The Recipe For Empowered Leadership – by Doug Meyer-Cuno
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is not a “here’s how to become a leader, you young would-be Machiavelli”; it’s more a “so you’re in a leadership role; now what?” book. The book’s subtitle describes well its contents: “25 Ingredients For Creating Value & Empowering Others”
The book is written with the voice of experience, but without the ego-driven padding that accompanies many such books. Especially: any anecdotal illustrations are short and to-the-point, no chapter-long diversions here.
Which we love!
Equally helpful is where the author does spend a little more time and energy: on the “down to brass tacks” of how exactly to do various things.
In short: if instead of a lofty-minded book of vague idealized notions selling a pipedream, you’d rather have a manual of how to actually be a good leader when it comes down to it, this is the book for you.
Pick Up The Recipe For Empowered Leadership On Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Planet of Viruses – by Carl Zimmer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed numerous books on the immune system before, and this one’s mostly not about that.
Instead, this one focuses on the viruses themselves, and the part they play in our world, for good and for ill. Popular awareness tends to focus on the ill, of course.
But, there’s a lot that viruses do for us too, including:
- Weak/harmless viruses that keep our immune systems on their toes and ready
- Bacteriophage viruses that kill and consume pathogens that, left unchecked, would do the same to us
- Endogenous retroviruses that have become symbiotic with the human organism, without which our species would quickly go extinct
He also talks about biological warfare, and how we cannot bury our heads in the sand by avoiding research on those grounds, because someone will always do it anyway, so (as the motto of the immune system itself might say), best to be prepared.
The author is a science journalist, by the way, and has no PhD, but does have a flock of Fellowships and assorted scientific awards and honors, so he appears to be doing good work so far as the scientific community is concerned.
Bottom line: if you’d like to know more about viruses than “they’re very small and can cause harm”, then this book will open a whole new world.
Click here to check out A Planet of Viruses, and upgrade your knowledge!
Share This Post
-
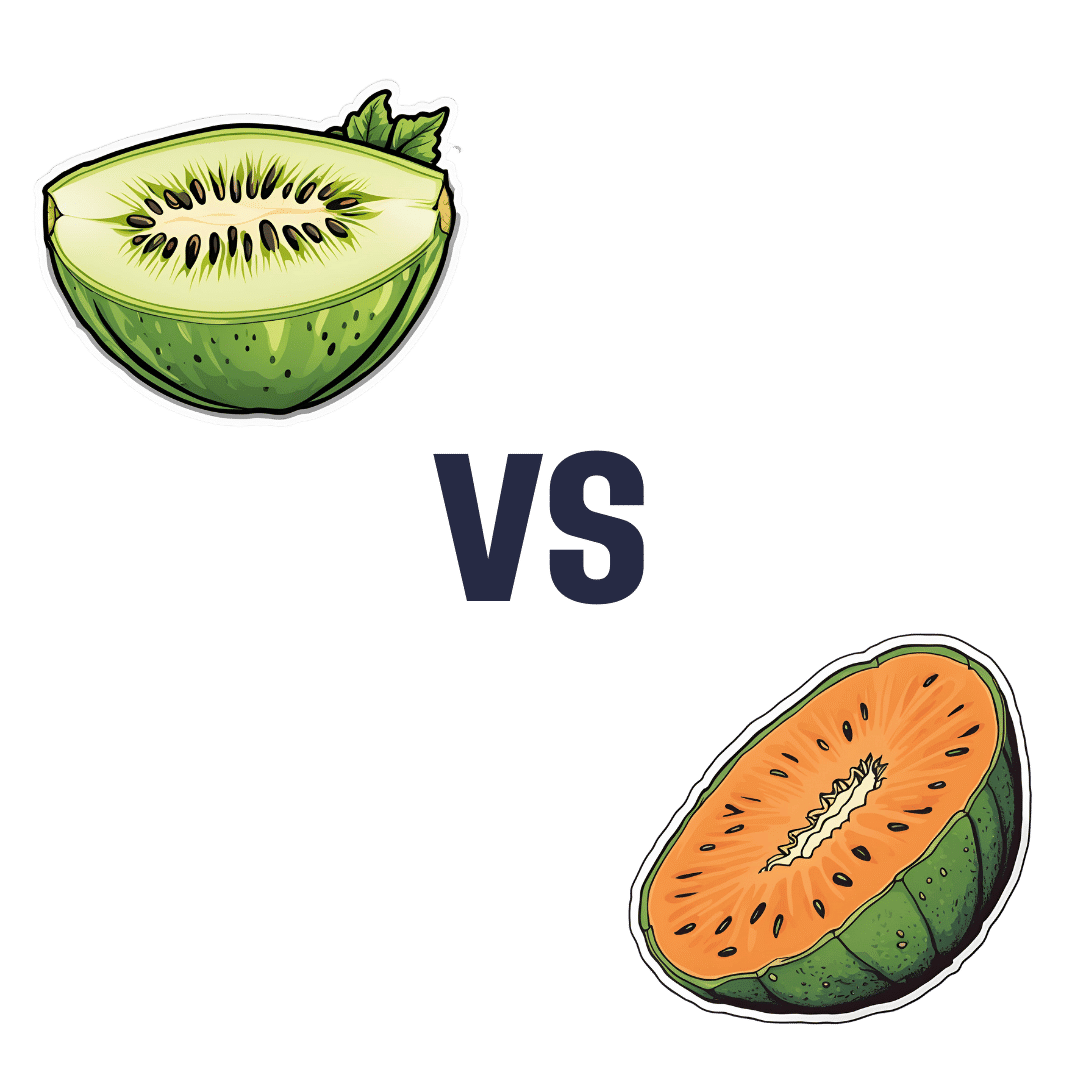
Honeydew vs Cantaloupe – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honeydew to cantaloupe, we picked the cantaloupe.
Why?
In terms of macros, there’s not a lot between them—they’re both mostly water. Nominally, honeydew has more carbs while cantaloupe has more fiber and protein, but the differences are very small. So, a very slight win for cantaloupe.
Looking at vitamins: honeydew has slightly more of vitamins B5 and B6 (so, the vitamins that are in pretty much everything), while cantaloupe has a more of vitamins A, B1, B2, B3, C, and E (especially notably 67x more vitamin A, whence its color). A more convincing win for cantaloupe.
The minerals category is even more polarized: honeydew has more selenium (and for what it’s worth, more sodium too, though that’s not usually a plus for most of us in the industrialized world), while cantaloupe has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An overwhelming win for cantaloupe.
No surprises: adding up the slight win for cantaloupe, the convincing win for cantaloupe, and the overwhelming win for cantaloupe, makes cantaloupe the overall best pick here.
Enjoy!
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
Lower Cholesterol Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Lower Cholesterol, Without Statins
We’ll start this off by saying that lowering cholesterol might not, in fact, be critical or even especially helpful for everyone, especially in the case of women. We covered this more in our article about statins:
…which was largely informed by the wealth of data in this book:
The Truth About Statins – by Dr. Barbara H. Roberts
…which in turn, may in fact put a lot of people off statins. We’re not here to tell you don’t use them—they may indeed be useful or even critical for some people, as Dr. Roberts herself also makes makes clear. But rather, we always recommend learning as much as possible about what’s going on, to be able to make the most informed choices when it comes to what often might be literally life-and-death decisions.
On which note, if anyone would like a quick refresher on cholesterol, what it actually is (in its various forms) and what it does, why we need it, the problems it can cause anyway, then here you go:
Now, with all that in mind, we’re going to assume that you, dear reader, would like to know:
- how to lower your LDL cholesterol, and/or
- how to maintain a safe LDL cholesterol level
Because, while the jury’s out on the dangers of high LDL levels for women in particular, it’s clear that for pretty much everyone, maintaining them within well-established safe zones won’t hurt.
Here’s how:
Relax
Or rather, manage your stress. This doesn’t just reduce your acute risk of a heart attack, it also improves your blood metrics along the way, and yes, that includes not just blood pressure and blood sugars, but even triglycerides! Here’s the science for that, complete with numbers:
What are the effects of psychological stress and physical work on blood lipid profiles?
With that in mind, here’s…
How To Manage Chronic Stress (Even While Chronically Stressed)
Not chemically “relaxed”, though
While relaxing is important, drinking alcohol and smoking are unequivocally bad for pretty much everything, and this includes cholesterol levels:
Can We Drink To Good Health? ← this also covers popular beliefs about red wine and heart health, and the answer is no, we cannot
As for smoking, it is good to quit as soon as possible, unless your doctor specifically advises you otherwise (there are occasional situations where something else needs to be dealt with first, but not as many some might like to believe):
Addiction Myths That Are Hard To Quit
If you’re wondering about cannabis (CBD and/or THC), then we’d love to tell you about the effect these things have on heart health in general and cholesterol levels in particular, but the science is far too young (mostly because of the historic, and in some places contemporary, illegality cramping the research), and we could only find small, dubious, mutually contradictory studies so far. So the honest answer is: science doesn’t know this one, yet.
Exercise… But don’t worry, you can still stay relaxed
When it comes to heart health, the most important thing is keeping moving, so getting in those famous 150 minutes per week of moderate exercise is critical, and getting more is ideal.
240 minutes per week is a neat 40 minutes per day, by the way and is very attainable (this writer lives a 20-minute walk away from where she does her daily grocery shopping, thus making for a daily 40-minute round trip, not counting the actual shopping).
See: The Doctor Who Wants Us To Exercise Less, And Move More
If walking is for some reason not practical for you, here’s a whole list of fun options that don’t feel like exercise but are:
Manage your hormones
This one is mostly for menopausal women, though some people with atypical hormonal situations may find it applicable too.
Estrogen protects the heart… Until it doesn’t:
See also: World Menopause Day: Menopause & Cardiovascular Disease Risk
Here’s a great introduction to sorting it out, if necessary:
Dr. Jen Gunter: What You Should Have Been Told About Menopause Beforehand
Eat a heart-healthy diet
Shocking nobody, but it has to be said, for the sake of being methodical. So, what does that look like?
What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
(it’s fiber in the #1 spot, but there’s a list of most important things there, that’s worth checking out and comparing it to what you habitually eat)
You can also check out the DASH (Dietary Approaches to Stop Hypertension) edition of the Mediterranean diet, here:
Four Ways To Upgrade The Mediterranean Diet
As for saturated fat (and especially trans-fats), the basic answer is to keep them to minimal, but there is room for nuance with saturated fats at least:
Can Saturated Fats Be Healthy?
And lastly, do make sure to get enough omega 3 fatty-acids:
What Omega-3s Really Do For Us
And enjoy plant sterols and stanols! This would need a whole list of their own, so here you go:
Take These To Lower Cholesterol! (Statin Alternatives)
Take care!
Share This Post
Related Posts
-
Parsnips vs Potatoes – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing parsnips to potatoes, we picked the parsnips.
Why?
To be more specific, we’re looking at russet potatoes, and in both cases we’re looking at cooked without fat or salt, skin on. In other words, the basic nutritional values of these plants in edible form, without adding anything. With this in mind, once we get to the root of things, there’s a clear winner:
Looking at the macros first, potatoes have more carbs while parsnips have more fiber. Potatoes do have more protein too, but given the small numbers involved when it comes to protein we don’t think this is enough of a plus to outweigh the extra fiber in the parsnips.
In the category of vitamins, again a champion emerges: parsnips have more of vitamins B1, B2, B5, B9, C, E, and K, while potatoes have more of vitamins B3, B6, and choline. So, a 7:3 win for parsnips.
When it comes to minerals, parsnips have more calcium copper, manganese, selenium, and zinc, while potatoes have more iron and potassium. Potatoes do also have more sodium, but for most people most of the time, this is not a plus, healthwise. Disregarding the sodium, this category sees a 5:2 win for parsnips.
In short: as with most starchy vegetables, enjoy both in moderation if you feel so inclined, but if you’re picking one, then parsnips are the nutritionally best choice here.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Should You Go Light Or Heavy On Carbs?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Are You, Really? And How Old Is Your Heart?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Are You, Really? The Free NHS Health Test
We took this surprisingly incisive 10-minute test from the UK’s famous National Health Service—the test is part of the “Better Health” programme, a free-to-all (yes, even those from/in other countries) initiative aimed at keeping people healthy enough to have less need of medical attention.
As one person who took the test wrote:
❝I didn’t expect that a government initiative would have me talking about how I need to keep myself going to be there for the people I love, let alone that a rapid-pace multiple-choice test would elicit these responses and give personalized replies in turn, but here we are❞
It goes beyond covering the usual bases, in that it also looks at what’s most important to you, and why, and what might keep you from doing the things you want/need to do for your health, AND how those obstacles can be overcome.
Pretty impressive for a 10-minute test!
Is Your Health Above Average Already? Take the Free 10-minute NHS test now!
How old are you, in your heart?
Poetic answers notwithstanding (this writer sometimes feels so old, and yet also much younger than she is), there’s a biological answer here, too.
Again free for the use of all*, here’s a heart age calculator.
*It is suitable for you if you are aged 30–95, and do not have a known complicating cardiovascular disease.
It will ask you your (UK) postcode; just leave that field blank if you’re not in the UK; it’ll be fine.
How Old Are You, In Your Heart? Take the Free 10-minute NHS test now!
(Neither test requires logging into anything, and they do not ask for your email address. The tests are right there on the page, and they give the answers right there on the page, immediately)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
12 Questions For Better Brain Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We usually preface our “Expert Insights” pieces with a nice banner that has a stylish tall cutout that allows us to put a photo of the expert in. Today we’re not doing that, because for today’s camera-shy expert, we could only find one photo, and it’s a small, grainy, square headshot that looks like it was taken some decades ago, and would not fit our template at all. You can see it here, though!
In any case, Dr. Linda Selwa is a neurologist and neurophysiologist with nearly 40 years of professional experience.
The right questions to ask
As a neurologist, she found that one of the problems that results in delayed interventions (and thus, lower efficacy of those interventions) is that people don’t know there’s anything to worry about until a degenerative brain condition has degenerated past a certain point. With that in mind, she bids us ask ourselves the following questions, and discuss them with our primary healthcare providers as appropriate:
- Sleep: Are you able to get sufficient sleep to feel rested?
- Affect, mood and mental health: Do you have concerns about your mood, anxiety, or stress?
- Food, diet and supplements: Do you have concerns about getting enough or healthy enough food, or have any questions about supplements or vitamins?
- Exercise: Do you find ways to fit physical exercise into your life?
- Supportive social interactions: Do you have regular contact with close friends or family, and do you have enough support from people?
- Trauma avoidance: Do you wear seatbelts and helmets, and use car seats for children?
- Blood pressure: Have you had problems with high blood pressure at home or at doctor visits, or do you have any concerns about blood pressure treatment or getting a blood pressure cuff at home?
- Risks, genetic and metabolic factors: Do you have trouble controlling blood sugar or cholesterol? Is there a neurological disease that runs in your family?
- Affordability and adherence: Do you have any trouble with the cost of your medicines?
- Infection: Are you up to date on vaccines, and do you have enough information about those vaccines?
- Negative exposures: Do you smoke, drink more than one to two drinks per day, or use non-prescription drugs? Do you drink well water, or live in an area with known air or water pollution?
- Social and structural determinants of health: Do you have concerns about keeping housing, having transportation, having access to care and medical insurance, or being physically or emotionally safe from harm?
You will note that some of these are well-known (to 10almonds readers, at least!) risk factors for cognitive decline, but others are more about systemic and/or environmental considerations, things that don’t directly pertain to brain health, but can have a big impact on it anyway.
About “concerns”: in the case of those questions that ask “do you have concerns about…?”, and you’re not sure, then yes, you do indeed have concerns.
About “trouble”: as for these kinds of health-related questionnaires in general, if a question asks you “do you have trouble with…?” and your answer is something like “no, because I have a special way of dealing with that problem” then the answer for the purposes of the questionnaire is yes, you do indeed have trouble.
Note that you can “have trouble with” something that you simultaneously “have under control”—just as a person can have no trouble at all with something that they leave very much out of control.
Further explanation on each of the questions
If you’re wondering what is meant by any of these, or what counts, or why the question is even being asked, then we recommend you check out Dr. Selwa et al’s recently-published paper, then all is explained in there, in surprisingly easy-to-read fashion:
Emerging Issues In Neurology: The Neurologist’s Role in Promoting Brain Health
If you scroll past the abstract, introduction, and disclaimers, then you’ll be straight into the tables of information about the above 12 factors.
Want to be even more proactive?
Check out:
How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: