Why do I keep getting urinary tract infections? And why are chronic UTIs so hard to treat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing with chronic urinary tract infections (UTIs) means facing more than the occasional discomfort. It’s like being on a never ending battlefield against an unseen adversary, making simple daily activities a trial.
UTIs happen when bacteria sneak into the urinary system, causing pain and frequent trips to the bathroom.
Chronic UTIs take this to the next level, coming back repeatedly or never fully going away despite treatment. Chronic UTIs are typically diagnosed when a person experiences two or more infections within six months or three or more within a year.
They can happen to anyone, but some are more prone due to their body’s makeup or habits. Women are more likely to get UTIs than men, due to their shorter urethra and hormonal changes during menopause that can decrease the protective lining of the urinary tract. Sexually active people are also at greater risk, as bacteria can be transferred around the area.
Up to 60% of women will have at least one UTI in their lifetime. While effective treatments exist, about 25% of women face recurrent infections within six months. Around 20–30% of UTIs don’t respond to standard antibiotic. The challenge of chronic UTIs lies in bacteria’s ability to shield themselves against treatments.
Why are chronic UTIs so hard to treat?
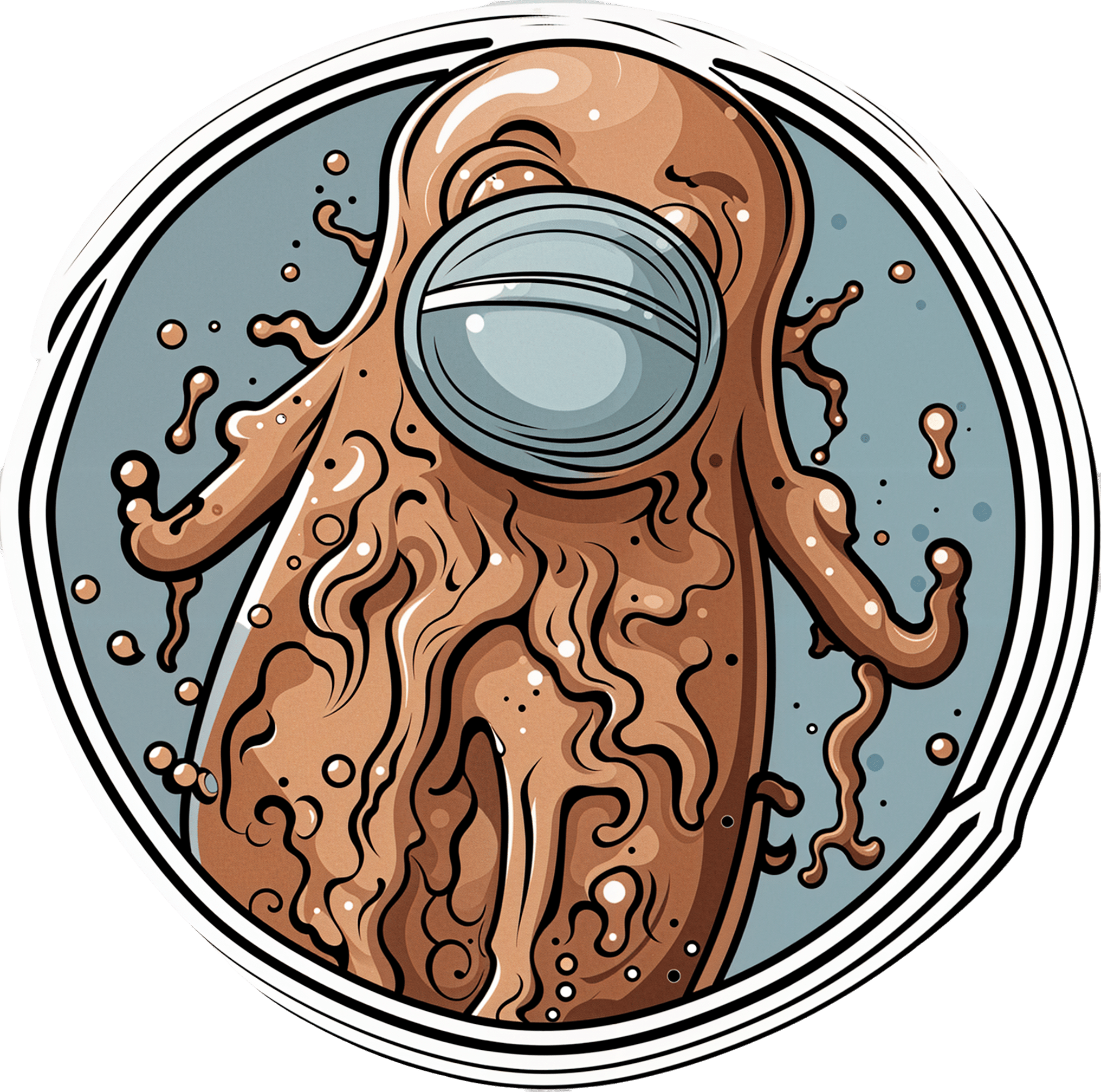
Once thought of as straightforward infections cured by antibiotics, we now know chronic UTIs are complex. The cunning nature of the bacteria responsible for the condition allows them to hide in bladder walls, out of antibiotics’ reach.
The bacteria form biofilms, a kind of protective barrier that makes them nearly impervious to standard antibiotic treatments.
This ability to evade treatment has led to a troubling increase in antibiotic resistance, a global health concern that renders some of the conventional treatments ineffective.

Michael Ebardt/Shutterstock
Antibiotics need to be advanced to keep up with evolving bacteria, in a similar way to the flu vaccine, which is updated annually to combat the latest strains of the flu virus. If we used the same flu vaccine year after year, its effectiveness would wane, just as overused antibiotics lose their power against bacteria that have adapted.
But fighting bacteria that resist antibiotics is much tougher than updating the flu vaccine. Bacteria change in ways that are harder to predict, making it more challenging to create new, effective antibiotics. It’s like a never-ending game where the bacteria are always one step ahead.
Treating chronic UTIs still relies heavily on antibiotics, but doctors are getting crafty, changing up medications or prescribing low doses over a longer time to outwit the bacteria.
Doctors are also placing a greater emphasis on thorough diagnostics to accurately identify chronic UTIs from the outset. By asking detailed questions about the duration and frequency of symptoms, health-care providers can better distinguish between isolated UTI episodes and chronic conditions.
The approach to initial treatment can significantly influence the likelihood of a UTI becoming chronic. Early, targeted therapy, based on the specific bacteria causing the infection and its antibiotic sensitivity, may reduce the risk of recurrence.
For post-menopausal women, estrogen therapy has shown promise in reducing the risk of recurrent UTIs. After menopause, the decrease in estrogen levels can lead to changes in the urinary tract that makes it more susceptible to infections. This treatment restores the balance of the vaginal and urinary tract environments, making it less likely for UTIs to occur.
Lifestyle changes, such as drinking more water and practising good hygiene like washing hands with soap after going to the toilet and the recommended front-to-back wiping for women, also play a big role.
Some swear by cranberry juice or supplements, though researchers are still figuring out how effective these remedies truly are.
What treatments might we see in the future?
Scientists are currently working on new treatments for chronic UTIs. One promising avenue is the development of vaccines aimed at preventing UTIs altogether, much like flu shots prepare our immune system to fend off the flu.

guys_who_shoot/Shutterstock
Another new method being looked at is called phage therapy. It uses special viruses called bacteriophages that go after and kill only the bad bacteria causing UTIs, while leaving the good bacteria in our body alone. This way, it doesn’t make the bacteria resistant to treatment, which is a big plus.
Researchers are also exploring the potential of probiotics. Probiotics introduce beneficial bacteria into the urinary tract to out-compete harmful pathogens. These good bacteria work by occupying space and resources in the urinary tract, making it harder for harmful pathogens to establish themselves.
Probiotics can also produce substances that inhibit the growth of harmful bacteria and enhance the body’s immune response.
Chronic UTIs represent a stubborn challenge, but with a mix of current treatments and promising research, we’re getting closer to a day when chronic UTIs are a thing of the past.
Iris Lim, Assistant Professor, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Here’s the latest you need to know about bird flu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Although bird flu continues to spread in wild birds, livestock, and humans, the risk to the public remains low.
- The majority of U.S. bird flu cases have been reported in farm workers who had direct contact with infected birds and cattle. Health officials are working to monitor the spread of the virus and improve protections for those most at risk.
- Recent data suggests that mutations in bird flu viruses could make them more dangerous to humans and potentially increase the risk of a pandemic.
- On January 6, Louisiana health officials confirmed the first U.S. death from bird flu.
Throughout 2024, dozens of human cases of H5N1 bird flu were detected as the virus spreads rapidly in livestock. The current risk to humans is low but not nonexistent. Here’s everything you need to know about the current status and future outlook of H5 bird flu in the United States.
Current U.S. bird flu status (as of January 6, 2025)
As of January 6, 66 human bird flu cases have been reported in eight states. Over half of all cases are in California. The state’s governor declared a state of emergency as a “proactive” action against bird flu on December 18.
On January 6, the Louisiana Department of Health reported the first U.S. bird flu death. The patient, a man over age 65, was previously confirmed to be the first severe bird flu case in the U.S. and the first case linked to backyard flocks. The department emphasized that the risk to the public is low and that no new cases or evidence of human transmission have been detected in the state.
All but two human bird flu cases this year were in farm workers who were exposed to infected livestock. The exposure source of the remaining cases—one in California and one in Missouri—is unknown.
The CDC reported on November 22 that a child in California tested positive for bird flu, the first known pediatric bird flu case in the U.S. However, it is unclear how the child contracted the virus, as they had no known contact with infected animals.
To date, there have been no reports of human transmission of bird flu during the current outbreak. Additionally, most human cases have not been severe, and no deaths have been reported. For these reasons, experts are confident that the bird flu risk to humans remains low.
“In the short term, there is very little threat,” Dr. Scott Roberts, an infectious diseases specialist with Yale Medicine said. “The risk for the general public is so low,” he emphasized to Yale Medicine.
How the U.S. is monitoring bird flu
The CDC continues to monitor the circulation of bird flu in humans as part of its year-round flu monitoring. The agency is also working to improve protections for farm workers, who are at the highest risk of contracting bird flu.
In November 2024, the CDC also announced expanded actions and updated guidance for farm workers, including improved access to and training for using personal protective equipment (such as N95 face masks), more rigorous testing procedures, and increased outreach. These updates followed a CDC report finding that 7 percent of participating dairy workers had signs of a recent bird flu infection. A second CDC study, also released in November, found inadequate use of personal protective equipment among dairy workers on farms with bird flu outbreaks.
After the H5N1 virus was found in raw milk being sold in California, the U.S. Department of Agriculture announced on December 6 that unpasteurized milk must be tested for bird flu. The USDA order also requires dairy farms with positive bird flu cases to cooperate with health officials in disease surveillance.
Is a bird flu pandemic possible?
In early November, a Canadian teen was hospitalized with bird flu caused by a virus that’s closely related to the H5N1 virus circulating in the U.S. The case has troubled experts for a few reasons.
First, it is Canada’s first human bird flu case where the patient was not infected while traveling, and the source of exposure is unknown. Second, the teen experienced severe symptoms and developed a lung infection requiring critical care, raising concern that bird flu infections may be more severe in younger people.
The final and biggest concern about the case is that genetic analysis revealed several changes in the virus’s DNA sequence, called mutations, that could potentially make the virus better able to infect humans. Researchers say that two of those mutations could make it easier for the virus to infect humans, and another one may make it easier for the virus to replicate after infecting a human. However, it’s unclear if the changes occurred before or after the teen was infected.
Scott Hensley, a professor of microbiology at the University of Pennsylvania, told Nature that “this should serve as a warning: this virus has the capacity to switch very quickly into a form that can cause severe disease.”
Notably, even in this more severe case, there is still no evidence of human transmission, which is necessary for a potential bird flu pandemic. However, the case underscores the risk of new and potentially dangerous mutations emerging as the H5N1 virus continues to spread and multiply.
A study published in Science on December 5 found that a genetic change on a protein on the surface of the virus could make it easier for the virus to attach to and infect human cells. But none of the mutations observed in the Canadian case are those identified in the study.
Importantly, the researchers stressed that the ability of the virus to attach to a specific part of human cells “is not the only [factor] required for human-to-human transmission of influenza viruses.”
How to stay safe
Most people are not at high risk of being exposed to bird flu. The virus is spreading between animals and from animals to humans through direct contact. The CDC recommends avoiding the consumption of raw milk products and direct contact with wild birds and potentially infected livestock.
“Pasteurization kills the bird flu virus and other harmful germs that can be found in raw milk,” says a November 24 California Department of Public Health press release. “CDPH advises consumers not to drink raw milk or eat raw milk products due to the risk of foodborne illnesses.”
Additionally, although the annual flu shot does not protect against bird flu, getting vaccinated helps prevent infection with seasonal flu and bird flu at the same time. In very rare instances, getting infected by two influenza viruses at the same time can result in a combination of genetic material that produces a new virus.
This phenomenon, known as antigenic shift, triggered the 2009 swine flu pandemic.
Learn more about how to protect yourself and your loved ones against bird flu.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Patient Underwent One Surgery but Was Billed for Two. Even After Being Sued, She Refused To Pay.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Jamie Holmes says a surgery center tried to make her pay for two operations after she underwent only one. She refused to buckle, even after a collection agency sued her last winter.
Holmes, who lives in northwestern Washington state, had surgery in 2019 to have her fallopian tubes tied, a permanent birth-control procedure that her insurance company agreed ahead of time to cover.
During the operation, while Holmes was under anesthesia, the surgeon noticed early signs of endometriosis, a common condition in which fibrous scar tissue grows around the uterus, Holmes said. She said the surgeon later told her he spent about 15 minutes cauterizing the troublesome tissue as a precaution. She recalls him saying he finished the whole operation within the 60 minutes that had been allotted for the tubal ligation procedure alone.
She said the doctor assured her the extra treatment for endometriosis would cost her little, if anything.
Then the bill came.
The Patient: Jamie Holmes, 38, of Lynden, Washington, who was insured by Premera Blue Cross at the time.
Medical Services: A tubal ligation operation, plus treatment of endometriosis found during the surgery.
Service Provider: Pacific Rim Outpatient Surgery Center of Bellingham, Washington, which has since been purchased, closed, and reopened under a new name.
Total Bill: $9,620. Insurance paid $1,262 to the in-network center. After adjusting for prices allowed under the insurer’s contract, the center billed Holmes $2,605. A collection agency later acquired the debt and sued her for $3,792.19, including interest and fees.
What Gives: The surgery center, which provided the facility and support staff for her operation, sent a bill suggesting that Holmes underwent two separate operations, one to have her tubes tied and one to treat endometriosis. It charged $4,810 for each.
Holmes said there were no such problems with the separate bills from the surgeon and anesthesiologist, which the insurer paid.
Holmes figured someone in the center’s billing department mistakenly thought she’d been on the operating table twice. She said she tried to explain it to the staff, to no avail.
She said it was as if she ordered a meal at a fast-food restaurant, was given extra fries, and then was charged for two whole meals. “I didn’t get the extra burger and drink and a toy,” she joked.
Her insurer, Premera Blue Cross, declined to pay for two operations, she said. The surgery center billed Holmes for much of the difference. She refused to pay.
Holmes said she understands the surgery center could have incurred additional costs for the approximately 15 minutes the surgeon spent cauterizing the spots of endometriosis. About $500 would have seemed like a fair charge to her. “I’m not opposed to paying for that,” she said. “I am opposed to paying for a whole bunch of things I didn’t receive.”
The physician-owned surgery center was later purchased and closed by PeaceHealth, a regional health system. But the debt was turned over to a collection agency, SB&C, which filed suit against Holmes in December 2023, seeking $3,792.19, including interest and fees.
The collection agency asked a judge to grant summary judgment, which could have allowed the company to garnish wages from Holmes’ job as a graphic artist and marketing specialist for real estate agents.
Holmes said she filed a written response, then showed up on Zoom and at the courthouse for two hearings, during which she explained her side, without bringing a lawyer. The judge ruled in February that the collection agency was not entitled to summary judgment, because the facts of the case were in dispute.
More From Bill Of The Month
- Her Hearing Implant Was Preapproved. Nonetheless, She Got $139,000 Bills for Months.
- It’s Called an Urgent Care Emergency Center — But Which Is It?
- He Fell Ill on a Cruise. Before He Boarded the Rescue Boat, They Handed Him the Bill.
Representatives of the collection agency and the defunct surgery center declined to comment for this article.
Sabrina Corlette, co-director of Georgetown University’s Center on Health Insurance Reforms, said it was absurd for the surgery center to bill for two operations and then refuse to back down when the situation was explained. “It’s like a Kafka novel,” she said.
Corlette said surgery center staffers should be accustomed to such scenarios. “It is quite common, I would think, for a surgeon to look inside somebody and say, ‘Oh, there’s this other thing going on. I’m going to deal with it while I’ve got the patient on the operating table.’”
It wouldn’t have made medical or financial sense for the surgeon to make Holmes undergo a separate operation for the secondary issue, she said.
Corlette said that if the surgery center was still in business, she would advise the patient to file a complaint with state regulators.
The Resolution: So far, the collection agency has not pressed ahead with its lawsuit by seeking a trial after the judge’s ruling. Holmes said that if the agency continues to sue her over the debt, she might hire a lawyer and sue them back, seeking damages and attorney fees.
She could have arranged to pay off the amount in installments. But she’s standing on principle, she said.
“I just got stonewalled so badly. They treated me like an idiot,” she said. “If they’re going to be petty to me, I’m willing to be petty right back.”
The Takeaway: Don’t be afraid to fight a bogus medical bill, even if the dispute goes to court.
Debt collectors often seek summary judgment, which allows them to garnish wages or take other measures to seize money without going to the trouble of proving in a trial that they are entitled to payments. If the consumers being sued don’t show up to tell their side in court hearings, judges often grant summary judgment to the debt collectors.
However, if the facts of a case are in dispute — for example, because the defendant shows up and argues she owes for just one surgery, not two — the judge may deny summary judgment and send the case to trial. That forces the debt collector to choose: spend more time and money pursuing the debt or drop it.
“You know what? It pays to be stubborn in situations like this,” said Berneta Haynes, a senior attorney for the National Consumer Law Center who reviewed Holmes’ bill for KFF Health News.
Many people don’t go to such hearings, sometimes because they didn’t get enough notice, don’t read English, or don’t have time, she said.
“I think a lot of folks just cave” after they’re sued, Haynes said.
Emily Siner reported the audio story.
After six years, we’ll have a final installment with NPR of our Bill of the Month project in the fall. But Bill of the Month will continue at KFF Health News and elsewhere. We still want to hear about your confusing or outrageous medical bills. Visit Bill of the Month to share your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Why Fibromyalgia Is Not An Acceptable Diagnosis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Efrat Lamandre makes the case that fibromyalgia is less of a useful diagnosis and more of a rubber stamp, much like the role historically often fulfilled by “heart failure” as an official cause of death (because certainly, that heart sure did stop beating). It’s a way of answering the question without answering the question.
…and what to look for instead
Fibromyalgia is characterized by chronic pain, tenderness, sleep disturbances, fatigue, and other symptoms. It’s often considered an “invisible” illness, because it’s the kind that’s easy to dismiss if you’re not the one carrying it. A broken leg, one can point at and see it’s broken; a respiratory infection, one can see its effects and even test for presence of the pathogen and/or its antigens. But fibromyalgia? “It hurts and I’m tired” doesn’t quite cut it.
Much like “heart failure” as a cause of death when nothing else is indicated, fibromyalgia is a diagnosis that gets applied when known causes of chronic pain have been ruled out.
Dr. Lamandre advocates for functional medicine and seeking the underlying causes of the symptoms, rather than the industry standard approach, which is to just manage the symptoms themselves with medications (of course, managing the symptoms with medications has its place; there is no need to suffer needlessly if pain relief can be used; it’s just not a sufficient response).
She notes that potential triggers for fibromyalgia include microbiome imbalances, food sensitivities, thyroid issues, nutrient deficiencies, adrenal fatigue, mitochondrial dysfunction, mold toxicity, Lyme disease, and more. Is this really just one illness? Maybe, but quite possibly not.
In short… If you are given a diagnosis of fibromyalgia, she advises that you insist doctors keep on looking, because that’s not an answer.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Managing Chronic Pain (Realistically!)
- How To Eat To Beat Chronic Fatigue ← yes, including how to do so when you are chronically fatigued. In other words, this isn’t just dietary advice, but rather practical advice too
- When Painkillers Aren’t Helping, These Things Might
Take care!
Share This Post
Related Posts
-
Cherries vs Elderberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cherries to elderberries, we picked the elderberries.
Why?
Both are great! But putting them head-to-head…
In terms of macros, cherries have slightly more protein (but we are talking miniscule numbers here, 0.34mg/100g), while elderberries have moderately more carbs and more than 4x the fiber. This carbs:fiber ratio difference means that elderberries have the lower glycemic index by far, as well as simply more grams/100g fiber, making this an easy win for elderberries.
In the category of vitamins, cherries have more of vitamins A, B9, E, K, and choline, while elderberries have more of vitamins B1, B2, B3, B6, and C. The margins of difference mean that elderberries have the very slightly better overall vitamin coverage, but it’s so slight that we’ll call this a 5:5 tie.
When it comes to minerals, cherries have more copper, magnesium, and manganese, while elderberries have more calcium, iron, phosphorus, potassium, selenium, and zinc. A nice easy win to top it off for elderberries.
On the polyphenols (and other phytochemicals) front, both are great in different ways, nothing that’d we’d consider truly sets one ahead of the other.
All in all, adding up the sections, an overall win for elderberries, but by all means enjoy either or both!
Want to learn more?
You might like to read:
- Cherries’ Very Healthy Wealth Of Benefits!
- Herbs for Evidence-Based Health & Healing ← one of them is elderberry, which hastens recovery from upper respiratory viral infections 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tranquility by Tuesday?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
I Know How She Does It: How Successful Women Make The Most of Their Time
This is Laura Vanderkam, author of “Tranquility By Tuesday” (amongst other books). Her “thing” is spending more time on what’s important, and less on what isn’t. Sounds simple, but she’s made a career out of it, so condensed here for you are…
Laura’s 7 Keys To Productivity
Key One: Plan your weeks on Fridays
You don’t want your Monday morning to be a “James Bond intro” (where everything is already in action and you’re just along for the ride, trying to figure out what’s going on). So, take some time last thing each Friday, to plan ahead for the following week!
Key Two: Measure what matters
Whatever that means to you. Laura tracks her use of time in half-hour blocks, and likes keeping track of streaks. For her, that means running daily and keeping a log of it. She also keeps track of the books she reads. For someone else it could be music practice, or a Duolingo streak, or eating fruit each day.
On which note…
“Dr. Greger’s Daily Dozen” is simpler than most nutrition trackers (where you must search for everything you eat, or scan barcodes for all ingredients).
Instead, it keeps track of whether you are having certain key health-giving foods often enough to maintain good health.
We might feature his method in a future edition of 10almonds, but for now, check the app out for yourself here:
Get Dr. Greger’s Daily Dozen on iOS / Get Dr. Greger’s Daily Dozen on Android
Dr. Greger’s Daily Dozen @ Nutrition Facts
Key Three: Figure out 2–3 “anchor” events for the weekend
Otherwise, it can become a bit of a haze and on Monday you find yourself thinking “where did the weekend go?”. So, plan some stuff! It doesn’t have to be anything out-of-this-world, just something that you can look forward to in advance and remember afterwards. It could be a meal out with your family, or a session doing some gardening, or a romantic night in with your partner. Whatever makes your life “living” and not passing you by!
Key Four: Tackle the toughest work first
You’ve probably heard about “swallowing frogs”. If not, there are various versions, usually attributed to Mark Twain.
Here’s one:
“If it’s your job to eat a frog, it’s best to do it first thing in the morning. And if it’s your job to eat two frogs, it’s best to eat the biggest one first.”
Top Productivity App “ToDoist” has an option for this, by the way!
Laura’s key advice here is: get the hard stuff done now! Before you get distracted or tired and postpone it to tomorrow (and then lather rinse repeat, so it never gets done)
10almonds Tip:
“But what if something’s really important but not as pressing as some less important, but more urgent tasks?”
Simple!
Set a timer (we love the Pomodoro method, by the way) and do one burst of the important-but-not-urgent task first. Then you can get to the more urgent stuff.
Repeat each day until the important-but-not-urgent task is done!
The 10almonds Team
Key Five: Use bits of time well
If, like many of us, you’ve a neverending “to read” list, use the 5–10 minute breaks that get enforced upon us periodically through the day!
- Use those few minutes before a meeting/phonecall!
- Use the time you spend waiting for public transport or riding on it!
- Use the time you spent waiting for a family member to finish doing a thing!
All those 5–10 minute bits soon add up… You might as well spend that time reading something you know will add value to your life, rather than browsing social media, for example.
Key Six: Make very short daily to-do lists
By “short”, Laura considers this “under 10 items”. Do this as the last part of your working day, ready for tomorrow. Not at bedtime! Bedtime is for winding down, not winding up
Key Seven: Have a bedtime
Laura shoots for 10:30pm, but whatever works for you and your morning responsibilities. Your morning responsibilities aren’t tied to a specific time? Lucky you, but try to keep a bedtime anyway. Otherwise, your daily rhythm can end up sliding around the clock, especially if you work from home!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A Peek Behind The 10almonds Curtain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At 10almonds we give a lot of health information, so you may wonder: how much do we (the 10almonds team) put into practice? Is it even possible to do all these things? Do we have an 80:20 rule going on?
So, here’s what someone who thinks, reads, and writes about health all day, does for her health—and how it ties in with what you read here at 10almonds.
Hi, it’s me, a member of the 10almonds team and regular writer here, and I’m going to do the rest of this article in the first-person, since it’s using me as an example!
(PS: yes, the thumbnail is a digital impression of my appearance, though I would correct it that my hair is much longer, and my eyes are more gray; I must admit though it captured my smile, not to mention my collarbones-that-you-could-sit-on)
Dietary habits
Before we get to foods, let’s talk intermittent fasting. I practise 16:8 intermittent fasting… Approximately. That is to say, I’m mostly not religious about it, but I will generally breakfast around 12 noon, and have finished eating dinner before 8pm, with no food outside of those hours.
See also: Intermittent Fasting: What’s the truth?
Importantly, while I feel free to be a little flexible around start and finish times, I do very consciously decide “I am now fasting” and “I will now break the fast”.
Note my imperfection: it would be ideal to have the eating period earlier in the day, and have a bigger breakfast and small dinner. However, that doesn’t really work for me (leisurely evening meal is an important daily event in this household), so this is how I do it instead.
Foods!
It gets an exclamation mark because a thing about me is that I do love foods.
Breakfast: a typical breakfast for me these past months is a couple of ounces of mixed nuts with about 1oz of goji berries.
The mixed nuts are in equal proportions: almonds, walnuts, hazelnuts, cashews. Why those four? Simple, it’s because that’s what Aldi sells as “mixed nuts” and they are the cheapest nuts around, as well as containing absolute nutritional heavyweights almonds and walnuts in generous portions.
Often, but not always, I’ll have some dates with it, or dried apricots, or prunes.
I go through phases; sometimes I’ll enjoy overnight oats as my breakfast for a month or two at a time. I really just follow my gut in this regard.
See for example: Spiced Pear & Pecan Polyphenol Porridge
Lunch: I don’t really lunch per se, but between breakfast and dinner I’ll usually snack on a 3–5 organic carrots (I literally just cut the tops off and otherwise eat them like Bugs Bunny—peeling them would be extra work just to lose fiber). Note my imperfection: I don’t buy all of my vegetables organic, but I do for the ones where it makes the biggest difference.
If I’m feeling like it, I may lunch on a selection of herbs sabzi khordan style (see: Invigorating Sabzi Khordan), though I’m vegan so for simplicity I just skip the cheeses that are also traditional with that dish. On the other hand, for protein and fat I’ll usually add a cup of beans (usually black beans or kidney beans), seasoned with garlic and black pepper in an olive oil and balsamic vinegar dressing (that I make myself, so it’s just those ingredients). See also: Kidney Beans vs Black Beans – Which Is Healthier?
Dinner: this is my main sit-down meal of the day, and it’s enjoyed in a leisurely fashion (say, 40 minutes average with a normal distribution bell curve running between 20 and 60 minutes) with my son who lives with me. I mention all of this, because of the importance of relaxed mindful eating. In the instances of it being nearer the 20 minutes end, it’s not because of rushing, but rather because of a lighter meal some days.
See also: How To Get More Nutrition From The Same Food
Regular recurrences in the menu include:
I’ll often snack on something probiotic (e.g. kimchi) while I’m cooking.
See also: Make Friends With Your Gut! (You Can Thank Us Later)
In terms of what’s not in my diet: as mentioned, I’m vegan, so animal products are out. I don’t drink alcohol or use other recreational drugs, and I mostly drink decaffeinated coffee, but I’ll have a caffeinated one if I’m out somewhere. I’m not a puritan when it comes to sugar, but also, I simply don’t like it and I know well its health effects, so it doesn’t really form part of my diet except insofar as it’s in some ready-made condiments I may sometimes use (e.g. sriracha, teriyaki sauce). I’m also not a puritan when it comes to wheat, but it’s not something I consume daily. Usually on a weekly basis I’ll have a wholegrain pasta dish, and a dish with some kind of wholegrain flatbread.
See also:
Exercise!
First, some things that are lifestyle factors:
- I do not own a car, and I dislike riding in cars, buses, etc. So, I walk everywhere, unless it’s far enough that I must take the train, and even then I usually stand between carriages rather than sitting down.
- I have a standing desk setup, that hasn’t been lowered even once since I got it. I highly recommend it, as someone who spends a lot of time at my desk.
- You may imagine that I spend a lot of time reading; if it’s books (as opposed to scientific papers etc, which I read at my desk), then I’ll most of the time read them while perched like a gargoyle in a sitting squat (Slav squat, Asian squat, resting squat, deep squat, etc) on a balance ball. Yes, it is comfortable once you’re used to it!
About that latter, see also: The Most Anti Aging Exercise
In terms of “actual” exercise, I get 150–300 minutes “moderate exercise” per week, which is mostly composed of:
- Most days I walk into town to get groceries; it’s a 40-minute round trip on foot
- On days I don’t do that, even if I do walk to a more local shop, I spend at least 20 minutes on my treadmill.
See also: The Doctor Who Wants Us To Exercise Less, & Move More
Strength and mobility training, for me, comes mostly in what has been called “exercise snacking”, that is to say, I intersperse my working day with brief breaks to do Pilates exercises. I have theme days (lower body, core, upper body) and on average one rest day (from Pilates exercises) per week, though honestly, that’s usually more likely because of time constraints than anything else, because a deadline is looming.
See also: Four Habits That Drastically Improve Mobility
You may be wondering about HIIT: when I’m feeling extra-serious about it, I use my exercise bike for this, but I’ll be honest, I don’t love the bike, so on a daily basis, I’m much more likely to do HIIT by blasting out a hundred or so Hindu squats, resting, and repeating.
See also: How To Do HIIT (Without Wrecking Your Body)
Supplements
First I’ll mention, I do have HRT, of which the hormones I have are bioidentical estradiol gel in the morning, and a progesterone pessary in the evening. They may not be for everybody, but they’ve made a world of difference to me.
See also: HRT: A Tale Of Two Approaches
In terms of what one usually means when one says supplements, many I use intermittently (which is good in some cases, as otherwise the body may stop using them so well, or other problems can arise), but regular features include:
- Magnesium glycinate, malate, & citrate (See: Which Magnesium? (And: When?))
- Active vitamers of vitamins B9 and B12 (See: Which B Vitamins? It Makes A Difference!)
- Liposomal vitamin C (I actually get enough for general purposes in my diet, but as a vegan I don’t get dietary collagen, so this helps collagen synthesis)
- L-theanine (bedtime only) (See: L-Theanine: What’s The Tea?)
- Lion’s mane mushroom (See: What does lion’s mane mushroom actually do, anyway?)
- Quercetin (See: Fight Inflammation & Protect Your Brain, With Quercetin)
- Fisetin (weekends only) (See: Fisetin: The Anti-Aging Assassin)
Why weekends only for Fisetin? See: The Drug & Supplement Combo That Reverses Aging ← the supplement is fisetin, which outperforms quercetin in this role, and/but it only needs be taken for two days every two weeks, as a sort of “clearing out” of senescent cells. There is no need to take it every day, because if you just cleared out your senescent cells, then guess what, they’re not there now. Also, while sensescent cells are a major cause of aging, on a lower level they do have some anti-tumor effects, so it can be good to let some live a least for a while now and again. In short, cellular sensescence can help prevent tumors on a daily level, but it doesn’t hurt that capacity to have a clearing-out every couple of weeks; so says the science (linked above). Note my imperfection: I take it at weekends instead of for two days every two weeks (as is standard in studies, like those linked above), because it is simpler than remembering to count the weeks.
Cognitive exercise
Lest we forget, exercising our mind is also important! In my case:
- I’m blessed to have work that’s quite cognitively stimulating; our topics here at 10almonds are interesting. If it weren’t for that, I’d still be reading and writing a lot.
- I play chess, though these days I don’t play competitively anymore, and play rather for the social aspect, but this too is important in avoiding cognitive decline.
- I am one of those people who compulsively learns languages, and uses them a lot. This is very beneficial, as language ability is maintained in a few small areas of the brain, and it’s very much “use it or lose it”. Now, while I may not need my French or Russian or Arabic to keep the lights on in this part of the brain or that, the fact that I am pushing my limits every day is the important part. It’s not about how much I know—it’s about how much I engage those parts of my brain on a daily basis. Thus, even if you speak only one language right now, learning even just one more, and learning even only a little bit, you will gain the brain benefits—because you’re engaging it regularly in a new way, and that forces the brain to wire new synapses and also to maintain volume in those parts.
See also: How To Reduce Your Alzheimer’s Risk
And about language-learning specifically: An Underrated Tool Against Alzheimer’s ←this also shows how you don’t have to be extreme about language learning like I admittedly am.
How’s all this working out for me?
I can say: it works! My general health is better now than it was decades ago. I’ve personally focused a lot on reducing inflammation, and that really pays dividends when it comes to the rest of health. I didn’t talk about it above, but focusing on my sleep regularity and quality has helped a lot too.
In terms of measurable results, I recently had a general wellness checkup done by means of a comprehensive panel of 14 blood tests, and various physical metrics (BMI, body fat %, blood pressure, etc), and per those, I could not be in better health; it was as though I had cheated and written in all the best answers. I say this not to brag (you don’t know me, after all), but rather to say: it can be done!
Even without extreme resources, and without an abundance of free time, etc, it can be done!
Caveat: if you have some currently incurable chronic disease, there may be some limits. For example, if you have Type 1 Diabetes, probably your HbA1c* is going to be a little off even if you do everything right.
*HbA1c = glycated hemoglobin, a very accurate measure of what your blood glucose has been on average for the past 2–3 months—why 2–3 months? Because that’s the approximate lifespan of a red blood cell, and we’re measuring how much hemoglobin (in the red blood cells) has been glycated (because of blood glucose).
In summary
The stuff we write about at 10almonds can be implemented, on a modest budget and while juggling responsibilities (work, family, classes, etc).
I’m not saying that my lifestyle should be everyone’s template, but it’s at least an example of one that can work.
- Maybe you hate walking and love swimming.
- Maybe you have no wish to give up fish and eggs, say (both of which are fine/good in moderation healthwise).
- Maybe you have different priorities with supplements.
- Maybe you find language-learning uninteresting but take singing lessons.
- And so on.
In the absolute fewest words, the real template is:
- Decide your health priorities (what matters most for you)
- Look them up on 10almonds
- Put the things into action in a way that works for you!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: