Osteoarthritis Of The Knee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Very informative thank you. And made me think. I am a 72 yr old whitewoman, have never used ( or even been offered) HRT since menopause ~15 yrs ago. Now I’m wondering if it would have delayed the onset of osteoarthritis ( knee) and give me more energy in general. And is it wise to start taking hrt after being without those hormones for so long?❞
(this was in response to our article about menopausal HRT)
Thanks for writing! To answer your first question, obviously we can never know for sure now, but it certainly is possible, per for example a large-ish (n=1003) study of women aged 45–64, in which:
- Those with HRT were significantly less likely to have knee arthritis than those without
- However, to enjoy this benefit depended on continued use (those who used it for a bit and then stopped did not enjoy the same results)
- While it made a big difference to knee arthritis, it made only a small (but still beneficial) difference to wrist/hand arthritis.
We could hypothesize that this is because the mechanism of action is more about strengthening the bones (proofing against osteoporosis is one of the main reasons many people take HRT) and cartilage than it is against inflammation directly.
Since the knee is load-bearing and the hand/wrist joints usually are not, this would mean the HRT strengthening the bones makes a big difference to the “wear and tear” aspect of potential osteoarthritis of the knee, but not the same level of benefit for the hand/wrist, which is less about wear and tear and more about inflammatory factors. But that latter, about it being load-bearing, is just this writer’s hypothesis as to why the big difference.
The researchers do mention:
❝In OA the mechanisms by which HRT might act are highly speculative, but could entail changes in cartilage repair or bone turnover, perhaps with cytokines such as interleukin 6, for example.❞
What is clear though, is that it does indeed appear to have a protective effect against osteoarthritis of the knee.
With regard to the timing, the researchers do note:
❝Why as little as three years of HRT should have a demonstrable effect is unclear. Given the difficulty in ascertaining when the disease starts, it is hard to be sure of the importance of the timing of HRT, and whether early or subclinical disease was present.
These results taken together suggest that HRT has a metabolic action that is only effective if given continuously, perhaps by preventing disease initiation; once HRT is stopped there might be a ‘rebound’ effect, explaining the rapid return to normal risk❞
~ Ibid.
You can read the study here:
On whether it is worth it now…
Again, do speak with an endocrinologist because your situation may vary, but:
- hormones are simply messengers, and your body categorically will respond to those messages regardless of age, or time elapsed without having received such a message. Whether it will repair all damage done is another matter entirely, but it would take a biological miracle for it to have no effect at all.
- anecdotally, many women do enjoy life-changing benefits upon starting HRT at your age and older!
(We don’t like to rely on “anecdotally”, but we couldn’t find studies isolating according to “length of time since menopause”—we’ll keep an eye out and if we find something in the future, we’ll mention it!)
Meanwhile, take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kidney Beans vs Fava Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to fava beans, we picked the kidney beans.
Why?
It’s a simple and straightforward one today!
The macronutrient profiles are mostly comparable, but kidney beans do have a little more protein and a little more fiber.
In the category of vitamins, kidney beans have more of vitamins B1, B5, B6, B9, C, E, & K, while fava beans boast only more of vitamins B2 and B3. They are both equally good sources of choline, but the general weight of vitamins is very much in kidney beans’ favor, with a 7:2 lead, most of which have generous margins.
When it comes to minerals, kidney beans have more iron, phosphorus, and potassium, while fava beans have more copper and selenium. They’re both equally good sources of other minerals they both contain. Still, a 3:2 victory for kidney beans on the mineral front.
Adding up the moderate victory on macros, the strong victory on vitamins, and the slight victory on minerals, all in all makes for a clear win for kidney beans.
Still, enjoy both! Diversity is healthy.
Want to learn more?
You might like to read:
Chickpeas vs Black Beans – Which is Healthier?
Take care!
Share This Post
-
Constipation increases your risk of a heart attack, new study finds – and not just on the toilet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you Google the terms “constipation” and “heart attack” it’s not long before the name Elvis Presley crops up. Elvis had a longstanding history of chronic constipation and it’s believed he was straining very hard to poo, which then led to a fatal heart attack.
We don’t know what really happened to the so-called King of Rock “n” Roll back in 1977. There were likely several contributing factors to his death, and this theory is one of many.
But after this famous case researchers took a strong interest in the link between constipation and the risk of a heart attack.
This includes a recent study led by Australian researchers involving data from thousands of people.
Elvis Presley was said to have died of a heart attack while straining on the toilet. But is that true? Kraft74/Shutterstock Are constipation and heart attacks linked?
Large population studies show constipation is linked to an increased risk of heart attacks.
For example, an Australian study involved more than 540,000 people over 60 in hospital for a range of conditions. It found constipated patients had a higher risk of high blood pressure, heart attacks and strokes compared to non-constipated patients of the same age.
A Danish study of more than 900,000 people from hospitals and hospital outpatient clinics also found that people who were constipated had an increased risk of heart attacks and strokes.
It was unclear, however, if this relationship between constipation and an increased risk of heart attacks and strokes would hold true for healthy people outside hospital.
These Australian and Danish studies also did not factor in the effects of drugs used to treat high blood pressure (hypertension), which can make you constipated.
Researchers have studied thousands of people to see if there’s a link between constipation and heart attacks. fongbeerredhot/Shutterstock How about this new study?
The recent international study led by Monash University researchers found a connection between constipation and an increased risk of heart attacks, strokes and heart failure in a general population.
The researchers analysed data from the UK Biobank, a database of health-related information from about half a million people in the United Kingdom.
The researchers identified more than 23,000 cases of constipation and accounted for the effect of drugs to treat high blood pressure, which can lead to constipation.
People with constipation (identified through medical records or via a questionnaire) were twice as likely to have a heart attack, stroke or heart failure as those without constipation.
The researchers found a strong link between high blood pressure and constipation. Individuals with hypertension who were also constipated had a 34% increased risk of a major heart event compared to those with just hypertension.
The study only looked at the data from people of European ancestry. However, there is good reason to believe the link between constipation and heart attacks applies to other populations.
A Japanese study looked at more than 45,000 men and women in the general population. It found people passing a bowel motion once every two to three days had a higher risk of dying from heart disease compared with ones who passed at least one bowel motion a day.
How might constipation cause a heart attack?
Chronic constipation can lead to straining when passing a stool. This can result in laboured breathing and can lead to a rise in blood pressure.
In one Japanese study including ten elderly people, blood pressure was high just before passing a bowel motion and continued to rise during the bowel motion. This increase in blood pressure lasted for an hour afterwards, a pattern not seen in younger Japanese people.
One theory is that older people have stiffer blood vessels due to atherosclerosis (thickening or hardening of the arteries caused by a build-up of plaque) and other age-related changes. So their high blood pressure can persist for some time after straining. But the blood pressure of younger people returns quickly to normal as they have more elastic blood vessels.
As blood pressure rises, the risk of heart disease increases. The risk of developing heart disease doubles when systolic blood pressure (the top number in your blood pressure reading) rises permanently by 20 mmHg (millimetres of mercury, a standard measure of blood pressure).
The systolic blood pressure rise with straining in passing a stool has been reported to be as high as 70 mmHg. This rise is only temporary but with persistent straining in chronic constipation this could lead to an increased risk of heart attacks.
High blood pressure from straining on the toilet can last after pooing, especially in older people. Andrey_Popov/Shutterstock Some people with chronic constipation may have an impaired function of their vagus nerve, which controls various bodily functions, including digestion, heart rate and breathing.
This impaired function can result in abnormalities of heart rate and over-activation of the flight-fight response. This can, in turn, lead to elevated blood pressure.
Another intriguing avenue of research examines the imbalance in gut bacteria in people with constipation.
This imbalance, known as dysbiosis, can result in microbes and other substances leaking through the gut barrier into the bloodstream and triggering an immune response. This, in turn, can lead to low-grade inflammation in the blood circulation and arteries becoming stiffer, increasing the risk of a heart attack.
This latest study also explored genetic links between constipation and heart disease. The researchers found shared genetic factors that underlie both constipation and heart disease.
What can we do about this?
Constipation affects around 19% of the global population aged 60 and older. So there is a substantial portion of the population at an increased risk of heart disease due to their bowel health.
Managing chronic constipation through dietary changes (particularly increased dietary fibre), increased physical activity, ensuring adequate hydration and using medications, if necessary, are all important ways to help improve bowel function and reduce the risk of heart disease.
Vincent Ho, Associate Professor and clinical academic gastroenterologist, Western Sydney University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Why Going Gluten-Free Could Be A Bad Idea
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is A Gluten-Free Diet Right For You?
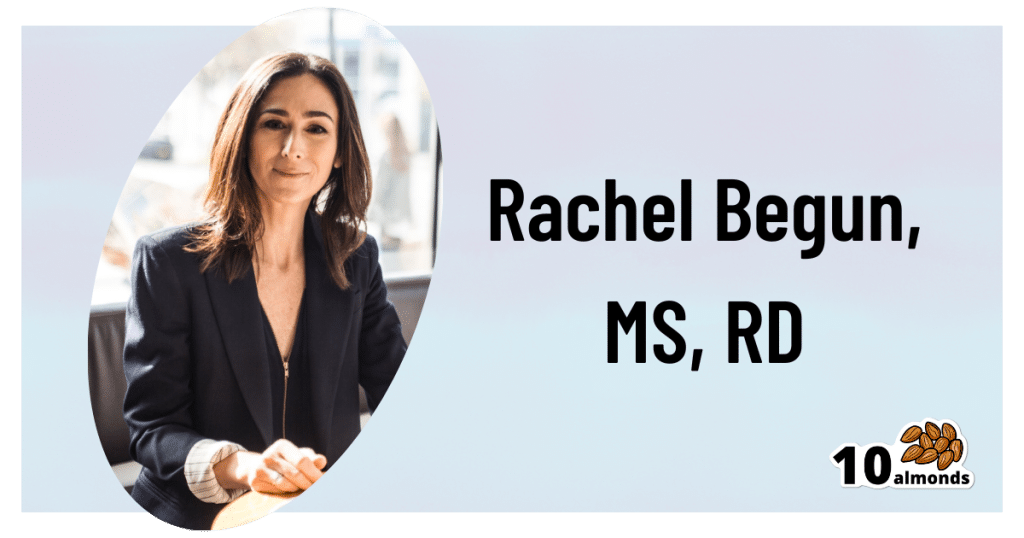
This is Rachel Begun, MS, RD. She’s a nutritionist who, since her own diagnosis with Celiac disease, has shifted her career into a position of educating the public (and correcting misconceptions) about gluten sensitivity, wheat allergy, and Celiac disease. In short, the whole “gluten-free” field.
First, a quick recap
We’ve written on this topic ourselves before; here’s what we had to say:
On “Everyone should go gluten-free”
Some people who have gone gluten-free are very evangelical about the lifestyle change, and will advise everyone that it will make them lose weight, have clearer skin, more energy, and sing well, too. Ok, maybe not the last one, but you get the idea—a dietary change gets seen as a cure-all.
And for some people, it can indeed make a huge difference!
Begun urges us to have a dose of level-headedness in our approach, though.
Specifically, she advises:
- Don’t ignore symptoms, and/but…
- Don’t self-diagnose
- Don’t just quit gluten
One problem with self-diagnosis is that we can easily be wrong:
But why is that a problem? Surely there’s not a health risk in skipping the gluten just to be on the safe side? As it turns out, there actually is:
If we self-diagnose incorrectly, Begun points out, we can miss the actual cause of the symptoms, and by cheerfully proclaiming “I’m allergic to gluten” or such, a case of endometriosis, or Hashimoto’s, or something else entirely, might go undiagnosed and thus untreated.
“Oh, I feel terrible today, there must have been some cross-contamination in my food” when in fact, it’s an undiagnosed lupus flare-up, that kind of thing.
Similarly, just quitting gluten “to be on the safe side” can mask a different problem, if wheat consumption (for example) contributed to, but did not cause, some ailment.
In other words: it could reduce your undesired symptoms, but in so doing, leave a more serious problem unknown.
Instead…
If you suspect you might have a gluten sensitivity, a wheat allergy, or even Celiac disease, get yourself tested, and take professional advice on proceeding from there.
How? Your physician should be able to order the tests for you.
You can also check out resources available here:
Celiac Disease Foundation | How do I get tested?
Or for at-home gluten intolerance tests, here are some options weighed against each other:
MNT | 5 gluten intolerance tests and considerations
Want to learn more?
Begun has a blog:
Rachel Begun | More than just recipes
(it is, in fact, just recipes—but they are very simple ones!)
You also might enjoy this interview, in which she talks about gluten sensitivity, celiac disease, and bio-individuality:
Want to watch it, but not right now? Bookmark it for later
Take care!
Share This Post
Related Posts
-
5 Stretches To Relieve The Pain From Sitting & Poor Posture
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sitting is not good for the health, yes often it’s a necessity of modern life, especially if driving. To make things worse, it can often be difficult to remember to maintain good posture the rest of the time, if it’s not a habit. So, while reducing sitting and improving posture are both very good things to do, here are 5 stretches to mitigate the damage meanwhile:
Daily doses:
These are best done at a rate of 2–3 sets daily:
Cat-Cow Stretch:
- Benefits: eases spinal tension, boosts flexibility, improves posture.
- How to: start on all fours, alternate between arching and rounding your back while syncing with your breath (10-15 times).
Butterfly Stretch:
- Benefits: loosens tight hips, improves lower back flexibility, and enhances mobility for activities like squats.
- How to: sit with soles of feet together, let knees fall toward the floor, lean forward slightly, and hold for 30 seconds to 1 minute.
Supine Twist:
- Benefits: unlocks the spine, relieves post-workout tension, and relaxes the shoulders and hips.
- How to: lie on your back, bend knees, twist to one side while keeping shoulders grounded, and hold for 30 seconds to 1 minute per side.
Calf Stretch:
- Benefits: improves ankle mobility, loosens tight calves, and prevents injuries like Achilles tendinitis.
- How to: stand facing a wall, extend one leg back with the heel on the ground, lean into the stretch, or use a step for deeper stretches. Hold for 30 seconds to 1 minute per leg.
Child’s Pose:
- Benefits: decompresses the spine, relaxes hips, and relieves tension in back and thighs.
- How to: start on hands and knees, sit back onto your heels, stretch arms forward, and rest forehead on the mat. Hold for 30 seconds to 1 minute.
For more on each of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
10 Tips To Reduce Morning Pain & Stiffness With Arthritis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Has Nobody Told Me This Before? – by Dr. Julie Smith
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superficially, this can be called a “self-help” book, but that undersells it rather. It’s a professionally-written (as in, by a professional psychologist) handbook full of resources. Its goal? Optimizing your mental health to help you stay resilient no matter what life throws your way.
While the marketing of this book is heavily centered around Dr. Smith’s Internet Celebrity™ status, a lot of her motivation for writing it seems to be precisely so that she can delve deeper into the ideas that her social media “bites” don’t allow room for.
Many authors of this genre pad their chapters with examples; there are no lengthy story-telling asides here, and her style doesn’t need them. She knows her field well, and knows well how to communicate the ideas that may benefit the reader.
The main “meat” of the book? Tips, tricks, guides, resources, systems, flowcharts, mental frameworks, and “if all else fails, do this” guidance. The style of the book is clear and simple, with very readable content that she keeps free from jargon without “dumbing down” or patronizing the reader.
All in all, a fine set of tools for anyone’s “getting through life” toolbox.
Get Your Personal Copy Of “Why Has Nobody Told Me This Before?” on Amazon Now!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Hospital Kept a Brain-Damaged Patient on Life Support to Boost Statistics. His Sister Is Now Suing for Malpractice.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
In 2018, Darryl Young was hoping for a new lease on life when he received a heart transplant at a New Jersey hospital after years of congestive heart failure. But he suffered brain damage during the procedure and never woke up.
The following year, a ProPublica investigation revealed that Young’s case was part of a pattern of heart transplants that had gone awry at Newark Beth Israel Medical Center in 2018. The spate of bad outcomes had pushed the center’s percentage of patients still alive one year after surgery — a key benchmark — below the national average. Medical staff were under pressure to boost that metric. ProPublica published audio recordings from meetings in which staff discussed the need to keep Young alive for a year, because they feared another hit to the program’s survival rate would attract scrutiny from regulators. On the recordings, the transplant program’s director, Dr. Mark Zucker, cautioned his team against offering Young’s family the option of switching from aggressive care to comfort care, in which no lifesaving efforts would be made. He acknowledged these actions were “very unethical.”
ProPublica’s revelations horrified Young’s sister Andrea Young, who said she was never given the full picture of her brother’s condition, as did the findings of a subsequent federal regulator’s probe that determined that the hospital was putting patients in “immediate jeopardy.” Last month, she filed a medical malpractice lawsuit against the hospital and members of her brother’s medical team.
The lawsuit alleges that Newark Beth Israel staff were “negligent and deviated from accepted standards of practice,” leading to Young’s tragic medical outcome.
Defendants in the lawsuit haven’t yet filed responses to the complaint in court documents. But spokesperson Linda Kamateh said in an email that “Newark Beth Israel Medical Center is one of the top heart transplant programs in the nation and we are committed to serving our patients with the highest quality of care. As this case is in active litigation, we are unable to provide further detail.” Zucker, who is no longer on staff at Newark Beth Israel, didn’t respond to requests for comment. His attorney also didn’t respond to calls and emails requesting comment.
Zucker also didn’t respond to requests for comment from ProPublica in 2018; Newark Beth Israel at the time said in a statement, made on behalf of Zucker and other staff, that “disclosures of select portions of lengthy and highly complex medical discussions, when taken out of context, may distort the intent of conversations.”
The lawsuit alleges that Young suffered brain damage as a result of severely low blood pressure during the transplant surgery. In 2019, when the federal Centers for Medicare and Medicaid Services scrutinized the heart transplant program following ProPublica’s investigation, the regulators found that the hospital had failed to implement corrective measures even after patients suffered, leading to further harm. For example, one patient’s kidneys failed after a transplant procedure in August 2018, and medical staff made recommendations internally to increase the frequency of blood pressure measurement during the procedure, according to the lawsuit. The lawsuit alleges that the hospital didn’t implement its own recommendations and that one month later, “these failures were repeated” in Young’s surgery, leading to brain damage.
The lawsuit also alleges that Young wasn’t asked whether he had an advance directive, such as a preference for a do-not-resuscitate order, despite a hospital policy stating that patients should be asked at the time of admission. The lawsuit also noted that CMS’ investigation found that Andrea Young was not informed of her brother’s condition.
Andrea Young said she understands that mistakes can happen during medical procedures, “however, it’s their duty and their responsibility to be honest and let the family know exactly what went wrong.” Young said she had to fight to find out what was going on with her brother, at one point going to the library and trying to study medical books so she could ask the right questions. “I remember as clear as if it were yesterday, being so desperate for answers,” she said.
Andrea Young said that she was motivated to file the lawsuit because she wants accountability. “Especially with the doctors never, from the outset, being forthcoming and truthful about the circumstances of my brother’s condition, not only is that wrong and unethical, but it took a lot away from our entire family,” she said. “The most important thing to me is that those responsible be held accountable.”
ProPublica’s revelation of “a facility putting its existence over that of a patient is a scary concept,” said attorney Jonathan Lomurro, who’s representing Andrea Young in this case with co-counsel Christian LoPiano. Besides seeking damages for Darryl Young’s children, “we want to call attention to this so it doesn’t happen again,” Lomurro said.
The lawsuit further alleges that medical staff at Newark Beth Israel invaded Young’s privacy and violated the Health Insurance Portability and Accountability Act, more commonly known as HIPAA, by sharing details of his case with the media without his permission. “We want people to be whistleblowers and want information out,” but that information should be told to patients and their family members directly, Lomurro said.
The 2019 CMS investigation determined that Newark Beth Israel’s program placed patients in “immediate jeopardy,” the most serious level of violation, and required the hospital to implement corrective plans. Newark Beth Israel did not agree with all of the regulator’s findings and in a statement at the time said that the CMS team lacked the “evidence, expertise and experience” to assess and diagnose patient outcomes.
The hospital did carry out the corrective plans and continues to operate a heart transplant program today. The most recent federal data, based on procedures from January 2021 through June 2023, shows that the one year probability of survival for a patient at Newark Beth is lower than the national average. It also shows that the number of graft failures, including deaths, in that time period was higher than the expected number of deaths for the program.
Andrea Young said she’s struggled with a feeling of emptiness in the years after her brother’s surgery. They were close and called each other daily. “There’s nothing in the world that can bring my brother back, so the only solace I will have is for the ones responsible to be held accountable,” she said. Darryl Young died on Sept 12, 2022, having never woken up after the transplant surgery.
A separate medical malpractice lawsuit filed in 2020 by the wife of another Newark Beth Israel heart transplant patient who died after receiving an organ infected with a parasitic disease is ongoing. The hospital has denied the allegations in court filing. The state of New Jersey, employer of the pathologists named in the case, settled for $1.7 million this month, according to the plaintiff’s attorney Christian LoPiano. The rest of the case is ongoing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: