
Enjoy!
Share This Post
Related Posts
-
100 Ways to Change Your Life – by Liz Moody
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes we crave changing things up, just to feel something new. This can result in anything from bad haircut decisions or impulsive purchases, to crashing and burning-out of a job, project, or relationship. It doesn’t have to be that way, though!
This book brings us (as the title suggest) 100 evidence-based ways of changing things up in a good way—small things that can make a big difference in many areas of life.
In terms of format, these are presented in 100 tiny chapters, each approximately 2 pages long (obviously it depends on the edition, but you get the idea). Great to read in any of at least three ways:
- Cover-to-cover
- One per day for 100 days
- Look up what you need on an ad hoc basis
Bottom line: even if you already do half of these things, the other half will each compound your health happiness one-by-one as you add them. This is a very enjoyable and practical book!
Click here to check out 100 Ways to Change Your Life, and level-up yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eat To Beat Chronic Fatigue!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Eat To Beat Chronic Fatigue
Chronic fatigue is on the rise, and it can make life a living Hell. Days blur into one, and you try to take each day as it comes, but sometimes several days gang up on you at once.
You probably know some lifestyle changes that might help—if only you had the energy to implement them.
You’d like to eat well, but you need to…
- Buy the fresh produce (and take a little rest after)
- Put the groceries away (and take a little rest after)
- Wash the vegetables (and take a little rest after)
- Chop the things as necessary (and take a little rest after)
- Cook dinner (and take a little rest after)
…and now you’re too exhausted to eat it.
So, what can be done?
First, avoid things that cause inflammation, as this is a major contributor to chronic fatigue. You might like our previous main feature:
Next up, really do stay hydrated. It’s less about quantity, and more about ubiquity. Hydrate often.
Best is if you always have some (hydrating) drink on the go.
Do experiment with your diet, and/but keep a food journal of what you eat and how you feel 30–60 minutes after eating it. Only make one change at a time, otherwise you won’t know which change made the difference.
Notice what patterns emerge over time, and adjust your ingredients accordingly.
Limit your caffeine intake. We know that sometimes it seems like the only way to get through the day, but you will always crash later, because it was only ever taxing your adrenal system (thus: making you more tired in the long run) and pulling the wool over the eyes of your adenosine receptors (blocking you from feeling how tired you are, but not actually reducing your body’s tiredness).
Put simply, caffeine is the “payday loan” of energy.
Eat more non-starchy vegetables, and enjoy healthy fats. Those healthy fats can come from nuts and seeds, avocado, or fish (not fried, though!).
The non-starchy vegetables will boost your vitamins and fiber while being easy on your beleaguered metabolism, while the healthy fats will perk up your energy levels without spiking insulin like sugars would.
Pay the fatigue tax up front. What this means is… Instead of throwing away vegetables that didn’t get used because it would take too much effort and you just need an easier dinner today, buy ready-chopped vegetables, for example.
And if you buy vegetables frozen, they’re also often not only cheaper, but also (counterintuitively) contain more nutrients.
A note of distinction:
Many more people have chronic fatigue (the symptom: being exhausted all the time) than have chronic fatigue syndrome (the illness: myalgic encephalomyelitis).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Foods For Managing Hypothyroidism (incl. Hashimoto’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Foods for Managing Hypothyroidism
For any unfamiliar, hypothyroidism is the condition of having an underactive thyroid gland. The thyroid gland lives at the base of the front of your neck, and, as the name suggests, it makes and stores thyroid hormones. Those are important for many systems in the body, and a shortage typically causes fatigue, weight gain, and other symptoms.
What causes it?
This makes a difference in some cases to how it can be treated/managed. Causes include:
- Hashimoto’s thyroiditis, an autoimmune condition
- Severe inflammation (end result is similar to the above, but more treatable)
- Dietary deficiencies, especially iodine deficiency
- Secondary endocrine issues, e.g. pituitary gland didn’t make enough TSH for the thyroid gland to do its thing
- Some medications (ask your pharmacist)
We can’t do a lot about those last two by leveraging diet alone, but we can make a big difference to the others.
What to eat (and what to avoid)
There is nuance here, which we’ll go into a bit, but let’s start by giving the
one-linetwo-line summary that tends to be the dietary advice for most things:- Eat a nutrient-dense whole-foods diet (shocking, we know)
- Avoid sugar, alcohol, flour, processed foods (ditto)
What’s the deal with meat and dairy?
- Meat: avoid red and processed meats; poultry and fish are fine or even good (unless fried; don’t do that)
- Dairy: limit/avoid milk; but unsweetened yogurt and cheese are fine or even good
What’s the deal with plants?
First, get plenty of fiber, because that’s important to ease almost any inflammation-related condition, and for general good health for most people (an exception is if you have Crohn’s Disease, for example).
If you have Hashimoto’s, then gluten (as found in wheat, barley, and rye) may be an issue, but the jury is still out, science-wise. Here’s an example study for “avoid gluten” and “don’t worry about gluten”, respectively:
- The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Women with Hashimoto’s Thyroiditis
- Doubtful Justification of the Gluten-Free Diet in the Course of Hashimoto’s Disease
So, you might want to skip it, to be on the safe side, but that’s up to you (and the advice of your nutritionist/doctor, as applicable).
A word on goitrogens…
Goitrogens are found in cruciferous vegetables and soy, both of which are very healthy foods for most people, but need some extra awareness in the case of hypothyroidism. This means there’s no need to abstain completely, but:
- Keep serving sizes small, for example a 100g serving only
- Cook goitrogenic foods before eating them, to greatly reduce goitrogenic activity
For more details, reading even just the abstract (intro summary) of this paper will help you get healthy cruciferous veg content without having a goitrogenic effect.
(as for soy, consider just skipping that if you suffer from hypothyroidism)
What nutrients to focus on getting?
- Top tier nutrients: iodine, selenium, zinc
- Also important: vitamin B12, vitamin D, magnesium, iron
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: