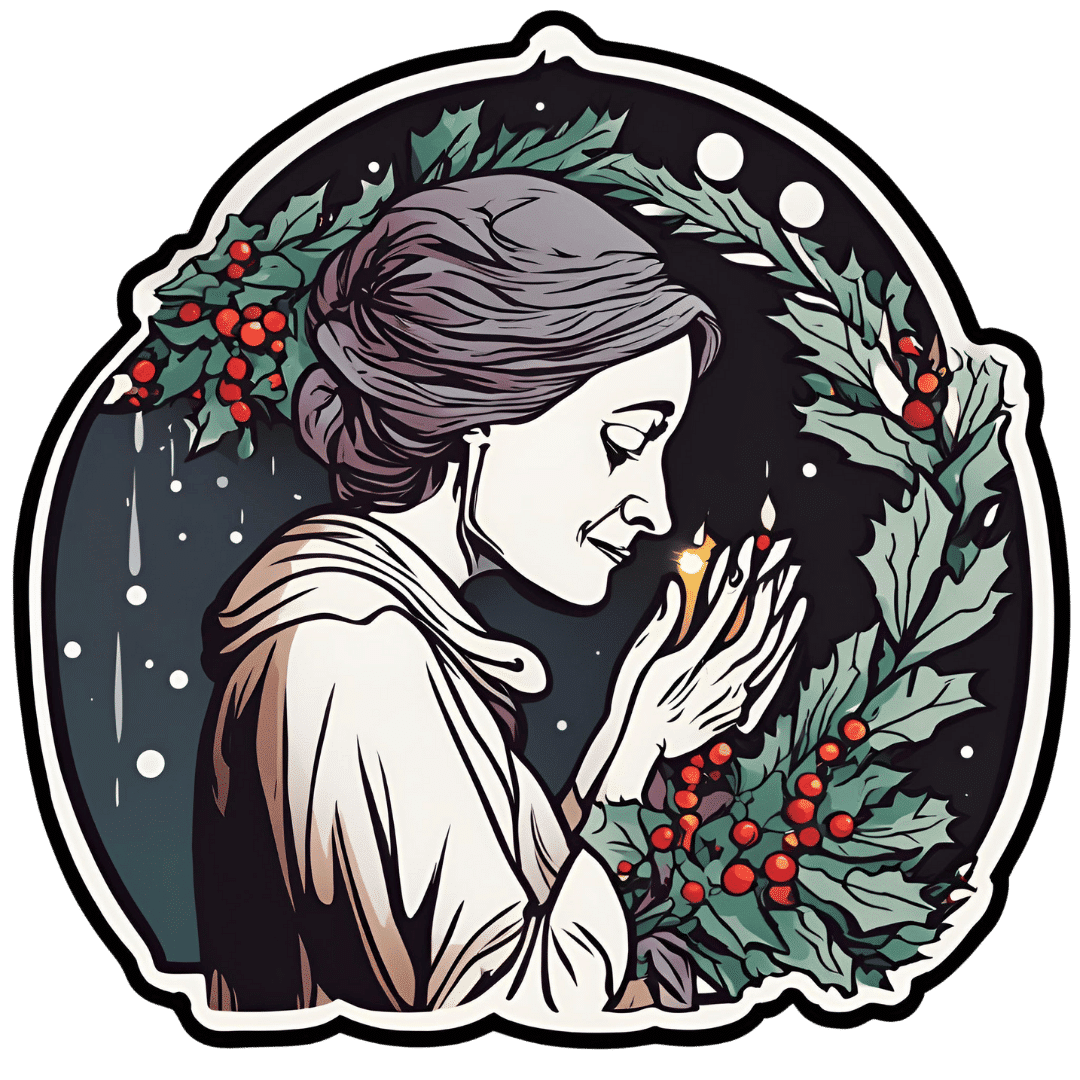
For many who are suffering with prolonged grief, the holidays can be a time to reflect and find meaning in loss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The holiday season is meant to be filled with joy, connection and celebration of rituals. Many people, however, are starkly reminded of their grief this time of year and of whom – or what – they have lost.
The added stress of the holiday season doesn’t help. Studies show that the holidays negatively affect many people’s mental health.
While COVID-19-related stressors may have lessened, the grief from change and loss that so many endured during the pandemic persists. This can cause difficult emotions to resurface when they are least expected.
I am a licensed therapist and trauma-sensitive yoga instructor. For the last 12 years, I’ve helped clients and families manage grief, depression, anxiety and complex trauma. This includes many health care workers and first responders who have recounted endless stories to me about how the pandemic increased burnout and affected their mental health and quality of life.
I developed an online program that research shows has improved their well-being. And I’ve observed firsthand how much grief and sadness can intensify during the holidays.
Post-pandemic holidays and prolonged grief
During the pandemic, family dynamics, close relationships and social connections were strained, mental health problems increased or worsened, and most people’s holiday traditions and routines were upended.
Those who lost a loved one during the pandemic may not have been able to practice rituals such as holding a memorial service, further delaying the grieving process. As a result, holiday traditions may feel more painful now for some. Time off from school or work can also trigger more intense feelings of grief and contribute to feelings of loneliness, isolation or depression.
Sometimes feelings of grief are so persistent and severe that they interfere with daily life. For the past several decades, researchers and clinicians have been grappling with how to clearly define and treat complicated grief that does not abate over time.
In March 2022, a new entry to describe complicated grief was added to the Diagnostic and Statistical Manual of Mental Disorders, or DSM, which classifies a spectrum of mental health disorders and problems to better understand people’s symptoms and experiences in order to treat them.
This newly defined condition is called prolonged grief disorder. About 10% of bereaved adults are at risk, and those rates appear to have increased in the aftermath of the pandemic.
People with prolonged grief disorder experience intense emotions, longing for the deceased, or troublesome preoccupation with memories of their loved one. Some also find it difficult to reengage socially and may feel emotionally numb. They commonly avoid reminders of their loved one and may experience a loss of identity and feel bleak about their future. These symptoms persist nearly every day for at least a month. Prolonged grief disorder can be diagnosed at least one year after a significant loss for adults and at least six months after a loss for children.
I am no stranger to complicated grief: A close friend of mine died by suicide when I was in college, and I was one of the last people he spoke to before he ended his life. This upended my sense of predictability and control in my life and left me untangling the many existential themes that suicide loss survivors often face.
How grieving alters brain chemistry
Research suggests that grief not only has negative consequences for a person’s physical health, but for brain chemistry too.
The feeling of grief and intense yearning may disrupt the neural reward systems in the brain. When bereaved individuals seek connection to their lost loved one, they are craving the chemical reward they felt before their loss when they connected with that person. These reward-seeking behaviors tend to operate on a feedback loop, functioning similar to substance addiction, and could be why some people get stuck in the despair of their grief.
One study showed an increased activation of the amygdala when showing death-related images to people who are dealing with complicated grief, compared to adults who are not grieving a loss. The amygdala, which initiates our fight or flight response for survival, is also associated with managing distress when separated from a loved one. These changes in the brain might explain the great impact prolonged grief has on someone’s life and their ability to function.
Recognizing prolonged grief disorder
Experts have developed scales to help measure symptoms of prolonged grief disorder. If you identify with some of these signs for at least one year, it may be time to reach out to a mental health professional.
Grief is not linear and doesn’t follow a timeline. It is a dynamic, evolving process that is different for everyone. There is no wrong way to grieve, so be compassionate to yourself and don’t make judgments on what you should or shouldn’t be doing.
Increasing your social supports and engaging in meaningful activities are important first steps. It is critical to address any preexisting or co-occurring mental health concerns such as anxiety, depression or post-traumatic stress.
It can be easy to confuse grief with depression, as some symptoms do overlap, but there are critical differences.
If you are experiencing symptoms of depression for longer than a few weeks and it is affecting your everyday life, work and relationships, it may be time to talk with your primary care doctor or therapist.
A sixth stage of grief
I have found that naming the stage of grief that someone is experiencing helps diminish the power it might have over them, allowing them to mourn their loss.
For decades, most clinicians and researchers have recognized five stages of grief: denial/shock, anger, depression, bargaining and acceptance.
But “accepting” your grief doesn’t sit well for many. That is why a sixth stage of grief, called “finding meaning,” adds another perspective. Honoring a loss by reflecting on its meaning and the weight of its impact can help people discover ways to move forward. Recognizing how one’s life and identity are different while making space for your grief during the holidays might be one way to soften the despair.
When my friend died by suicide, I found a deeper appreciation for what he brought into my life, soaking up the moments he would have enjoyed, in honor of him. After many years, I was able to find meaning by spreading mental health awareness. I spoke as an expert presenter for suicide prevention organizations, wrote about suicide loss and became certified to teach my local community how to respond to someone experiencing signs of mental health distress or crisis through Mental Health First Aid courses. Finding meaning is different for everyone, though.
Sometimes, adding a routine or holiday tradition can ease the pain and allow a new version of life, while still remembering your loved one. Take out that old recipe or visit your favorite restaurant you enjoyed together. You can choose to stay open to what life has to offer, while grieving and honoring your loss. This may offer new meaning to what – and who – is around you.
If you need emotional support or are in a mental health crisis, dial 988 or chat online with a crisis counselor.
Mandy Doria, Assistant Professor of Psychiatry, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Oxygen Advantage – by Patrick McKeown
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably know to breathe through your nose, and use your diaphragm. What else does this book have to offer?
A lot of the book is aimed at fixing specific problems, and optimizing what can be optimized—including with tips and tricks you may not have encountered before. Yet, the offerings are not bizarre either; we don’t need to learn to breathe through our ears while drinking a glass of water upside down or anything.
Rather, such simple things as improving one’s VO₂Max by occasionally holding one’s breath while walking briskly. But, he advises specifically, this should be done by pausing the breath halfway through the exhalation (a discussion of the ensuing physiological response is forthcoming).
Little things like that are woven throughout the book, whose style is mostly anecdotal rather than hard science, yet is consistent with broad scientific consensus in any case.
Bottom line: if you’ve any reason to think your breathing might be anything less than the best it could possibly be, this book is likely to help you to tweak it to be a little better.
Click here to check out The Oxygen Advantage, and get yours!
Share This Post
-
The Only Exercise You Need To Strengthen Every Hip Muscle (Ages 50+)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One exercise, no equipment, and easy to do without even getting changed:
You may be on the fence about this one
Standing on one leg is great, of course, and then…
Basic exercise:
- Imagine stepping over an electric fence side to side.
- Lift each leg high but slowly to engage hip muscles.
- Adjust the height and speed based on ease/difficulty.
Variations:
- Step over an imaginary side fence.
- Step over an imaginary front fence.
- Step sideways in the opposite direction.
- Step backward to complete a square.
- Ensure both legs are worked evenly.
As a bonus, it also improves balance!
For more on all this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
How Tight Are Your Hips? Test (And Fix!) With This
Take care!
Share This Post
-
Butter vs Plant Oils: What The Latest Evidence Shows
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve done some relevant head-to-head comparisons before in our “This or That” section:
- Avocado Oil vs Olive Oil – Which is Healthier?
- Olive Oil vs Coconut Oil – Which is Healthier?
- Sesame Oil vs Almond Oil – Which is Healthier?
- Sunflower Oil vs Canola Oil – Which is Healthier?
- Margarine vs Butter – Which is Healthier
- Butter vs Ghee – Which is Healthier?
We also did a deeper-dive into butter vs margarine:
Butter vs Margarine – Mythbusting Edition ← this one clears up a lot of misinformation about both butter and margarine
As well as: Saturated Fats: What’s The Truth? Can Saturated Fats Be Healthy?
So, we’re not coming into this one today unawares, and/but it’s an interesting comparison we haven’t directly written about before: butter vs plant oils in general
The Study
It was a JAMA Internal Medicine cohort study, which followed 221,054 adults (average age 56 at the start of the study, with a standard deviation of 7 years from that age) for up to 33 years.
Why “up to”? Because not everybody survived the study.
Specifically, 50,932 deaths were recorded, including 12,241 from cancer and 11,240 from cardiovascular disease (CVD).
Participants were categorized into quartiles based on butter or plant-based oil intake, and…
- The highest quartile (i.e. the 25% of people who consumed the most) butter intake linked to a 15% higher total mortality.
- The highest quartile (i.e. the 25% of people who consumed the most) plant-based oil intake linked to a 16% lower total mortality.
But, if those are the opposite ends of the spectrum, what about smaller differences?
Every 10g/day increase in consumption of plant-based oils yielded…
- 11% lower cancer mortality.
- 6% lower CVD mortality.
Meanwhile, 10g/day increase in butter consumption yielded…
- 12% higher cancer mortality.
- 17% higher CVD mortality.
These benefits must have a cap (after all, one cannot just drink liters of olive oil per day for for a 3400% decrease in mortality), but that cap was not ascertained, because there was no group drinking liters of plant oils per day, not even for science.
However, in the realm of small changes, substituting even 10g/intake of total butter with an equivalent amount of plant-based oils yielded 17% lower total mortality.
You can read the study in full, here: Butter and Plant-Based Oils Intake and Mortality
“So, what about the surely great difference between seed oils and olive oil?”
Compared the the vast gaping statistical chasm that lay between the results of butter and the results of plant oils, which plant oil one chooses doesn’t make a huge difference, iff one isn’t consuming a large amount—the important thing was skipping butter in favor of a plant oil of some kind.
Note also that, for example, deep-frying a starchy food like potatoes will cause the resultant fries (or such), even if not visibly oily, to now have about 10–15% of their original weight in water, replaced with oil. So, 100g (about 3oz) of fries may have around 10-15g oil. Obviously, this does depend on the cut and other factors, but that’s a ballpark figure.
Here’s a lengthier discussion about seed oils than we have room for today:
If you’re worried about inflammation, stop stressing about seed oils and focus on the basics ← in other words, yes it counts, but there are other things that count a lot more, such that if you’re paying attention to the other things, the fact that you sprayed your wok with a little canola oil before stir-frying those vegetables isn’t going to make a meaningful difference.
An as for olive oil? It’s a famously healthy oil, and certainly a candidate for the top spot along with avocado oil*:
All About Olive Oil ← we talk lipids, polyphenols, virginity, and more!
*…and it’s worth noting that these two oils’ (excellent) lipids profiles are very similar, meaning that the main factor between them is that olive oil usually retains vitamins that avocado oil doesn’t.
Take care!
Share This Post
Related Posts
-
The End of Alzheimer’s – by Dr. Dale Bredesen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one didn’t use the “The New Science Of…” subtitle that many books do, and this one actually is a “new science of”!
Which is exciting, and/but comes with the caveat that the overall protocol itself is still undergoing testing, but the results so far are promising. The constituent parts of the protocol are for the most already well-established, but have not previously been put together in this way.
Dr. Bredesen argues that Alzheimer’s Disease is not one condition but three (medical consensus agrees at least that it is a collection of conditions, but different schools of thought slice them differently), and outlines 36 metabolic factors that are implicated, and the good news is, most of them are within our control.
Since there’s a lot to put together, he also offers many workarounds and “crutches”, making for very practical advice.
The style of the book is on the hard end of pop-science, that is to say while the feel and tone is very pop-sciencey, there are nevertheless a lot of words that you might know but your spellchecker probably wouldn’t. He does explain everything along the way, but this does mean that if you’re not already well-versed, you can’t just dip in to a later point without reading the earlier parts.
Bottom line: even if you only implement half the advice in this book, you’ll be doing your long-term cognitive health a huge favor.
Click here to check out The End of Alzheimer’s, and keep cognitive decline at bay!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dyslexia Test
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
(and it’s mostly not about reading/writing!)
More than just shuffled letters
This video provides a self-test based on the Bangor Dyslexia Test (BDT). The BDT is 94% accurate in identifying dyslexia, and it includes 9 parts, with a mix of questions and tasks. Answering “yes” or struggling with tasks indicates possible dyslexia. Collecting 4+ indicators suggests dyslexia, but of course is not a replacement for official diagnosis.
It’s best to watch the video if you can, but here’s what to expect:
- Left-Right confusion: point your left hand to your right/left shoulder.
- Family history: any family members with dyslexia or struggles with reading/writing?
- Repeating numbers (order): repeat a given sequence of numbers in order.
- Letter confusion (e.g. b/d): do you confuse letters like “b” and “d” beyond age 8?
- Times tables: recite the 6, 7, and 8 times tables.
- Word manipulation: replace the letters in a word to create a new word, e.g. change “slide” (s ⇾ g) to “glide.”
- Repeating numbers (reversed): repeat a given sequence of numbers in reverse order.
- Months in reverse: recite the months of the year in reverse order.
- Subtraction: do you struggle with subtraction, e.g. 44-9 or 55-12?
Writer’s anecdote: I am not dyslexic, and/but I have an impressive level of dyscalculia (the purely numerical equivalent), to the point I’ll sometimes use a calculator to do single-digit calculations, and I am so bad at calculating ages or other differences between dates (I will have to count on my fingers or else run the severe risk of out-by-one errors). I have also been known to make mistakes counting down from 10, which really ruins dramatic tension.
In contrast, the left-right thing is interesting, because when I was first learning Arabic, I had no trouble reading/writing right-to-left, but I initially struggled so much to remember which way the “backspace” key would take me (in Arabic the backspace key backspaces to the right, despite still pointing to the left).
Anyway, for the test itself, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Reading, Better (Reading As A Cognitive Exercise)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
5 Ways To Beat Afternoon Energy Slumps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Nisha Vora, of Rainbow Plant Life fame. After graduating from Harvard Law School, she realized she hated being a lawyer, and pivoted completely to become what she now is 12 years later, a chef and health coach.
Here are her tips for boosting energy through the day:
Caffeine timing
If you don’t do caffeine at all, no need to change that, but if you do, Vora advises that midday is the best time for it, with a very good rationale:
- of course it should not be too late in the day, because the elimination half-life of caffeine (4–8 hours to eliminate just half of the caffeine, depending on genes, call it 6 hours as an average though honestly for most people it will either be 4 or 8, not 6) is such that it can easily interfere with sleep for most people
- because caffeine is an adenosine blocker, not an adenosine inhibitor, taking caffeine in the morning means either there’s no adenosine to block, or it’ll just “save” that adenosine for later, i.e. when the caffeine is eliminated, then the adenosine will kick in, meaning that your morning sleepiness has now been deferred to the afternoon, rather than eliminated.
Another reminder that caffeine is the “payday loan” of energy. So, midday it is. No morning sleepiness to defer, and yet also not so late as to interfere with sleep.
See also: Calculate (And Enjoy) The Perfect Night’s Sleep
Simplify what can be simplified
This one’s not from a physiological basis, but rather, that a lot of the time most of us have much of our energy being taken by constant task-switching (what gets called multitasking, but as our brain is a single processor, it really means switching rapidly between different kinds of cognition, which is not efficient). In order to avoid that energy drain, try to streamline things and make a particular effort to not only single-task, but to do so without distractions.
Counterpoint: if you have unmedicated ADHD, then chances are you’ll do better with a single small distraction chosen by you, than trying to go without distractions, because your brain will find distractions anyway, so you might as well choose one (for many people it is background music, or a podcast or TV show that one doesn’t may attention to but it’s there) as a matter of harm reduction, and that way you’ll do better at focusing on your primary task than if your brain were reaching out for every and any possible distraction.
Manage your blood sugars
In particular, she advocates for avoiding sugary breakfasts, opting instead for protein, fat, and fiber-rich options. For more in this regard, see:
10 Ways To Balance Your Blood Sugars
Walk after meals
You don’t have to don hiking boots and “I am just going outside and may be some time“; rather, even a 2–5 minute walk after a meal helps regulate digestion and glucose levels, avoiding postprandial energy slumps.
So,
- if you have a treadmill, after eating is a great time to use it for a few minutes
- if you have stairs, now’s a great time to go up and down them a few times
One last technique for when everything else fails
We’ll quote her directly on this one:
❝Despite my best efforts, soemtimes I just have one of those days. Maybe I didn’t sleep well or I’m distracted by my never ending thoughts. If I need to be productive or energized on those days, I will do something that I absolutely hate:
I will take a cold shower.
And I hate it because I’m already always cold all the time, so why would I want to get a cold shower?
Well, it’s because cold water immersion has been shown to dramatically boost your dopamine levels, which gives you more energy and motivation.
In the moment though, it’s mostly painful and I hate everything and everyone around me.
But I know that if I can suffer through two minutes of a cold shower, I will feel so refreshed.❞
There are more benefits than just that, though, see:
A Cold Shower A Day Keeps The Doctor Away?
Want more from Nisha Vora?
We reviewed one of her books a while back:
The Vegan Instant Pot Cookbook – by Nisha Vora
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: