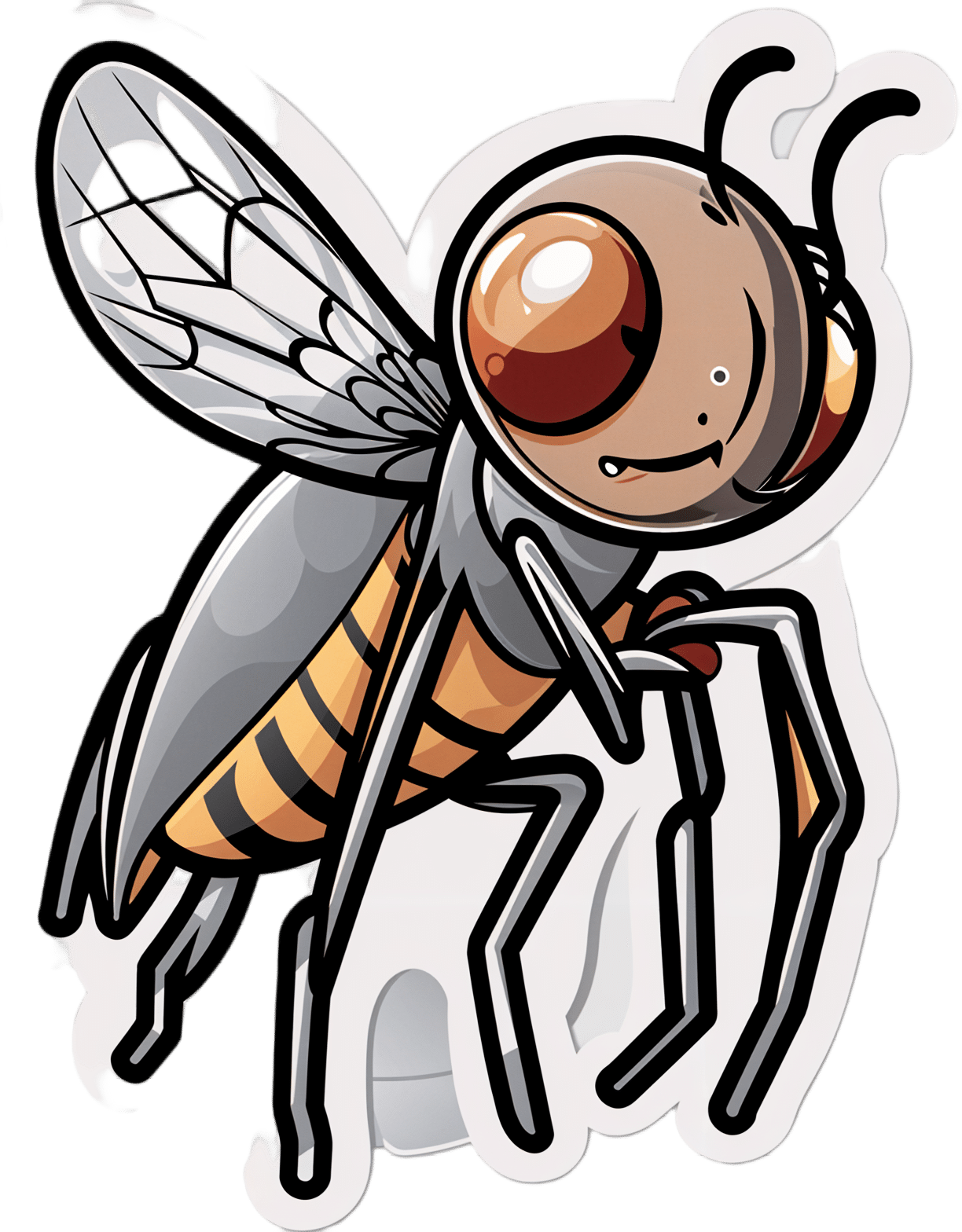
Mosquitoes can spread the flesh-eating Buruli ulcer. Here’s how you can protect yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Each year, more and more Victorians become sick with a flesh-eating bacteria known as Buruli ulcer. Last year, 363 people presented with the infection, the highest number since 2004.
But it has been unclear exactly how it spreads, until now. New research shows mosquitoes are infected from biting possums that carry the bacteria. Mozzies spread it to humans through their bite.
What is Buruli ulcer?
Buruli ulcer, also known as Bairnsdale ulcer, is a skin infection caused by the bacterium Mycobacterium ulcerans.
It starts off like a small mosquito bite and over many months, slowly develops into an ulcer, with extensive destruction of the underlying tissue.
While often painless initially, the infection can become very serious. If left untreated, the ulcer can continue to enlarge. This is where it gets its “flesh-eating” name.
Thankfully, it’s treatable. A six to eight week course of specific antibiotics is an effective treatment, sometimes supported with surgery to remove the infected tissue.
Where can you catch it?
The World Health Organization considers Buruli ulcer a neglected tropical skin disease. Cases have been reported across 33 countries, primarily in west and central Africa.
However, since the early 2000s, Buruli ulcer has also been increasingly recorded in coastal Victoria, including suburbs around Melbourne and Geelong.
Scientists have long known Australian native possums were partly responsible for its spread, and suspected mosquitoes also played a role in the increase in cases. New research confirms this.
Our efforts to ‘beat Buruli’
Confirming the role of insects in outbreaks of an infectious disease is achieved by building up corroborating, independent evidence.
In this new research, published in Nature Microbiology, the team (including co-authors Tim Stinear, Stacey Lynch and Peter Mee) conducted extensive surveys across a 350 km² area of Victoria.
We collected mosquitoes and analysed the specimens to determine whether they were carrying the pathogen, and links to infected possums and people. It was like contact tracing for mosquitoes.

Cameron Webb (NSW Health Pathology)
Molecular testing of the mosquito specimens showed that of the two most abundant mosquito species, only Aedes notoscriptus (a widespread species commonly known as the Australian backyard mosquito) was positive for Mycobacterium ulcerans.
We then used genomic tests to show the bacteria found on these mosquitoes matched the bacteria in possum poo and humans with Buruli ulcer.
We further analysed mosquito specimens that contained blood to show Aedes notoscriptus was feeding on both possums and humans.
To then link everything together, geospatial analysis revealed the areas where human Buruli ulcer cases occur overlap with areas where both mosquitoes and possums that harbour Mycobacterium ulcerans are active.
Stop its spread by stopping mozzies breeding
The mosquito in this study primarily responsible for the bacteria’s spread is Aedes notoscriptus, a mosquito that lays its eggs around water in containers in backyard habitats.
Controlling “backyard” mosquitoes is a critical part of reducing the risk of many global mosquito-borne disease, especially dengue and now Buruli ulcer.
You can reduce places where water collects after rainfall, such as potted plant saucers, blocked gutters and drains, unscreened rainwater tanks, and a wide range of plastic buckets and other containers. These should all be either emptied at least weekly or, better yet, thrown away or placed under cover.

Cameron Webb (NSW Health Pathology)
There is a role for insecticides too. While residual insecticides applied to surfaces around the house and garden will reduce mosquito populations, they can also impact other, beneficial, insects. Judicious use of such sprays is recommended. But there are ecological safe insecticides that can be applied to water-filled containers (such as ornamental ponds, fountains, stormwater pits and so on).
Recent research also indicates new mosquito-control approaches that use mosquitoes themselves to spread insecticides may soon be available.
How to protect yourself from bites
The first line of defence will remain personal protection measures against mosquito bites.
Covering up with loose fitted long sleeved shirts, long pants, and covered shoes will provide physical protection from mosquitoes.
Applying topical insect repellent to all exposed areas of skin has been proven to provide safe and effective protection from mosquito bites. Repellents should include diethytolumide (DEET), picaridin or oil of lemon eucalyptus.
While the rise in Buruli ulcer is a significant health concern, so too are many other mosquito-borne diseases. The steps to avoid mosquito bites and exposure to Mycobacteriam ulcerans will also protect against viruses such as Ross River, Barmah Forest, Japanese encephalitis, and Murray Valley encephalitis.
Cameron Webb, Clinical Associate Professor and Principal Hospital Scientist, University of Sydney; Peter Mee, Adjunct Associate Lecturer, School of Applied Systems Biology, La Trobe University; Stacey Lynch, Team Leader- Mammalian infection disease research, CSIRO, and Tim Stinear, Professor of Microbiology, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
All of your hepatitis B vaccine questions answered
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hepatitis B is a viral infection that can cause liver disease in people of any age or background. Vaccination is 95 percent effective against the virus. But in recent years, false claims, rumors, and myths about the hepatitis B vaccine have become increasingly common.
Here’s everything you need to know about the lifesaving hepatitis B vaccine.
What is hepatitis B?
Hepatitis B is a liver infection caused by the hepatitis B virus. The virus attacks the liver, causing severe short-term and long-term infections.
Short-term hepatitis B infections may cause “fever, fatigue, loss of appetite, nausea, vomiting, jaundice (yellow skin or eyes, dark urine, clay-colored bowel movements), and pain in the muscles, joints, and stomach,” according to the Centers for Disease Control and Prevention.
A long-term hepatitis B infection occurs when the virus stays in the body beyond the initial infection, causing chronic illness. Hepatitis B infections become chronic in 90 percent of infected infants, half of infected young children, and between 5 to 10 percent of infected adults.
“Most people who go on to develop chronic hepatitis B do not have symptoms, but it is still very serious and can lead to liver damage (cirrhosis), liver cancer, and death. Chronically infected people can spread hepatitis B virus to others, even if they do not feel or look sick themselves,” says the CDC.
How does the hepatitis B virus spread?
The hepatitis B virus is spread through body fluids, including blood, semen, and saliva. It can also be transmitted from birthing parent to child during pregnancy and childbirth.
“While hepatitis B is an infection that lives in bodily fluids, it can survive outside the human body for several days, which means that sharing contaminated household products is a possible source of infection,” said Dr. Christopher Labos, a McGill University cardiologist and epidemiologist, in a 2019 article.
In 2022, over 250 million people worldwide had chronic hepatitis B, and 1.1 million died from the disease. Most of the deaths were from liver damage and liver cancer. Less than 15 percent of people living with hepatitis B have been diagnosed.
How well does the vaccine protect against hepatitis B?
Hepatitis B vaccination is up to 95 percent effective, providing lasting—and possibly lifelong—protection against the virus. Depending on when the first dose is given, the complete vaccine series consists of two to three doses.
The vaccine is most effective for infants and children. The CDC recommends that infants receive it at birth for the most protection.
The first dose is followed by two to three additional doses administered before 18 months. Children, adolescents, and adults who weren’t vaccinated as infants should also receive the vaccine.
Vaccination is particularly important for high-risk groups, including health workers and those who are in close contact with individuals living with chronic hepatitis B, people who use intravenous drugs, and people receiving blood transfusions, dialysis, or organ transplants.
Is the vaccine safe?
Vaccines against hepatitis B were first developed in the 1980s, and they have been proven safe for decades. They have a low risk of serious side effects and are safe enough to be given to newborns, pregnant people, and immunocompromised people.
We also know hepatitis B vaccines work: “Between 1990 (about the time when universal hepatitis B vaccinations started) and 2006, the rate of hepatitis B infection fell by 81 percent to the lowest level ever recorded, and the decline was greatest among children,” added Labos.
Hepatitis B rates have continued to decline across all age groups, with the U.S. exceeding its goal of reducing new hepatitis B infections by 20 percent.
Why do doctors recommend the vaccine for babies?
Hepatitis B vaccination helps protect infants from a lifetime of potentially life-threatening infections and complications. Nine out of 10 unvaccinated infants infected with hepatitis B will develop chronic infections, which increases their risk of liver failure and liver cancer.
The hepatitis B vaccine is administered at birth to help prevent the virus from being transmitted from birthing parent to child. It also helps protect infants who might be in close contact with someone with hepatitis B. This is particularly important because most people who have hepatitis are undiagnosed.
Have more questions? Talk to your health care provider to learn more about hepatitis B vaccination.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Shrimp vs Caviar – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing shrimp to caviar, we picked the caviar.
Why?
Both of these seafoods share a common history (also shared with lobster, by the way) of “nutrient-dense peasant-food that got gentrified and now it’s more expensive despite being easier to source”. But, cost and social quirks aside, what are their strengths and weaknesses?
In terms of macros, both are high in protein, but caviar is much higher in fat. You may be wondering: are the fats healthy? And the answer is that it’s a fairly even mix between monounsaturated (healthy), polyunsaturated (healthy), and saturated (unhealthy). The fact that caviar is generally enjoyed in very small portions is its saving grace here, but quantity for quantity, shrimp is the natural winner on macros.
…unless we take into account the omega-3 and omega-6 balance, in which case, it’s worthy of note that caviar has more omega-3 (which most people could do with consuming more of) while shrimp has more omega-6 (which most people could do with consuming less of).
When it comes to vitamins, caviar has more of vitamins A, B1, B2, B5, B6, B9, B12, D, K, and choline; nor are the margins small in most cases, being multiples (or sometimes, tens of multiples) higher. Shrimp, meanwhile, boasts only more vitamin B3.
In the category of minerals, caviar leads with more calcium, iron, magnesium, manganese, phosphorus, potassium, and selenium, while shrimp has more copper and zinc.
All in all, while shrimp has its benefits for being lower in fat (and thus also, for those whom that may interest, lower in calories), caviar wins the day by virtue of its overwhelming nutritional density.
Want to learn more?
You might like to read:
What Omega-3 Fatty Acids Really Do For Us
Take care!
Share This Post
-
Eat To Beat Chronic Fatigue!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Eat To Beat Chronic Fatigue
Chronic fatigue is on the rise, and it can make life a living Hell. Days blur into one, and you try to take each day as it comes, but sometimes several days gang up on you at once.
You probably know some lifestyle changes that might help—if only you had the energy to implement them.
You’d like to eat well, but you need to…
- Buy the fresh produce (and take a little rest after)
- Put the groceries away (and take a little rest after)
- Wash the vegetables (and take a little rest after)
- Chop the things as necessary (and take a little rest after)
- Cook dinner (and take a little rest after)
…and now you’re too exhausted to eat it.
So, what can be done?
First, avoid things that cause inflammation, as this is a major contributor to chronic fatigue. You might like our previous main feature:
Next up, really do stay hydrated. It’s less about quantity, and more about ubiquity. Hydrate often.
Best is if you always have some (hydrating) drink on the go.
Do experiment with your diet, and/but keep a food journal of what you eat and how you feel 30–60 minutes after eating it. Only make one change at a time, otherwise you won’t know which change made the difference.
Notice what patterns emerge over time, and adjust your ingredients accordingly.
Limit your caffeine intake. We know that sometimes it seems like the only way to get through the day, but you will always crash later, because it was only ever taxing your adrenal system (thus: making you more tired in the long run) and pulling the wool over the eyes of your adenosine receptors (blocking you from feeling how tired you are, but not actually reducing your body’s tiredness).
Put simply, caffeine is the “payday loan” of energy.
Eat more non-starchy vegetables, and enjoy healthy fats. Those healthy fats can come from nuts and seeds, avocado, or fish (not fried, though!).
The non-starchy vegetables will boost your vitamins and fiber while being easy on your beleaguered metabolism, while the healthy fats will perk up your energy levels without spiking insulin like sugars would.
Pay the fatigue tax up front. What this means is… Instead of throwing away vegetables that didn’t get used because it would take too much effort and you just need an easier dinner today, buy ready-chopped vegetables, for example.
And if you buy vegetables frozen, they’re also often not only cheaper, but also (counterintuitively) contain more nutrients.
A note of distinction:
Many more people have chronic fatigue (the symptom: being exhausted all the time) than have chronic fatigue syndrome (the illness: myalgic encephalomyelitis).
This is because fatigue can be a symptom of many, many other conditions, and can be heavily influenced by lifestyle factors too.
A lot of the advice for dealing with chronic fatigue is often the same in both cases, but some will be different, because for example:
- If your fatigue is from some other condition, that condition probably impacts what lifestyle factors you are (and are not) able to change, too
- If your fatigue is from lifestyle factors, that hopefully means you can change those and enjoy less fatigue…
- But if it’s not from lifestyle factors, as in ME/CFS, then advice to “exercise more” etc is not going to help so much.
There are ways to know the difference though:
Check out: Do You Have Chronic Fatigue Syndrome?
Share This Post
Related Posts
-
Pine Nuts vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pine nuts to pecans, we picked the pine nuts.
Why?
Both have their merits!
In terms of macros, pine nuts have more protein while pecans have more fiber. They’re about equal on fats, although pine nuts have more polyunsaturated fat and pecans have more monounsaturated fat, of which, both are healthy. They’re also about equal on carbs. So really it comes down to the subjective choice between prioritizing protein and prioritizing fiber. On principle, we pick fiber, which gives the win to pecans, but your preference in this regard may differ; prioritizing the protein would give the win to pine nuts.
In the category of vitamins, pine nuts have more of vitamins B2, B3, B9, E, K, and choline, while pecans have more of vitamins A, B1, B5, B6, and C. Thus, a 6:5 marginal win for pine nuts.
Looking at the minerals, pine nuts have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while pecans have more calcium and selenium. An easy win for pine nuts this time.
Adding up the sections makes for a win for pine nuts, but of course, enjoy either or (preferably) both; diversity is good!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Metabolical – by Dr. Robert Lustig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The premise of this book itself is not novel: processed food is bad, food giants lie to us, and eating better makes us less prone to disease (especially metabolic disease).
What this book does offer that’s less commonly found is a comprehensive guide, a walkthrough of each relevant what and why and how, with plenty of good science and practical real-world examples.
In terms of unique selling points, perhaps the greatest strength of this book is its focus on two things in particular that affect many aspects of health: looking after our liver, and looking after our gut.
The style is… A little dramatic perhaps, but that’s just the style; there’s no hyperbole, he is stating well-established scientific facts.
Bottom line: very much of chronic disease would be a lot less diseasey if we all ate with these aspects of our health in mind. This book’s a comprehensive guide to that.
Click here to check out Metabolical, and let food be thy medicine!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: