How the stress of playing chess can be fatal
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The death of a chess player in the middle of a match at the world’s most prestigious competition may have shocked those who view the game as a relaxing pastime. Kurt Meier, 67, collapsed during his final match in the tournament and died in hospital later that day. But chess, like any other game or sport, can lead to an immense amount of stress, which can be bad for a competitor’s physical health too.
We tend to associate playing sport or games with good health and well-being. And there are a countless number of studies showing playing games has an association with feeling happier. While this argument is true for recreational players, the story can be different for the elite, where success and failure are won and lost by the finest margins and where winning can mean funding and a future, and losing can mean poverty and unemployment. If this is the case, can being successful at a sport or game actually be bad for you?
Competitive anxiety
Elite competition can be stressful because the outcome is so important to the competitors. We can measure stress using a whole range of physiological indicators such as heart rate and temperature, and responses such as changes in the intensity of our emotions.
Emotions provide a warning of threat. So if you feel that achieving your goal is going to be difficult, then expect to feel intense emotions. The leading candidate that signals we are experiencing stress is anxiety, characterised by thoughts of worry, fears of dread about performance, along with accompanying physiological responses such as increased heart rate and sweaty palms. If these symptoms are experienced regularly or chronically, then this is clearly detrimental to health.
This stress response is probably not restricted to elite athletes. Intense emotions are linked to trying to achieve important goals and while it isn’t the only situation where it occurs, it is just very noticeable in sport.
The causes of stress
It makes more sense to focus on what the causes of stress are rather than where we experience it. The principle is that the more important the goal is to achieve, then the greater the propensity for the situation to intensify emotions.
Emotions intensify also by the degree of uncertainty and competing, at whatever level of a sport, is uncertain when the opposition is trying its hardest to win the contest and also has a motivation to succeed. The key point is that almost all athletes at any level can suffer bouts of stress, partly due to high levels of motivation.
A stress response is also linked to how performance is judged and reported. Potentially stressful tasks tend to be ones where performance is public and feedback is immediate. In chess – as with most sporting contests – we see who the winner is and can start celebrating success or commiserating failure as soon as the game is over.
There are many tasks which have similar features. Giving a speech in public, taking an academic examination, or taking your driving test are all examples of tasks that can illicit stress. Stress is not restricted to formal tasks but can also include social tasks. Asking a potential partner for a date, hand in marriage, and meeting the in-laws for the first time can be equally stressful.
Winning a contest or going on a date relate to higher-order goals about how we see ourselves. If we define ourselves as “being a good player” or “being attractive or likeable” then contrasting information is likely to associate with unpleasant emotions. You will feel devastated if you are turned down when asking someone out on a date, for instance, and if this was repeated, it could lead to reduced self-esteem and depression.
The key message here is to recognise what your goals are and think about how important they are. If you want to achieve them with a passion and if the act of achieving them leads to intense and sometimes unwanted emotions, then it’s worth thinking about doing some work to manage these emotions.
Andrew Lane, Professor in Sport and Learning, University of Wolverhampton
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Can a drug like Ozempic help treat addictions to alcohol, opioids or other substances?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (sold as Ozempic, Wegovy and Rybelsus) was initially developed to treat diabetes. It works by stimulating the production of insulin to keep blood sugar levels in check.
This type of drug is increasingly being prescribed for weight loss, despite the fact it was initially approved for another purpose. Recently, there has been growing interest in another possible use: to treat addiction.
Anecdotal reports from patients taking semaglutide for weight loss suggest it reduces their appetite and craving for food, but surprisingly, it also may reduce their desire to drink alcohol, smoke cigarettes or take other drugs.
But does the research evidence back this up?
Animal studies show positive results
Semaglutide works on glucagon-like peptide-1 receptors and is known as a “GLP-1 agonist”.
Animal studies in rodents and monkeys have been overwhelmingly positive. Studies suggest GLP-1 agonists can reduce drug consumption and the rewarding value of drugs, including alcohol, nicotine, cocaine and opioids.
Out team has reviewed the evidence and found more than 30 different pre-clinical studies have been conducted. The majority show positive results in reducing drug and alcohol consumption or cravings. More than half of these studies focus specifically on alcohol use.
However, translating research evidence from animal models to people living with addiction is challenging. Although these results are promising, it’s still too early to tell if it will be safe and effective in humans with alcohol use disorder, nicotine addiction or another drug dependence.
What about research in humans?
Research findings are mixed in human studies.
Only one large randomised controlled trial has been conducted so far on alcohol. This study of 127 people found no difference between exenatide (a GLP-1 agonist) and placebo (a sham treatment) in reducing alcohol use or heavy drinking over 26 weeks.
In fact, everyone in the study reduced their drinking, both people on active medication and in the placebo group.
However, the authors conducted further analyses to examine changes in drinking in relation to weight. They found there was a reduction in drinking for people who had both alcohol use problems and obesity.
For people who started at a normal weight (BMI less than 30), despite initial reductions in drinking, they observed a rebound increase in levels of heavy drinking after four weeks of medication, with an overall increase in heavy drinking days relative to those who took the placebo.
There were no differences between groups for other measures of drinking, such as cravings.

Some studies show a rebound increase in levels of heavy drinking. Deman/Shutterstock In another 12-week trial, researchers found the GLP-1 agonist dulaglutide did not help to reduce smoking.
However, people receiving GLP-1 agonist dulaglutide drank 29% less alcohol than those on the placebo. Over 90% of people in this study also had obesity.
Smaller studies have looked at GLP-1 agonists short-term for cocaine and opioids, with mixed results.
There are currently many other clinical studies of GLP-1 agonists and alcohol and other addictive disorders underway.
While we await findings from bigger studies, it’s difficult to interpret the conflicting results. These differences in treatment response may come from individual differences that affect addiction, including physical and mental health problems.
Larger studies in broader populations of people will tell us more about whether GLP-1 agonists will work for addiction, and if so, for whom.
How might these drugs work for addiction?
The exact way GLP-1 agonists act are not yet well understood, however in addition to reducing consumption (of food or drugs), they also may reduce cravings.
Animal studies show GLP-1 agonists reduce craving for cocaine and opioids.
This may involve a key are of the brain reward circuit, the ventral striatum, with experimenters showing if they directly administer GLP-1 agonists into this region, rats show reduced “craving” for oxycodone or cocaine, possibly through reducing drug-induced dopamine release.
Using human brain imaging, experimenters can elicit craving by showing images (cues) associated with alcohol. The GLP-1 agonist exenatide reduced brain activity in response to an alcohol cue. Researchers saw reduced brain activity in the ventral striatum and septal areas of the brain, which connect to regions that regulate emotion, like the amygdala.
In studies in humans, it remains unclear whether GLP-1 agonists act directly to reduce cravings for alcohol or other drugs. This needs to be directly assessed in future research, alongside any reductions in use.
Are these drugs safe to use for addiction?
Overall, GLP-1 agonists have been shown to be relatively safe in healthy adults, and in people with diabetes or obesity. However side effects do include nausea, digestive troubles and headaches.
And while some people are OK with losing weight as a side effect, others aren’t. If someone is already underweight, for example, this drug might not be suitable for them.
In addition, very few studies have been conducted in people with addictive disorders. Yet some side effects may be more of an issue in people with addiction. Recent research, for instance, points to a rare risk of pancreatitis associated with GLP-1 agonists, and people with alcohol use problems already have a higher risk of this disorder.
Other drugs treatments are currently available
Although emerging research on GLP-1 agonists for addiction is an exciting development, much more research needs to be done to know the risks and benefits of these GLP-1 agonists for people living with addiction.
In the meantime, existing effective medications for addiction remain under-prescribed. Only about 3% of Australians with alcohol dependence, for example, are prescribed medication treatments such as like naltrexone, acamprosate or disulfiram. We need to ensure current medication treatments are accessible and health providers know how to prescribe them.
Continued innovation in addiction treatment is also essential. Our team is leading research towards other individualised and effective medications for alcohol dependence, while others are investigating treatments for nicotine addiction and other drug dependence.
Read the other articles in The Conversation’s Ozempic series here.
Shalini Arunogiri, Addiction Psychiatrist, Associate Professor, Monash University; Leigh Walker, , Florey Institute of Neuroscience and Mental Health, and Roberta Anversa, , The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Does PRP Work For Hair Loss?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Ankit Gupta takes us through the details of this hair loss remedy for androgenic alopecia.
The bald truth
Platelet-Rich Plasma (PRP) is a controversial treatment for androgenic hair loss.
What it involves: blood is drawn and separated using a centrifuge. PRP—including growth proteins and hormones—is extracted from the blood; about 30 ml of blood is needed to produce 5 ml of PRP. This is then injected directly into the scalp. As this can be painful, local anaesthetic is sometimes used first. This usually involves monthly sessions for the first 3 months, then booster sessions every 3–6 months thereafter.
Does it work? Research is young; so far 60% of trials have found it worked; 40% found it didn’t. When it works, effectiveness (in terms of hair restoration) is considered to be between 25–43%. Results are inconsistent and seem to vary from person to person.
In short, this doctor’s recommendation is to consider it after already having tried standard treatments such as finasteride and/or minoxidil, as they are more likely to work and don’t involve such exciting procedures as injecting your own blood extracts back into your head.
For more on all of this, plus links to the 13 papers cited, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Hair-Loss Remedies, By Science
- Hair Growth: Caffeine and Minoxidil Strategies
- Gentler Hair Health Options
Take care!
Share This Post

Nature Valley Protein Granola vs Kellog’s All-Bran – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Nature Valley Protein Granola to Kellog’s All-Bran, we picked the All-Bran.
Why?
While the Protein Granola indeed contains more protein (13g/cup, compared to 5g/cup), it also contains three times as much sugar (18g/cup, compared to 9g/cup) and only ⅓ as much fiber (4g/cup, compared to 12g/cup)
Given that fiber is what helps our bodies to absorb sugar more gently (resulting in fewer spikes), this is extremely important, especially since 18g of sugar in one cup of Protein Granola is already most of the recommended daily allowance, all at once!
For reference: the AHA recommends no more than 25g added sugar for women, or 32g for men
Hence, we went for the option with 3x as much fiber and ⅓ of the sugar, the All-Bran.
For more about keeping blood sugars stable, see:
10 Ways To Balance Blood Sugars
Enjoy!
Share This Post
Related Posts

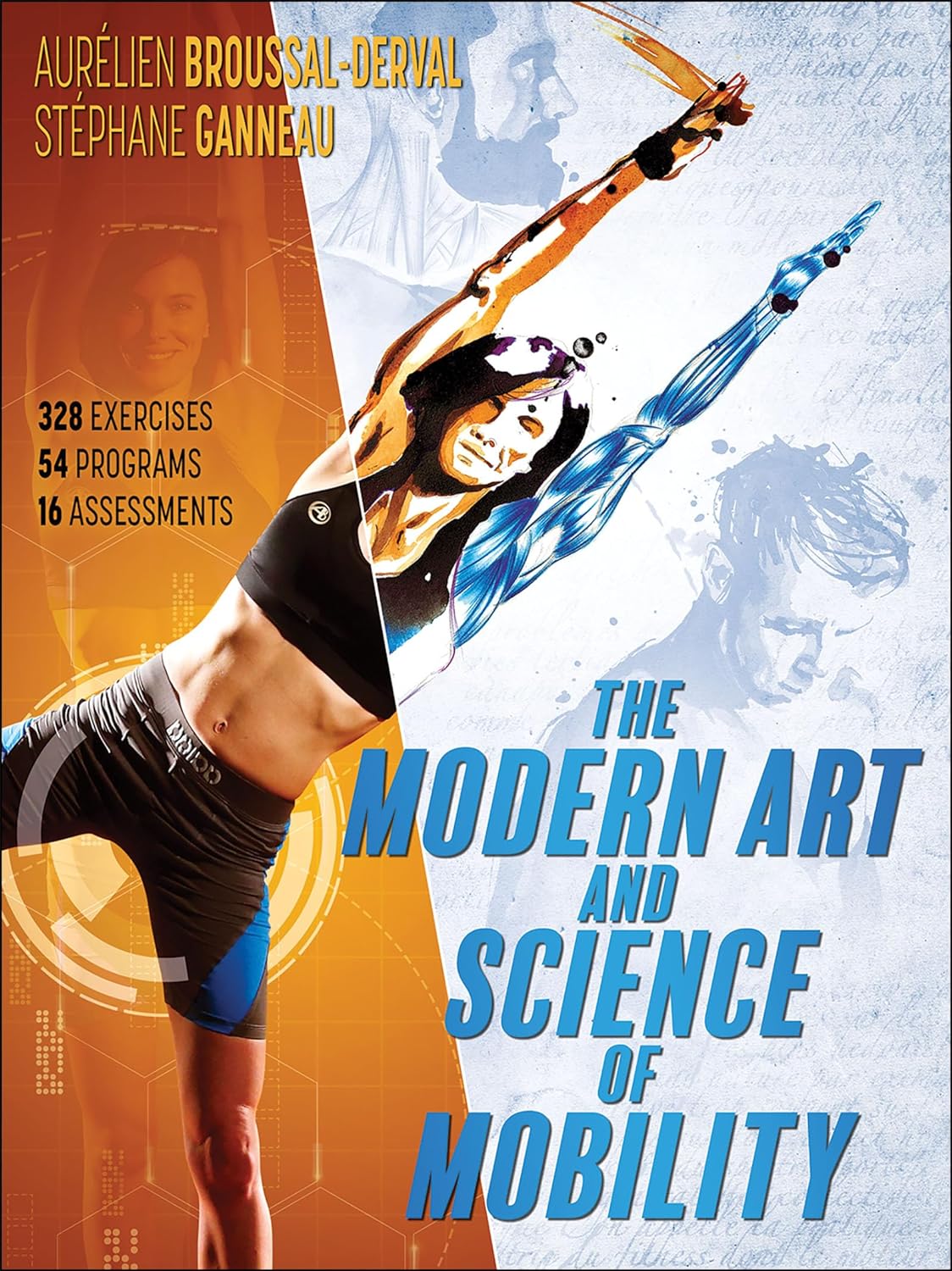
The Modern Art and Science of Mobility – by Aurélien Broussal-Derval
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed mobility books before, so what makes this one stand out?
We’ll be honest: the illustrations are lovely.
The science, the information, the exercises, the routines, the programs… All these things are excellent too, but these can be found in many a book.
What can’t usually be found is very beautiful (yet no less clear) watercolor paintings and charcoal sketches as anatomical illustrations.
There are photos too (also of high quality), but the artistry of the paintings and sketches is what makes the reader want to spend time perusing the books.
At least, that’s what this reviewer found! Because it’s all very well having access to a lot of information (and indeed, I read so much), but making it enjoyable increases the chances of rereading it much more often.
As for the rest of the content, the book’s information is divided in categories:
- Pain (what causes it, what it means, and how to manage it)
- Breathing (yes, a whole section devoted to this, and it is aligned heavily to posture also, as well as psychological state and the effect of stress on tension, inflammation, and more)
- Movement (this is mostly about kinds of movement and ranges of movement)
- Mobility (this is about aggregating movements as a fully mobile human)
So, each builds on from the previous because any pain needs addressing before anything else, breathing (and with it, posture) comes next, then we learn about movement, then we bring it all together for mobility.
Bottom line: this is a beautiful and comprehensive book that will make learning a joy
Click here to check out The Modern Art and Science of Mobility, and learn and thrive!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Turmeric (Curcumin) Dos and Don’ts With Dr. Kim
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Turmeric is a fabulous spice, most well-known for its anti-inflammatory powers; its antioxidant effects benefit all of the body, including the brain. While it fights seemingly everything from arthritis to atherosclerosis to Alzheimer’s and more, it also boosts brain-derived neurotrophic factor, looks after your cardiovascular health, holds back diabetes, reduces the risk of cancer, fights depression, slows aging, and basically does everything short of making you sing well too.
Dr. Leonid Kim goes over the scientific evidence for these, and also talks about some of the practicalities of taking turmeric, and safety considerations.
For the most part, turmeric is very safe even at high doses (up to 8g at least); indeed, at smaller doses (e.g. 500mg) it largely does the same job as non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, with fewer problems.
It also does the job of several antidiabetic medications, by increasing uptake of glucose (thus reducing blood sugar levels) while simultaneously decreasing the glucose secretion from the liver. It does this by regulating the AMPK signalling pathway, just like metformin—while again, being safer.
Dr. Kim also looks at the (good!) evidence for turmeric in managing PCOS and undoing NAFLD; so far, so good.
Dosage: he bids us pay attention whether we’re taking it as turmeric itself or as curcumin standardized extract. The latter is the active compound, and in principle more powerful, but in practice it can get metabolized too quickly and easily—before it can have its desired effect. So, turmeric itself is a very good choice.
Absorption: since we do want it to be absorbed well, though, he does recommend taking it with piperine (as in black pepper).
You may be thinking: isn’t this going to cause the same problem you were just talking about, and cause it to be metabolized too quickly? And the answer is: no! How piperine works is almost the opposite; it protects the curcumin in the turmeric from our digestive enzymes, and thus allows them to get absorbed without being broken down too quickly—thus increasing the bioavailability by slowing the process down.
Lipophilia: no, that’s not a disease (or a fetish), rather it means that curcumin is soluble in fats, so we should take it near in time to a meal that contains at least a tablespoon of oil in total (so if you’re cooking a curry with your turmeric, this need is covered already, for example).
Supplement provenance: he recommends picking a supplement that’s been tested by a reputable 3rd party, as otherwise turmeric can be quite prone to impurities (which can include lead and arsenic, so, not great).
Contraindications: for some people, curcumin can cause gastrointestinal issues (less likely if taking with meals), and also, it can interact with blood-thinners. While taking aspirin or curcumin alone might help avoid circulatory problems, taking both could increase the bleeding risk for some people, for example. Similarly, if taking curcumin and metformin while diabetic, one must watch out for the combination being too effective at lowering blood sugar levels, and thus causing hypoglycemia instead. Similar deal with blood pressure medications.
There’s more in the video though (yes really; we know we wrote a lot but it’s information-dense), so do check it out:
Click Here If The Embedded Video Doesn’t Load Automatically
Want to know more?
You can also check out our related articles:
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Black Pepper’s Impressive Anti-Cancer Arsenal (And More)Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Mental Health Courts Can Struggle to Fulfill Decades-Old Promise
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
GAINESVILLE, Ga. — In early December, Donald Brown stood nervously in the Hall County Courthouse, concerned he’d be sent back to jail.
The 55-year-old struggles with depression, addiction, and suicidal thoughts. He worried a judge would terminate him from a special diversion program meant to keep people with mental illness from being incarcerated. He was failing to keep up with the program’s onerous work and community service requirements.
“I’m kind of scared. I feel kind of defeated,” Brown said.
Last year, Brown threatened to take his life with a gun and his family called 911 seeking help, he said. The police arrived, and Brown was arrested and charged with a felony of firearm possession.
After months in jail, Brown was offered access to the Health Empowerment Linkage and Possibilities, or HELP, Court. If he pleaded guilty, he’d be connected to services and avoid prison time. But if he didn’t complete the program, he’d possibly face incarceration.
“It’s almost like coercion,” Brown said. “‘Here, sign these papers and get out of jail.’ I feel like I could have been dealt with a lot better.”
Advocates, attorneys, clinicians, and researchers said courts such as the one Brown is navigating can struggle to live up to their promise. The diversion programs, they said, are often expensive and resource-intensive, and serve fewer than 1% of the more than 2 million people who have a serious mental illness and are booked into U.S. jails each year.
People can feel pressured to take plea deals and enter the courts, seeing the programs as the only route to get care or avoid prison time. The courts are selective, due in part to political pressures on elected judges and prosecutors. Participants must often meet strict requirements that critics say aren’t treatment-focused, such as regular hearings and drug screenings.
And there is a lack of conclusive evidence on whether the courts help participants long-term. Some legal experts, like Lea Johnston, a professor of law at the University of Florida, worry the programs distract from more meaningful investments in mental health resources.
Jails and prisons are not the place for individuals with mental disorders, she said. “But I’m also not sure that mental health court is the solution.”
The country’s first mental health court was established in Broward County, Florida, in 1997, “as a way to promote recovery and mental health wellness and avoid criminalizing mental health problems.” The model was replicated with millions in funding from such federal agencies as the Substance Abuse and Mental Health Services Administration and the Department of Justice.
More than 650 adult and juvenile mental health courts were operational as of 2022, according to the National Treatment Court Resource Center. There’s no set way to run them. Generally, participants receive treatment plans and get linked to services. Judges and mental health clinicians oversee their progress.
Researchers from the center found little evidence that the courts improve participants’ mental health or keep them out of the criminal justice system. “Few studies … assess longer-term impacts” of the programs “beyond one year after program exit,” said a 2022 policy brief on mental health courts.
The courts work best when paired with investments in services such as clinical treatment, recovery programs, and housing and employment opportunities, said Kristen DeVall, the center’s co-director.
“If all of these other supports aren’t invested in, then it’s kind of a wash,” she said.
The courts should be seen as “one intervention in that larger system,” DeVall said, not “the only resource to serve folks with mental health needs” who get caught up in the criminal justice system.
Resource limitations can also increase the pressures to apply for mental health court programs, said Lisa M. Wayne, executive director of the National Association of Criminal Defense Lawyers. People seeking help might not feel they have alternatives.
“It’s not going to be people who can afford mental health intervention. It’s poor people, marginalized folks,” she said.
Other court skeptics wonder about the larger costs of the programs.
In a study of a mental health court in Pennsylvania, Johnston and a University of Florida colleague found participants were sentenced to longer time under government supervision than if they’d gone through the regular criminal justice system.
“The bigger problem is they’re taking attention away from more important solutions that we should be investing in, like community mental health care,” Johnston said.
When Melissa Vergara’s oldest son, Mychael Difrancisco, was arrested on felony gun charges in Queens in May 2021, she thought he would be an ideal candidate for the New York City borough’s mental health court because of his diagnosis of autism spectrum disorder and other behavioral health conditions.
She estimated she spent tens of thousands of dollars to prepare Difrancisco’s case for consideration. Meanwhile, her son sat in jail on Rikers Island, where she said he was assaulted multiple times and had to get half a finger amputated after it was caught in a cell door.
In the end, his case was denied diversion into mental health court. Difrancisco, 22, is serving a prison sentence that could be as long as four years and six months.
“There’s no real urgency to help people with mental health struggles,” Vergara said.
Critics worry such high bars to entry can lead the programs to exclude people who could benefit the most. Some courts don’t allow those accused of violent or sexual crimes to participate. Prosecutors and judges can face pressure from constituents that may lead them to block individuals accused of high-profile offenses.
And judges often aren’t trained to make decisions about participants’ care, said Raji Edayathumangalam, senior policy social worker with New York County Defender Services.
“It’s inappropriate,” she said. “We’re all licensed to practice in our different professions for a reason. I can’t show up to do a hernia operation just because I read about it or sat next to a hernia surgeon.”
Mental health courts can be overly focused on requirements such as drug testing, medication compliance, and completing workbook assignments, rather than progress toward recovery and clinical improvement, Edayathumangalam said.
Completing the programs can leave some participants with clean criminal records. But failing to meet a program’s requirements can trigger penalties — including incarceration.
During a recent hearing in the Clayton County Behavioral Health Accountability Court in suburban Atlanta, one woman left the courtroom in tears when Judge Shana Rooks Malone ordered her to report to jail for a seven-day stay for “being dishonest” about whether she was taking court-required medication.
It was her sixth infraction in the program — previous consequences included written assignments and “bench duty,” in which participants must sit and think about their participation in the program.
“I don’t like to incarcerate,” Malone said. “That particular participant has had some challenges. I’m rooting for her. But all the smaller penalties haven’t worked.”
Still, other participants praised Malone and her program. And, in general, some say such diversion programs provide a much-needed lifeline.
Michael Hobby, 32, of Gainesville was addicted to heroin and fentanyl when he was arrested for drug possession in August 2021. After entry into the HELP Court program, he got sober, started taking medication for anxiety and depression, and built a stable life.
“I didn’t know where to reach out for help,” he said. “I got put in handcuffs, and it saved my life.”
Even as Donald Brown awaited his fate, he said he had started taking medication to manage his depression and has stayed sober because of HELP Court.
“I’ve learned a new way of life. Instead of getting high, I’m learning to feel things now,” he said.
Brown avoided jail that early December day. A hearing to decide his fate could happen in the next few weeks. But even if he’s allowed to remain in the program, Brown said, he’s worried it’s only a matter of time before he falls out of compliance.
“To try to improve myself and get locked up for it is just a kick in the gut,” he said. “I tried really hard.”
KFF Health News senior correspondent Fred Clasen-Kelly contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: