5 Exercises That Fix 95% Of Your Problems
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Well, your musculoskeletal problems, anyway! The exercises won’t, for example, do your taxes or deal with your loud neighbor for you. But, they will help your body be strong, supple, and pain-free:
20 minutes total
The exercises & what they do:
- Dead hang: improves shoulder health, decompresses the spine, and strengthens grip. Hang from a bar for 20–30 seconds, progressing to 1–2 minutes.
- Glute bridge: builds glute strength, improves core stability, and reduces lower back tension. Perform 2 sets of 10–15 reps, with variations like single-leg bridges or added weight.
- Farmer’s walk: a full-body workout that strengthens the shoulders, core, and grip while improving posture. Walk with weights for 30–60 seconds, 3 rounds, increasing weight or duration over time.
- Resting squat: enhances ankle, hip, and knee mobility, restoring natural functionality. Hold a deep squat for 20–30 seconds, progressing to 1–2 minutes. Use support for balance if necessary.
- Thread the needle: improves flexibility, reduces tension, and enhances rotational mobility. Perform slow, controlled rotations from an all-fours position, 2 sets of 10 reps per side.
Suggested 20-minute workout plan:
- Dead hang: 3 sets of 30 seconds
- Glute bridge: 2 sets of 10–15 reps
- Farmer’s walk: 30–60 seconds, 3 rounds
- Resting squat: hold for 20–30 seconds, 2–3 rounds
- Thread the needle: 2 sets of 10 reps per side
It is recommended to perform this routine 3 times per week with 1-minute rests between sets.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Life Extension Multivitamins vs Centrum Multivitamins – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Life Extension Multivitamins to Centrum Multivitamins, we picked the Life Extension.
Why?
The clue here was on the label: “two per day”. It’s not so that they can sell extra filler! It’s because they couldn’t fit it all into one.
While the Centrum Multivitamins is a (respectably) run-of-the-mill multivitamin (and multimineral) containing reasonable quantities of most vitamins and minerals that people supplement, the Life Extension product has the same plus more:
- More of the vitamins and minerals; i.e. more of them are hitting 100%+ of the RDA
- More beneficial supplements, including:
- Inositol, Alpha lipoic acid, Bio-Quercetin phytosome, phosphatidylcholine complex, Marigold extract, Apigenin, Lycopene, and more that we won’t list here because it starts to get complicated if we do.
We’ll have to write some main features on some of those that we haven’t written about before, but suffice it to say, they’re all good things.
Main take-away for today: sometimes more is better; it just necessitates then reading the label to check.
Want to get some Life Extension Multivitamins (and/or perhaps just read the label on the back)? Here they are on Amazon
PS: it bears mentioning, since we are sometimes running brands against each other head-to-head in this section: nothing you see here is an advertisement/sponsor unless it’s clearly marked as such. We haven’t, for example, been paid by Life Extension or any agent of theirs, to write the above. It’s just our own research and conclusion.
Share This Post
-
I’m feeling run down. Why am I more likely to get sick? And how can I boost my immune system?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It has been a long winter, filled with many viruses and cost-of-living pressures, on top of the usual mix of work, study, life admin and caring responsibilities.
Stress is an inevitable part of life. In short bursts, our stress response has evolved as a survival mechanism to help us be more alert in fight or flight situations.
But when stress is chronic, it weakens the immune system and makes us more vulnerable to illnesses such as the common cold, flu and COVID.
Pexels/Ketut Subiyanto Stress makes it harder to fight off viruses
When the immune system starts to break down, a virus that would normally have been under control starts to flourish.
Once you begin to feel sick, the stress response rises, making it harder for the immune system to fight off the disease. You may be sick more often and for longer periods of time, without enough immune cells primed and ready to fight.
In the 1990s, American psychology professor Sheldon Cohen and his colleagues conducted a number of studies where healthy people were exposed to an upper respiratory infection, through drops of virus placed directly into their nose.
These participants were then quarantined in a hotel and monitored closely to determine who became ill.
One of the most important factors predicting who got sick was prolonged psychological stress.
Cortisol suppresses immunity
“Short-term stress” is stress that lasts for a period of minutes to hours, while “chronic stress” persists for several hours per day for weeks or months.
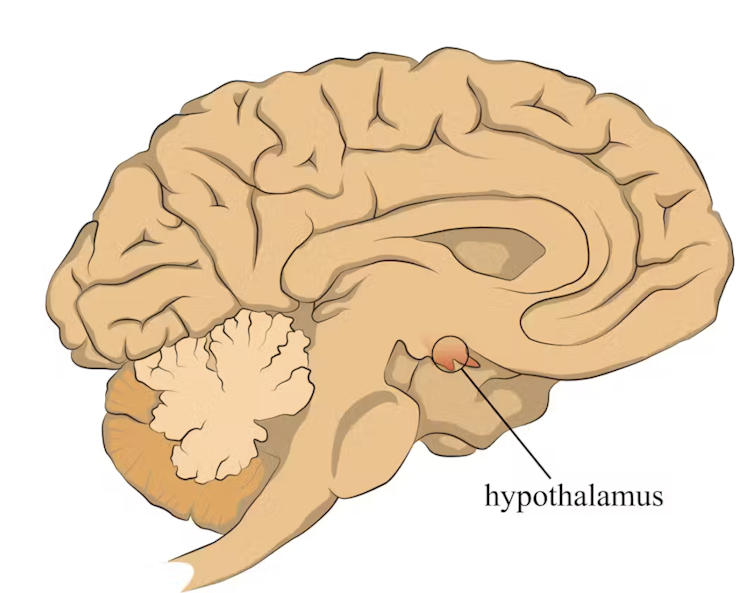
When faced with a perceived threat, psychological or physical, the hypothalamus region of the brain sets off an alarm system. This signals the release of a surge of hormones, including adrenaline and cortisol.
The hypothalamus sets off an alarm system in response to a real or perceived threat. stefan3andrei/Shutterstock In a typical stress response, cortisol levels quickly increase when stress occurs, and then rapidly drop back to normal once the stress has subsided. In the short term, cortisol suppresses inflammation, to ensure the body has enough energy available to respond to an immediate threat.
But in the longer term, chronic stress can be harmful. A Harvard University study from 2022 showed that people suffering from psychological distress in the lead up to their COVID infection had a greater chance of experiencing long COVID. They classified this distress as depression, probable anxiety, perceived stress, worry about COVID and loneliness.
Those suffering distress had close to a 50% greater risk of long COVID compared to other participants. Cortisol has been shown to be high in the most severe cases of COVID.
Stress causes inflammation
Inflammation is a short-term reaction to an injury or infection. It is responsible for trafficking immune cells in your body so the right cells are present in the right locations at the right times and at the right levels.
The immune cells also store a memory of that threat to respond faster and more effectively the next time.
Initially, circulating immune cells detect and flock to the site of infection. Messenger proteins, known as pro-inflammatory cytokines, are released by immune cells, to signal the danger and recruit help, and our immune system responds to neutralise the threat.
During this response to the infection, if the immune system produces too much of these inflammatory chemicals, it can trigger symptoms such as nasal congestion and runny nose.
Our immune response can trigger symptoms such as a runny nose. Alyona Mandrik/Shutterstock What about chronic stress?
Chronic stress causes persistently high cortisol secretion, which remains high even in the absence of an immediate stressor.
The immune system becomes desensitised and unresponsive to this cortisol suppression, increasing low-grade “silent” inflammation and the production of pro-inflammatory cytokines (the messenger proteins).
Immune cells become exhausted and start to malfunction. The body loses the ability to turn down the inflammatory response.
Over time, the immune system changes the way it responds by reprogramming to a “low surveillance mode”. The immune system misses early opportunities to destroy threats, and the process of recovery can take longer.
So how can you manage your stress?
We can actively strengthen our immunity and natural defences by managing our stress levels. Rather than letting stress build up, try to address it early and frequently by:
1) Getting enough sleep
Getting enough sleep reduces cortisol levels and inflammation. During sleep, the immune system releases cytokines, which help fight infections and inflammation.
2) Taking regular exercise
Exercising helps the lymphatic system (which balances bodily fluids as part of the immune system) circulate and allows immune cells to monitor for threats, while sweating flushes toxins. Physical activity also lowers stress hormone levels through the release of positive brain signals.
3) Eating a healthy diet
Ensuring your diet contains enough nutrients – such as the B vitamins, and the full breadth of minerals like magnesium, iron and zinc – during times of stress has a positive impact on overall stress levels. Staying hydrated helps the body to flush out toxins.
4) Socialising and practising meditation or mindfulness
These activities increase endorphins and serotonin, which improve mood and have anti-inflammatory effects. Breathing exercises and meditation stimulate the parasympathetic nervous system, which calms down our stress responses so we can “reset” and reduce cortisol levels.
Sathana Dushyanthen, Academic Specialist & Lecturer in Cancer Sciences & Digital Health| Superstar of STEM| Science Communicator, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
What Happens To Your Body When You Stop Drinking Alcohol
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Immediately after we stop drinking is rarely when we feel our best. But how long is it before we can expect to see benefits, instead of just suffering?
Timeline
After stopping drinking alcohol for…
- Seconds: the liver starts making progress filtering out toxins and sugars; ethanol starts to leave the system
- 1 hour: fatigue sets in as the body uses a lot of energy to metabolize and eliminate alcohol. However, sleep quality (if one goes to sleep now) is low because alcohol disrupts the brain patterns required for restful sleep
- 6–12 hours: the immune system starts recovering from the suppression caused by alcohol
- 24 hours: immune system is back to normal; withdrawal symptoms may occur in the case of heavy drinkers
- 3–5 days: resting blood pressure begins to drop, as stress levels decrease (alcohol may seem anxiolytic, but it is actually anxiogenic; it just masks its own effect in this regard). Also, because of insulin responses improving, appetite reduces. The liver, once it has finished dealing your last drinking session (if you used to drink all the time, it probably had a backlog to clear), can now begin to make repairs on itself.
- 1 week: skin will start looking better, as antidiuretic hormone levels neutralize, leading to a healthier maintenance of hydration
- 2 weeks: cognitive abilities improve as the brain begins to make progress in repairing itself. At the same time, kidneys start to heal.
- 3–4 weeks: the liver begins to regenerate in earnest. You may wonder what took it so long given the liver’s famous regenerative abilities, but in this case, the liver was also the organ that took the most damage from drinking, so its regeneration gets off to a slow start (in contrast, if the liver had “merely” suffered physical trauma, such as being shot, stabbed,
or eaten by eagles,it’d start regenerating vigorously as soon as the immediate wound-response had been tended to). Once it is able to pick up the pace though, overall health improves, as the liver can focus on breaking down other toxins. - 1–2 months: the heart is able to repair itself, and start to become stronger again (dependent on other lifestyle factors, of course).
- 3 months and more: bodily repairs continue (for example, the damage to the liver is often so severe that it can take quite a bit longer to recover completely, and repairs in the brain are always slow, for reasons beyond the scope of this article). Looking at the big picture, at this point we also see other benefits, such as reduced cancer risks.
In short… It’s never too soon to stop, but it’s also never too late, unless you are going to die in the next few days. So long as you’ll be in the land of the living for a few days yet, there’s time to enjoy the benefits of stopping.
Most importantly: the timeline for the most important repairs is not as long as many people might think, and that itself can be very motivating.
For more detail on much of the above, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Can We Drink To Good Health?
- How To Reduce Or Quit Alcohol
- Addiction Myths That Are Hard To Quit
- How To Unfatty A Fatty Liver
Take care!
Share This Post
Related Posts
-
Everything you need to know about cervical cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Every year, around 11,500 new cases of cervical cancer are diagnosed in the U.S. While cervical cancer used to be one of the most common causes of cancer death for U.S. women, the vaccine against the human papillomavirus (HPV), and increased early screening and detection have resulted in a decrease in rates.
“Cervical cancer is almost always preventable and typically diagnosed in patients who have either never had a screening test or have gone many years without one,” says Fred Wyand, director of communications at the American Sexual Health Association, which includes the National Cervical Cancer Coalition.
January is Cervical Cancer Awareness Month, so we spoke to experts to learn more about what it is, its symptoms, and what you can do to prevent it.
What is cervical cancer?
Cervical cancer is a type of cancer that starts in the cervix—the lower part of the uterus that connects the vagina to the uterus. Cervical cancer can affect anyone with a cervix but is most frequently diagnosed in women ages 35 to 44, according to the American Cancer Society.
There are two types:
- Squamous cell carcinoma: Cervical cancer that starts in the thin squamous cells on the outside of the cervix. This is the most common type of cervical cancer.
- Adenocarcinoma: Cervical cancer that starts in glandular cells that line the inside of the cervix. This type of cervical cancer is less common.
In some cases, cervical cancer has features of both types.
What causes cervical cancer?
Almost all cases of cervical cancer are caused by high-risk cases of HPV, a virus that is spread through sexual activity or other close skin-to-skin contact. But don’t panic: HPV is very common, and getting HPV doesn’t always mean you’ll get cervical cancer. Around 85 percent of people in the U.S. will get an HPV infection in their lifetime, but for most people, the virus clears on its own.
However, there are many strains of HPV, and some are linked to cervical cancer. In those cases, when the virus does not clear on its own and the HPV infection persists, it can cause a range of cancers in both men and women, including cancers of the cervix, anus, penis, throat, and vagina.
That’s why HPV vaccination is so important for all people: It can help prevent many types of cancer, including cervical cancer caused by those high-risk HPV infections.
What are the symptoms of cervical cancer?
Cervical cancer doesn’t usually have symptoms in its early stages, but once cancer begins to spread, the symptoms can include:
- Vaginal bleeding between periods, after sexual intercourse, or after menopause.
- Heavier and longer menstrual periods than usual.
- Vaginal discharge that has a strong odor and is watery.
- Pelvic pain or pain during sexual intercourse.
In more advanced stages, symptoms of cervical cancer can include:
- Leg swelling.
- Difficult or painful bowel movements or bleeding during a bowel movement.
- Blood in urine or difficulty urinating.
- Back pain.
“Most women present with no symptoms,” Dr. Kristina A. Butler, gynecologic oncologist at Mayo Clinic, tells PGN. “Therefore, the checkups with visualization of the cervix, speaking with your provider, and having a Pap smear are so important.”
How can you help prevent or reduce your risk for cervical cancer?
Vaccination: Cervical cancer is highly preventable. The most effective way to help protect yourself from it is by getting the HPV vaccine. The HPV vaccine is most effective before a person is first exposed to HPV, typically before becoming sexually active.
“If we are able to vaccinate children before they become adults [and] are subsequently exposed, those individuals are maximally protected against the [worst effects] of the virus, which could ultimately be cancer,” Butler adds.
You’re eligible to get the vaccine if you’re between 9 and 45 years old, but there are specific guidelines for each age group. The Centers for Disease Control and Prevention recommends HPV vaccination for children ages 11 or 12 (though it can start at 9 years).
The CDC says that you can get catch-up doses until you’re 26 if you didn’t get vaccinated earlier, but if you’re between 26 and 45 years old, you should talk to your health care provider about your individual risk for HPV and to see if you should get the vaccine.
Screenings: This is another effective way to prevent cervical cancer.
Dr. Deanna Gerber, a gynecologic oncologist at NYU Langone’s Laura and Isaac Perlmutter Cancer Center, tells PGN that regular screenings can catch HPV before it has a chance to become cancer.
“Now that we’re encouraging people to see their gynecologist and get screening more regularly, we’re catching cancer at earlier stages,” she says.
Screenings for cervical cancer include:
- Pap smear: During a Pap smear, also known as a Pap test, cells are collected from your cervix to find precancerous or cervical cancer cells. Pap smears should start at 21 years old, regardless of when you start having sex.
If you’re between 21 and 29, you should get a Pap smear every three years. If you’re 30 to 65 years old, it’s recommended you get one every three years, a Pap and HPV test together every five years, or an HPV test alone every five years.
- HPV test: During an HPV test, cells are collected from your cervix to look for infection with high-risk HPV strains that can cause cervical cancer. If you’re between 21 and 30 years old, it’s only recommended that you get an HPV test if you had an abnormal Pap smear result. After 30, an HPV test is recommended with a Pap smear every five years, as long as other results were normal.
(People over 65 years old should talk to their health care provider about whether they need screening.)
Not smoking: Avoiding smoking can reduce your risk of developing cervical cancer because “HPV and smoking tobacco work together to accelerate the negative effects of HPV,” says Gerber.
Wearing condoms: Although condoms don’t completely prevent HPV infection, they provide some protection. And according to the CDC, the use of condoms has been associated with a lower rate of cervical cancer.
There is hope with early detection
There is hope for people diagnosed with cervical cancer. “Compared to the survival [rates] 10 years ago, women survive much longer now with the great treatments we have,” adds Butler.
Some of those treatments and advances include radiation, chemotherapy, and surgical therapy.
And while there may be some stigma surrounding sexual health, it’s important to advocate for yourself, says Gerber.
“Being comfortable and bold talking to your doctor about your health or any concerns that you have, feeling comfortable with your provider by asking all these questions is really the best thing you can do.”
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
L-Theanine: What’s The Tea?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
L-Theanine: What’s The Tea?
We’ve touched previously on l-theanine, when this newsletter was new, and we had only a few hundred subscribers and the carefully organized format wasn’t yet what it is today.
So now it’s time to give this potent dietary compound / nutritional supplement the “Monday Research Review” treatment…
What is it?
L-theanine is an amino acid found in tea. The human body can’t produce it, and/but it’s not essential for humans. It does have a lot of benefits, though. See for example:
L-Theanine as a Functional Food Additive: Its Role in Disease Prevention and Health Promotion
How does it work?
L-theanine works by moderating and modulating the brain’s neurotransmitters.
This sounds fancy, but basically it means: it doesn’t actually add anything in the manner of a drug, but it changes how we use what we have naturally.
What does it do? Read on…
It increases mental focus
It has been believed that l-theanine requires the presence of caffeine to achieve this (i.e., it’s a combination-only effect). For example:
But as it turns out, when a group of researchers actually checked… This isn’t true, as Foxe et al. write:
❝We asked whether either compound alone, or both in combination, would affect performance of the task in terms of reduced error rates over time, and whether changes in alpha-band activity would show a relationship to such changes in performance. When treated with placebo, participants showed a rise in error rates, a pattern that is commonly observed with increasing time-on-task, whereas after caffeine and theanine ingestion, error rates were significantly reduced. The combined treatment did not confer any additional benefits over either compound alone, suggesting that the individual compounds may confer maximal benefits at the dosages employed❞
It promotes a calmly wakeful feeling of serenity
Those are not words typically found in biopharmaceutical literature, but they’re useful here to convey:
- L-theanine promotes relaxation without causing drowsiness
- L-theanine promotes mental alertness without being a stimulant
Here is where l-theanine really stands out from caffeine. If both substances promote mental focus, but one of them does it by making us “wired” and the other does it while simultaneously promoting calm, it makes the choice between them clearer!
Read more: L-theanine, a natural constituent in tea, and its effect on mental state
It relieves stress and anxiety
Building on from the above, but there’s more: l-theanine relieves stress and anxiety in people experiencing stressful situations, without any known harmful side effects… This is something that sets it apart from a lot of anxiolytic (antianxiety) drugs!
Here’s what a big systematic review of clinical trials had to say:
Theanine consumption, stress and anxiety in human clinical trials: A systematic review
L-theanine has other benefits too
We’ve talked about some of the most popular benefits of l-theanine, and we can’t make this newsletter too long, but research also suggests that it…
- Supports healthy weight management
- Reduces inflammation
- Supports immune health
- Helps fight cancer
- May extend lifespan ← this one’s a C. elegans study, but despite being a tiny worm, they actually function very similarly to humans on a cellular level; it’s why they’re used so much for anti-aging research
If you’re interested in this topic, we recommend also reading our previous article on l-theanine—pardon that we hadn’t really nailed down our style yet—but there’s a bunch of useful information about how l-theanine makes caffeine “better” in terms of benefits. We also talk dosage, and reference some other studies we didn’t have room to include today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The surprising ways ‘swimming off’ a hangover can be risky, even if alcohol has left your system
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s the morning after a big night and you’re feeling the effects of too much alcohol.
So it can be tempting to “refresh” and take the edge off a hangover with a swim at the beach, or a dip in the cool waters of your local river or pool.
But you might want to think twice.
The day after heavy drinking can affect your body, energy levels and perception of risk in many ways. This means you’re more likely to drown or make careless decisions – even without high levels of alcohol in your blood.
Wanderlust Media/Shutterstock Alcohol + water + summer = drowning
Alcohol is one of the main reasons why someone’s more likely to die due to drowning. And Australians consume a lot of it, including around the water.
The risk of drowning, and injury, including incidents involving alcohol, dramatically increases over the summer festive period – in particular on public holidays and long weekends.
Among people aged 18 and over who drowned in rivers where alcohol was involved, we found some 40% had a blood alcohol concentration of at least 0.20%. That’s four times the upper legal limit of 0.05% when driving a car on a full licence.
When we breathalysed people at four Australian rivers, we found higher levels of blood alcohol with higher temperatures, and particularly on public holidays.
At the beach, intoxication due to alcohol and/or drugs is involved in 23% of drowning deaths with an average blood alcohol concentration of 0.19%.
How about if you’re hungover?
Getting alcohol out of your body is a relatively slow process. On average, alcohol is metabolised at a rate of 0.015% per hour. So if someone stops drinking at 2am with a blood alcohol concentration of 0.20%, their alcohol levels don’t drop to zero until 4pm the next day.
Although hangovers can vary from person to person, typical symptoms include headache, muscle aches, fatigue, weakness, thirst, nausea, stomach pain, vertigo, irritability, sensitivity to light and sound, anxiety, sweating and increased blood pressure.
As well as feeling a bit dusty, the day after an evening of heavy drinking, you’re not so good at identifying risks and reacting to them.
In a pool, this might mean not noticing it’s too shallow to dive safely. In natural waterways, this might mean not noticing a strong river current or a rip current at the beach. Or someone might notice these hazards but swim or dive in anyway.
You don’t have to have alcohol in your blood to be affected. Fatigue can set in, leading you to make careless decisions. tismaja/Shutterstock In one study, we found that after a four-day Australian music festival where people drank heavily, even people who were sober (no longer had alcohol in their blood) were still affected.
Compared to baseline tests in the lab we ran three weeks before the festival, people who were sober the day after the festival had faster reaction times in a test to gauge their attention. But they made more mistakes. This suggests hangovers coupled with fatigue lead to quicker but more careless behaviour.
In and around water this could be the difference between life and death.
Positive blood alcohol readings, including of alcohol from the night before, are commonly implicated in drowning deaths as a result of risky behaviours such as jumping into the water, both at a river and along the coast. Jumping can cause physical injury or render you unconscious, leading to drowning.
Alcohol, including the day after drinking, can also make drowning more likely for a number of other reasons. It also reduces people’s coordination and reaction times.
What else is going on?
Alcohol makes the blood vessels near your skin open up (dilate). So more blood flows into them, making you feel hot. This means you may stay in colder water for longer, increasing your risk of hypothermia.
Alcohol can even make CPR (cardiopulmonary resuscitation) less effective, should you need to be resuscitated.
Normally, your body controls levels of certain minerals (or electrolytes) in the blood. But electrolyte imbalance is common after heavy drinking, including the day after. It’s the reason why hangover symptoms such as muscle pain can lead to cramps in your arms or legs. This can become dangerous when being in or on the water.
Low blood sugar levels the day after drinking is also common. This can lead to people becoming exhausted more quickly when doing physical activities, including swimming.
Other hazards include cold water, high waves and deep water, all of which your body may not be capable of dealing with if you’re feeling the effects of a big night.
What can we do about it?
Authorities regularly warn about the dangers of alcohol intoxication and being near the water. Young people and men are often targeted because these are the groups more likely to drown where alcohol is involved.
Beaches may have alcohol-free zones. Rivers rarely have the same rules, despite similar dangers. https://www.youtube.com/embed/5Salt-kkGUo?wmode=transparent&start=0 Royal Life Saving urges men to ‘make the right call’ and avoid alcohol around the water.
How to stay safe around water if you’re drinking
So take care this summer and stay out of the water if you’re not feeling your best:
- do your swimming before your drinking
- look out for your mates, especially ones who may have had a few too many or are hungover
- avoid getting back into the water after you’ve drunk alcohol or if you’re not feeling your best the next day.
Amy Peden, NHMRC Research Fellow, School of Population Health & co-founder UNSW Beach Safety Research Group, UNSW Sydney; Emmanuel Kuntsche, Director of the Centre for Alcohol Policy Research, La Trobe University, and Jasmin C. Lawes, Adjunct Senior Lecturer, UNSW Beach Safety Research Group, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: