6 Daily Habits To Keep Your Brain Young & Sharp
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Without brain health, we do not have health. So here are six ways to keep it in order:
Food for thought
The six areas to focus on are as follows:
- Physical exercise: as we at 10almonds sometimes say, what’s good for the heart is good for the brain (because the brain is only as healthy as the circulation feeding it). For this reason, the recommendation here is for physical exercise that improves heart health—so, walking, running, swimming, dancing, etc.
- Healthy diet: shocking nobody, this is important too. Specifically, a diet rich in fruits, vegetables, and healthy proteins and fats is important—partly for the heart benefits that give indirect benefits to the brain, and partly because the brain is built of stuff and so we have to consume that stuff in order to rebuild it (omega-3s features strongly here, for instance). Remember to hydrate, too! The body can’t do anything without water.
- Good sleep: yes, the famous 7–9 hours sleep per night, and yes, even at your age, whatever that might be. This is important for memory consolidation, cell repair, toxin removal, and more. Sleep deprivation, on the other hand, leads to cognitive decline and brain shrinkage.
- Mental stimulation: ideally, engaging those parts of the brain you most wish to protect (e.g. language, memory, or whatever is most important to you).
- Social interaction: this one gets underestimated a lot, but it’s important to have meaningful conversations (not just polite smalltalk from a small menu of stock phrases), and that these should be two-way, i.e. involving both listening/reading and speaking/writing. Ideally, all four of those, which for most people means online and offline social interactions.
- Stress management: because chronic stress damages brain cells and accelerates cognitive decline, it’s important to manage that; practices like mindfulness meditation go a very long way and make a big difference.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Physical Exercises That Build Your Brain ← this is different from just exercising for one’s heart and thus the brain by extension, and rather, is specific exercises that strengthen specific parts of the brain.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What’s Missing from Medicine – by Dr. Saray Stancic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Another from the ranks of “doctors who got a serious illness and it completely changed how they view the treatment of serious illness”, Dr. Stancic was diagnosed with multiple sclerosis, and wasn’t impressed with the treatments presented.
Taking an evidence-based lifestyle medicine approach, she was able to not only manage her illness sufficiently to resume her normal activities, but even when so far as to run a marathon, and today boasts a symptom-free, active life.
The subtitular six lifestyle changes are not too shocking, and include a plants-centric diet, good exercise, good sleep, stress management, avoidance of substance abuses, and a fostering of social connections, but the value here is in what she has to say about each, especially the ones that aren’t so self-explanatory and/or can even cause harm if done incorrectly (such as exercise, for example).
The style is on the academic end of pop-science, of the kind that has frequent data tables, lots of statistics, and an extensive bibliography, but is still very readable.
Bottom line: if you are faced with a chronic disease, or even just an increased risk of some chronic disease, or simply like to not take chances, then this is a high-value book for you.
Click here to check out What’s Missing From Medicine, and enjoy chronic good health!
Share This Post
-
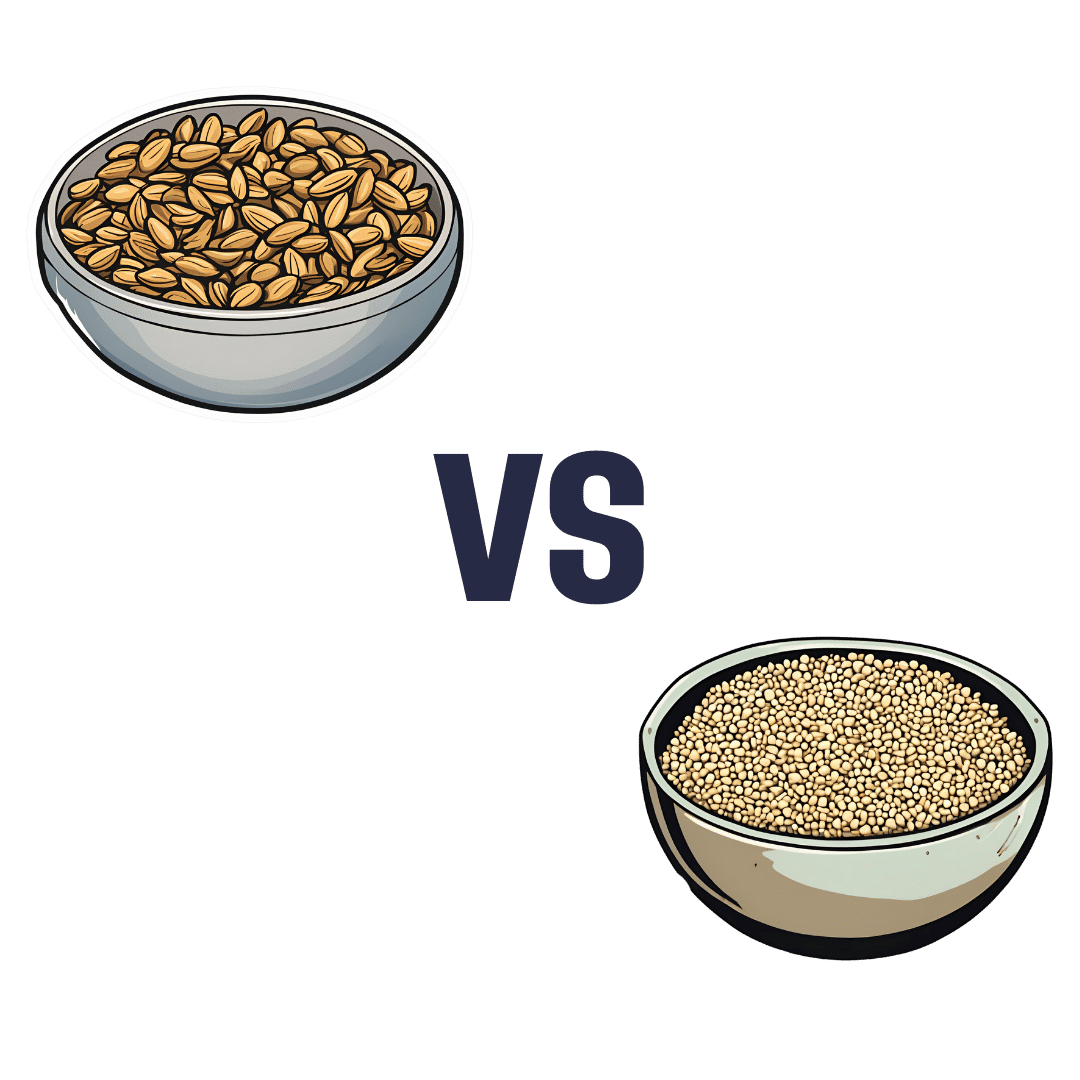
Sunflower Seeds vs Sesame Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower seeds to sesame seeds, we picked the sunflower.
Why?
In moderation, both are very healthy. We say “in moderation” because they’re both about 50% fat and such fats, while vital for life, are generally best enjoyed in small portions. Of that fat, sunflower has the slightly better fat profile; they’re both mostly poly- and monounsaturated fats, but sunflower has 10% saturated fat while sesame has 15%. Aside from fats, sunflower has slightly more protein and sesame has slightly more carbs. While sesame has slightly more fiber, because of the carb profile sunflower still has the lower glycemic index. All in all, a moderate win for sunflower in the macros category.
You may be wondering, with all that discussion of fats, what they’re like for omega-3, and sesame seeds have more omega-3, though sunflower seeds contain it too. Still, a point in sesame’s favor here.
When it comes to vitamins, sunflower has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, and choline, while sesame is not higher in any vitamins.
In the category of minerals, sunflower has more phosphorus, potassium, and selenium, while sesame has more calcium, copper, iron, and zinc. This is nominally a marginal win for sesame, but it should be noted that sunflower is still very rich in copper, iron, and zinc too (but not calcium).
Adding up the categories makes for a moderate win for sunflower seeds, but as ever, enjoy both; diversity is best!
Want to learn more?
You might like to read:
Sunflower Seeds vs Pumpkin Seeds – Which is Healthier?
Take care!
Share This Post
-
Mindsight – by Dr. Daniel Siegel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of books these days bear the subtitle “The New Science Of…”, but usually it’s not new, and often it’s not even science. So how does this one measure up?
- Is it new? The core ideas are mostly very old, but some of the interventions are new in presentation—and backed by relatively recent research—so we can give him this one on a technicality at least
- It is science? Yes! The author is a clinician (a psychatric clinician, specifically) and there’s nothing here that doesn’t have its foundations in robust science.
So, what’s this “mindsight”, then? Dr. Siegel wants to express to us a concept “for which no word currently exists”, so he had to make one up, to convey the idea of having a conscious awareness of what is going on in our brain, on an experiential basis. In other words: “mindfulness”. There was totally already a word for this, which he goes on to lampshade not very far into the book.
Nevertheless, we’ll forgive him a little copywriting swizzle with the title, because the content here is genuinely top-tier.
In the book, many ideas from many other pop-psychology books are covered, in useful, practical, no-nonsense fashion, laying out tools and interventions to strengthen various parts of our brain and our relationship with same.
Bottom line: this is the most comprehensive, science-centric, book on mindfulness that this reviewer has read.
Share This Post
Related Posts
-
5 Ways to Beat Menopausal Weight Gain!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As it turns out, “common” does not mean “inevitable”!
Health Coach Kait’s advice
Her 5 tips are…
- Understand your metabolism: otherwise you’re working the dark and will get random results. Learn about how different foods affect your metabolism, and note that hormonal changes due to menopause can mean that some food types have different effects now.
- Eat enough protein: one thing doesn’t change—protein helps with satiety, thus helping to avoid overeating.
- Focus on sleep: prioritizing sleep is essential for hormone regulation, and that means not just sex hormones, but also food-related hormones such as insulin, ghrelin, and leptin.
- Be smart about carbs: taking a lot of carbs at once can lead to insulin spikes and thus metabolic disorder, which in turn leads to fat in places you don’t want it (especially your liver and belly). Enjoying a low-carb diet, and/or pairing your carbs with proteins and fats, does a lot to help avoid insulin spikes too. Not mentioned in the video, but we’re going to mention here: don’t underestimate fiber’s role either, especially if you take it before the carbs, which is best for blood sugars, as it gives a buffer to the digestive process, thus slowing down absorption of carbs.
- Build muscle: if trying to avoid/lose fat, it’s tempting to focus on cardio, but we generally can’t exercise our way out of having fat, whereas having more muscle increases the body’s metabolic base rate, burning fat just by existing. So for this reason, enjoy muscle-building resistance exercises at least a few times per week.
For more information on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat & How To Lose It
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tuna Steak with Protein Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Yes, it’s protein on protein today, and it’s all healthy.
You will need (per person)
- 1 tuna steak
- 1 400g/12oz can mixed beans, drained & rinsed
- 1 tsp capers
- 2 tsp black pepper, coarse ground
- 1 red chili, chopped
- 1 lime, cut into wedges
- ½ tsp white wine vinegar
- Extra virgin olive oil, for cooking
- Garnish: chopped parsley
Method
(we suggest you read everything at least once before doing anything)
1) Put the beans in a bowl, mixing in the capers, vinegar, and 1 tsp of the black pepper
2) Gently rub a little olive oil onto each side of the tuna steak, and season with the remainder of the black pepper (as in, the other tsp, not the rest of what you have in the house).
3) Heat a ridged grill pan until hot, and then cook the tuna for around 3 minutes on each side. Do not jiggle it! Do not slide it, and definitely do not stir it. Just gently turn it over when necessary. The edges should be cooked, and the inside should still be pink (it’s easy to forget when it comes from a can, but remember tuna is usually eaten raw)
4) Serve, sprinkling with the chopped chili and garnishing with the parsley. The lime wedges go on the side for squeezing at the table.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Protein: How Much Do We Need, Really?
- Salmon vs Tuna – Which is Healthier?
- Cilantro vs Parsley – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’m So Effing Tired – by Dr. Amy Shah
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy sometimes to feel like we know more or less what we should be doing… If only we had the energy to get going!
- We know we want a better diet… But we don’t have the time/energy to cook so will go for the quickest option even when it’s not the best?
- We know we should exercise… But feel we just need to crash out on the couch for a bit first?
- We would dearly love to get better sleep… But our responsibilities aren’t facilitating that?
…and so on. Happily, Dr. Amy Shah is here with ways to cut through the Gordian Knot that is this otherwise self-perpetuating cycle of exhaustion.
Most of the book is based around tackling what Dr. Shah calls “the energy trifecta“:
- Hormone levels
- Immune system
- Gut health
You’ll note (perhaps with relief) that none of these things require an initial investment of energy that you don’t have… She’s not asking you to hit the gym at 5am, or magically bludgeon your sleep schedule into its proper place, say.
Instead, what she gives is practical, actionable, easy changes that don’t require much effort, to gently slide us back into the fast lane of actually having energy to do stuff!
In short: if you’ve ever felt like you’d like to implement a lot of very common “best practice” lifestyle advice, but just haven’t had the energy to get going, there’s more value in this handbook than in a thousand motivational pep talks.
Click here to check out “I’m So Effing Tired” and get on a better track of life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: