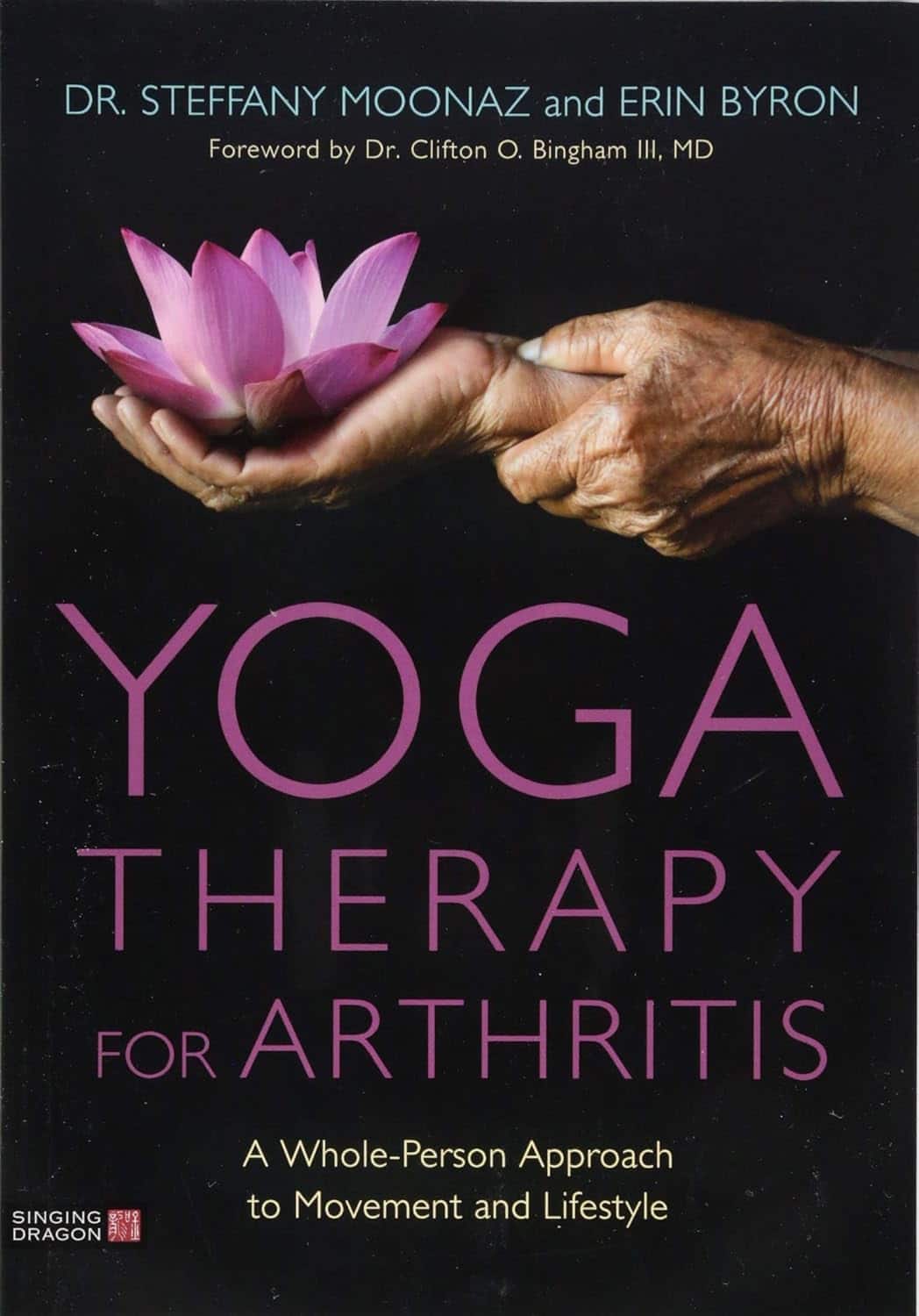
Yoga Therapy for Arthritis – by Dr. Steffany Moonaz & Erin Byron
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Two quick notes to start with:
- One of the problems with arthritis and exercise is that arthritis can often impede exercise.
- Another of the problems with arthritis and exercise is that some kinds of exercise can exacerbate arthritis.
This book deals with both of those issues, by providing yoga specifically tailored to living with arthritis. Indeed, the first-listed author’s PhD in public health was the result of 8 years of study developing an evidence-based yoga program for people with arthritis, including osteoarthritis and rheumatoid arthritis.
The authors take the view that arthritis is a whole-person disease (i.e. it affects all parts of you), and so addressing it requires a whole-person approach, which is what this book delivers.
As such, this is not just a book of asana (yoga postures). It does provide that, of course (as well as breathing exercises), but also its 328 pages additionally cover a lot of conscious work from the inside out, including attention to the brain, energy levels, pain, and so forth, and that the practice of yoga should not merely directly improve the joints via gentle physical exercise, but also should help to heal the whole person, including reducing stress levels, reducing physical tension, and with those two things, reducing inflammation also—and also, due to both that and the asana side of practice, better-functioning organs, which is always a bonus.
The style is interesting, as it refers to both science (8 pages of hard-science bibliography) and yogic principles (enough esoterica to put off, say, James Randi or Penn & Teller). This reviewer is very comfortable with both, and so if you, dear reader, are comfortable with both too, then you will surely enjoy this book.
Bottom line: if you or a loved one has arthritis, you’ll wish you got this book sooner.
Click here to check out Yoga Therapy For Arthritis, and live better!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Share This Post
-
Guava vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing guava to pineapple, we picked the guava.
Why?
Pineapple is great, but guava just beats it in most ways:
In terms of macros, guava has nearly 4x the fiber and nearly 5x the protein, for the same carbs, giving it the notably lower glycemic index. An easy win for guava in this category.
In the category of vitamins, guava has a lot more of vitamins A, B2, B3, B5, B9, C, E, K, and choline, while pineapple has marginally more vitamin B1. Another clear win for guava.
When it comes to minerals, guava has more calcium, copper, magnesium, phosphorus, potassium, selenium, and zinc, while pineapple has more iron and manganese. One more win for guava.
One big thing in pineapple’s favor is that it contains bromelain, which is an enzyme* found in pineapple (and only in pineapple), that has many very healthful properties, some of them unique to bromelain (and thus: unique to pineapple)
*actually a combination of enzymes, but most often referred to collectively in the singular. But when you do see it referred to as “they”, that’s what that means.
However cool that is, we think it unfair to weight it against guava winning in every other category, so we still say guava gets the overall win.
Of course, enjoy either or both; diversity is good!
Want to learn more?
You might like:
Let’s Get Fruity: Bromelain vs Inflammation & Much More
Enjoy!
Share This Post
-
Thinking of trying a new diet? 4 questions to ask yourself before you do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We live in a society that glorifies dieting, with around 42% of adults globally having tried to lose weight. Messages about dieting and weight loss are amplified on social media, with a never-ending cycle of weight loss fads and diet trends.
Amid often conflicting messages and misinformation, if you’re looking for diet advice online, it’s easy to become confused and overwhelmed.
So before diving into the latest weight loss trend or extreme diet, consider these four questions to help you make a more informed decision.
PeopleImages.com – Yuri A/Shutterstock 1. Is the diet realistic?
Have you considered the financial cost of maintaining the diet or lifestyle, and the time and resources that would be required? For example, do you need to purchase specific products, supplements, or follow a rigid meal plan?
If the diet is coming from someone who is trying to sell you something – such as a particular weight-loss product you need in order to follow the diet – this could be a particular red flag.
Many extreme diet recommendations come from a place of privilege and overlook food access, affordability, cooking skills, where you live, or even your culture and ethics.
If the diet has these sorts of issues it can lead to frustration, stress, stigmatisation and feelings of failure for the person trying to adhere to the diet. But the problem may be with the diet itself – not with you.
Many diets promoted online will be expensive, or require a lot of time and resources. artem evdokimov/Shutterstock 2. Is there evidence to support this diet?
Self-proclaimed “experts” online will often make claims focused on specific groups, known as target populations. This might be 30- to 50-year-old men with diabetes, for example.
In some cases, evidence for claims made may come from animal studies, which might not be applicable to humans at all.
So be aware that if research findings are for a group that doesn’t match your profile, then the results might not be relevant to you.
It takes time and a lot of high-quality studies to tell us a “diet” is safe and effective, not just one study. Ask yourself, is it supported by multiple studies in humans? Be critical and question the claims before you accept them.
For accurate information look for government websites, or ask your GP or dietitian.
3. How will this diet affect my life?
Food is much more than calories and nutrients. It plays many roles in our lives, and likewise diets can influence our lives in ways we often overlook.
Socially and culturally, food can be a point of connection and celebration. It can be a source of enjoyment, a source of comfort, or even a way to explore new parts of the world.
So when you’re considering a new diet, think about how it might affect meaningful moments for you. For example, if you’re going travelling, will your diet influence the food choices you make? Will you feel that you can’t sample the local cuisine? Or would you be deterred from going out for dinner with friends because of their choice of restaurant?
4. Will this diet make me feel guilty or affect my mental health?
What is your favourite meal? Does this diet “allow” you to eat it? Imagine visiting your mum who has prepared your favourite childhood meal. How will the diet affect your feelings about these special foods? Will it cause you to feel stressed or guilty about enjoying a birthday cake or a meal cooked by a loved one?
Studies have shown that dieting can negatively impact our mental health, and skipping meals can increase symptoms of depression and anxiety.
Many diets fail to consider the psychological aspects of eating, even though our mental health is just as important as physical health. Eating should not make you feel stressed, anxious, or guilty.
So before starting another diet, consider how it might affect your mental health.
Moving away from a dieting mindset
We’re frequently told that weight loss is the path to better health. Whereas, we can prioritise our health without focusing on our weight. Constant messages about the need to lose weight can also be harmful to mental health, and not necessarily helpful for physical health.
Our research has found eating in a way that prioritises health over weight loss is linked to a range of positive outcomes for our health and wellbeing. These include a more positive relationship with food, and less guilt and stress.
Our research also indicates mindful and intuitive eating practices – which focus on internal cues, body trust, and being present and mindful when eating – are related to lower levels of depression and stress, and greater body image and self-compassion.
But like anything, it takes practice and time to build a positive relationship with food. Be kind to yourself, seek out weight-inclusive health-care professionals, and the changes will come. Finally, remember you’re allowed to find joy in food.
Melissa Eaton, Accredited Practising Dietitian; PhD Candidate, University of Wollongong; Verena Vaiciurgis, Accredited Practising Dietitian; PhD Candidate, University of Wollongong, and Yasmine Probst, Associate Professor, School of Medical, Indigenous and Health Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Melatonin: A Safe, Natural Sleep Aid?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Melatonin: A safe sleep supplement?
Melatonin is a hormone normally made in our pineal gland. It helps regulate our circadian rhythm, by making us sleepy.
It has other roles too—it has a part to play in regulating immune function, something that also waxes and wanes as a typical day goes by.
Additionally, since melatonin and cortisol are antagonistic to each other, a sudden increase in either will decrease the other. Our brain takes advantage of this, by giving us a cortisol spike in the morning to help us wake up.
As a supplement, it’s generally enjoyed with the intention of inducing healthy, natural, restorative sleep.
Does it really induce healthy, natural, restorative, sleep?
Yes! Well, “natural” is a little subject and relative, if you’re taking it as a supplement, but it’s something your body produces naturally anyway.
Contrast with, for example, benzodiazepines (that whole family of medications with names ending in -azopan or -alozam), or other tranquilizing drugs that do not so much induce healthy sleep, but rather reduce your brain function and hopefully knock you out, and/but often have unwanted side effects, and a tendency to create dependency.
Melatonin, unlike most of those drugs, does not create dependency, and furthermore, we don’t develop tolerance to it. In other words, the same dose will continue working (we won’t need more and more).
In terms of benefits, melatonin not only reduces the time to fall asleep and increases total sleep time, but also (quite a bonus) improves sleep quality, too:
Meta-Analysis: Melatonin for the Treatment of Primary Sleep Disorders
Because it is a natural hormone rather than a drug with many side effects and interactions, it’s also beneficial for those who need good sleep and/but don’t want tranquilizing:
Any other benefits?
Yes! It can also help guard against Seasonal Affective Disorder, also called seasonal depression. Because SAD is not just about “not enough light = not enough serotonin”, but also partly about circadian rhythm and (the body is not so sure what time of day it is when there are long hours of darkness, or even, in the other hemisphere / other time of year, long hours of daylight), melatonin can help, by giving your brain something to “anchor” onto, provided you take it at the same time each day. See:
- Is seasonal affective disorder a disorder of circadian rhythms?
- The circadian basis of winter depression: the case for low-dose melatonin use
As a small bonus, melatonin also promotes HGH production (important for maintaining bone and muscle mass, especially in later life):
Anything we should worry about?
Assuming taking a recommended dose only (0.5mg–10mg per day), toxicity is highly unlikely, especially given that it has a half-life of only 40–60 minutes, so it’ll be eliminated quite quickly.
However! It does indeed induce sleepiness, so for example, don’t take melatonin and then try to drive or operate heavy machinery—or, ideally, do anything other than go to bed.
It can interfere with some medications. We mentioned that melatonin helps regulate immune function, so for example that’s something to bear in mind if you’re on immunosuppressants or otherwise have an autoimmune disorder. It can also interfere with blood pressure medications and blood thinners, and may make epilepsy meds less effective.
As ever, if in doubt, please speak with your doctor and/or pharmacist.
Where to get it?
As ever, we don’t sell it (or anything else), but for your convenience, here is an example product on Amazon.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why Do We Have Crooked Teeth When Our Ancestors Didn’t?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Evidence shows that people in ancient times typically had straight teeth set well into strong jaws, with even wisdom teeth fitting properly.
So, what went wrong? Did evolution do us a disservice?
Some information to chew on
Transition from hard-to-chew diets to processed, refined foods over millennia has reduced jaw size while tooth size stayed constant. Smaller jaws lead to tooth crowding, crookedness, and impacted wisdom teeth, requiring braces or extractions in modern times.
However, all is not lost!
Studies on non-human animals show softer diets reduce jaw and facial growth, causing dental crowding. In other words: dental crowding is primarily attributed to dietary and lifestyle changes, though genetics may play a role.
And notably, when it comes to humans, populations with less processed diets experience fewer dental problems, suggesting lifestyle modifications could help prevent tooth crowding.
And no, it is not too late. Remember, you are rebuilding your body all the time, including your bones!
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
The Exercises That Can Fix Sinus Problems (And More) ← this also improves the jaw structure
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
One Critical Mistake That Costs Seniors Their Mobility
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Will Harlow, the over-50s specialist physio, advises what to do instead:
Nose over toes
Often considered the most important test of mobility in later life (or in general, but later life is when it tends to decline) is the ability to get up off the floor without using your arms.
Many seniors, meanwhile, struggle to get out of a chair without using their arms.
Now, sitting in chairs in the first place is not good for the health, but that’s another matter and beyond the scope of today’s article.
If, perchance, you struggle to get up from a chair (especially if it’s low/deep, like many armchairs are) without using your hands, then here’s the way to do it:
- While practicing, cross your arms in front of you, so that you cannot use them.
- Shuffle yourself towards the front of the chair. No, don’t use your arms for this either, do a little butt-walk instead, to get you to the front edge of the chair.
- Lean forwards to position your nose over your toes (hence the mnemonic: “nose over toes”; memorize that!), as this will put your center of gravity where it needs to be.
- Now, push with your feet to rise up and forwards; slowly is better than quickly (quickly may be easier, but slowly will improve your strength and balance).
For more on all of this plus a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: