Who will look after us in our final years? A pay rise alone won’t solve aged-care workforce shortages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged-care workers will receive a significant pay increase after the Fair Work Commission ruled they deserved substantial wage rises of up to 28%. The federal government has committed to the increases, but is yet to announce when they will start.
But while wage rises for aged-care workers are welcome, this measure alone will not fix all workforce problems in the sector. The number of people over 80 is expected to triple over the next 40 years, driving an increase in the number of aged care workers needed.
How did we get here?
The Royal Commission into Aged Care Quality and Safety, which delivered its final report in March 2021, identified a litany of tragic failures in the regulation and delivery of aged care.
The former Liberal government was dragged reluctantly to accept that a total revamp of the aged-care system was needed. But its weak response left the heavy lifting to the incoming Labor government.
The current government’s response started well, with a significant injection of funding and a promising regulatory response. But it too has failed to pursue a visionary response to the problems identified by the Royal Commission.
Action was needed on four fronts:
- ensuring enough staff to provide care
- building a functioning regulatory system to encourage good care and weed out bad providers
- designing and introducing a fair payment system to distribute funds to providers and
- implementing a financing system to pay for it all and achieve intergenerational equity.
A government taskforce which proposed a timid response to the fourth challenge – an equitable financing system – was released at the start of last week.
Consultation closed on a very poorly designed new regulatory regime the week before.
But the big news came at end of the week when the Fair Work Commission handed down a further determination on what aged-care workers should be paid, confirming and going beyond a previous interim determination.
What did the Fair Work Commission find?
Essentially, the commission determined that work in industries with a high proportion of women workers has been traditionally undervalued in wage-setting. This had consequences for both care workers in the aged-care industry (nurses and Certificate III-qualified personal-care workers) and indirect care workers (cleaners, food services assistants).
Aged-care staff will now get significant pay increases – 18–28% increase for personal care workers employed under the Aged Care Award, inclusive of the increase awarded in the interim decision.

Shutterstock/Toa55
Indirect care workers were awarded a general increase of 3%. Laundry hands, cleaners and food services assistants will receive a further 3.96% on the grounds they “interact with residents significantly more regularly than other indirect care employees”.
The final increases for registered and enrolled nurses will be determined in the next few months.
How has the sector responded?
There has been no push-back from employer groups or conservative politicians. This suggests the uplift is accepted as fair by all concerned.
The interim increases of up to 15% probably facilitated this acceptance, with the recognition of the community that care workers should be paid more than fast food workers.
There was no criticism from aged-care providers either. This is probably because they are facing difficulty in recruiting staff at current wage rates. And because government payments to providers reflect the actual cost of aged care, increased payments will automatically flow to providers.
When the increases will flow has yet to be determined. The government is due to give its recommendations for staging implementation by mid-April.
Is the workforce problem fixed?
An increase in wages is necessary, but alone is not sufficient to solve workforce shortages.
The health- and social-care workforce is predicted to grow faster than any other sector over the next decade. The “care economy” will grow from around 8% to around 15% of GDP over the next 40 years.
This means a greater proportion of school-leavers will need to be attracted to the aged-care sector. Aged care will also need to attract and retrain workers displaced from industries in decline and attract suitably skilled migrants and refugees with appropriate language skills.

nastya_ph/Shutterstock
The caps on university and college enrolments imposed by the previous government, coupled with weak student demand for places in key professions (such as nursing), has meant workforce shortages will continue for a few more years, despite the allure of increased wages.
A significant increase in intakes into university and vocational education college courses preparing students for health and social care is still required. Better pay will help to increase student demand, but funding to expand place numbers will ensure there are enough qualified staff for the aged-care system of the future.
Stephen Duckett, Honorary Enterprise Professor, School of Population and Global Health, and Department of General Practice and Primary Care, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 8 Fruits That Prevent & Kill Cancer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Amy Dee, pharmacist and cancer survivor herself, lays out the best options for anticancer fruits:
The fruits
Without further ado, they are:
- Kiwi: promotes cancer cell death while sparing healthy cells
- Plums & peaches: an interesting choice to list these similar fruits together as one item, but they both also induce cell death in cancer cells while sparing healthy ones
- Dragon fruit: this does the same, while also inhibiting cancer cell growth
- Figs: these have antitumor effects specifically, while removing carcinogens too, and additionally sensitizing cancer cells to light therapy
- Cranberries: disrupt cancer cell adhesion, breaking down tumors, while protecting non-cancerous cells against DNA damage
- Citrus fruits: inhibit tumor growth and kill cancer cells; regular consumption is also associated with a lower cancer risk (be warned though, grapefruit interacts with some medications)
- Cherries: induce cancer cell death; protect healthy cells against DNA damage
- Tomatoes: don’t often make it into lists of fruits, but lycopene reduces cancer risk, and slows the growth of cancer cells (10almonds note: watermelon has more lycopene than tomatoes, and is more traditionally considered a fruit in all respects, so could have taken the spot here).
We would also argue that apricots could have had a spot on the list, both for their lycopene content (comparable to tomatoes) and their botanical (and thus phytochemical) similarities to peaches and plums.
For more information on each of these (she also talks about the different polyphenols and other nutrients that constitute the active compounds delivering these anticancer effects), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Food Choice & Cancer Risk: Eat To Beat Cancer
- Beat Cancer Kitchen: Deliciously Simple Plant-Based Anticancer Recipes (book)
Take care!
Share This Post
-
Get Fitter As You Go
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Jaime Seeman: Hard To Kill?
This is Dr. Jaime Seeman. She’s a board-certified obstetrician-gynecologist with a background in nutrition, exercise, and health science. She’s also a Fellow in Integrative Medicine, and a board-certified nutrition specialist.
However, her biggest focus is preventative medicine.
What does she want us to know?
The Five Pillars of being “Hard to Kill”!
As an athlete when she was younger, she got away with poor nutrition habits with good exercise, but pregnancy (thrice) brought her poor thyroid function, other hormonal imbalances, and pre-diabetes.
So, she set about getting better—not something the general medical establishment focuses on a lot! Doctors are pressured to manage symptoms, but are under no expectation to actually help people get better.
So, what are her five pillars?
Nutrition
Dr. Seeman unsurprisingly recommends a whole-foods diet with lots of plants, but unlike many plant-enjoyers, she is also an enjoyer of the ketogenic diet.
While keto-enthusiasts say “carbs are bad” and vegans say “meat is bad”, the reality is: both of those things can be bad, and in both cases, avoiding the most harmful varieties is a very good first step:
Movement
This is in two parts:
- get your 150 minutes of moderate exercise per week
- keep your body mobile!
See also:
Sleep
This one’s quite straightforward, and Dr. Seeman uncontroversially recommends getting 7–9 hours per night; yes, even you:
Mindset
This is key to Dr. Seeman’s approach, and it is about not settling for average, because the average is undernourished, overmedicated, sedentary, and suffering.
She encourages us all to keep working for better health, wherever we’re at. To not “go gentle into that good night”, to get stronger whatever our age, to showcase increasingly robust vitality as we go.
To believe we can, and then to do it.
Environment
That previous item usually won’t last beyond a 10-day health-kick without the correct environment.
As for how to make sure we have that? Check out:
Want more?
She does offer coaching:
Hard To Kill Academy: Master The Mindset To Maximize Your Years
Take care!
Share This Post
-
At The Heart Of Women’s Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A woman’s heart is a particular thing
For the longest time (and still to a large degree now), “women’s health” is assumed to refer to the health of organs found under a bikini. But there’s a lot more to it than that. We are whole people, with such things as brains and hearts and more.
Today (Valentine’s Day!) we’re focusing on the heart.
A quick recap:
We’ve talked previously about some of these sex differences when it comes to the heart, for example:
Heart Attack: His & Hers (Be Prepared!)
…but that’s fairly common knowledge at least amongst those who are attentive to such things, whereas…
…is much less common knowledge, especially with the ways statins are more likely to make things worse for a lot of women (not all though; see the article for some nuance about that).
We also talked about:
What Menopause Does To The Heart
…which is well worth reading too!
A question:
Why are women twice as likely to die from a heart attack as their age-equivalent male peers? Women develop heart disease later, but die from it sooner. Why is that?
That’s been a question scientists have been asking (and tentatively answering, as scientists do—hypotheses, theories, conclusions even sometimes) for 20 years now. Likely contributing factors include:
- A lack of public knowledge of the different symptoms
- A lack of confidence of bystanders to perform CPR on a woman
- A lack of public knowledge (including amongst prescribers) about the sex-related differences for statins
- A lack of women in cardiology, comparatively.
- A lack of attention to it, simply. Men get heart disease earlier, so it’s thought of as a “man thing”, by health providers as much as by individuals. Men get more regular cardiovascular check-ups, women get a mammogram and go.
Statistically, women are much more likely to die from heart disease than breast cancer:
- Breast cancer kills around 0.02% of us.
- Heart disease kills one in three.
And yet…
❝In a nationwide survey, only 22% of primary care doctors and 42% of cardiologists said they feel extremely well prepared to assess cardiovascular risks in women.
We are lagging in implementing risk prevention guidelines for women.
A lot of women are being told to just watch their cholesterol levels and see their doctor in a year. That’s a year of delayed care.❞
Source: The slowly evolving truth about heart disease and women
(there’s a lot more in that article than we have room for in ours, so do check it out!)
Some good news:
The “bystanders less likely to feel confident performing CPR on a woman” aspect may be helped by the deployment of new automatic external defibrillator, that works from four sides instead of one.
It’s called “double sequential external defibrillation”, and you can learn about it here:
A new emergency procedure for cardiac arrests aims to save more lives—here’s how it works
(it’s in use already in Canada and Aotearoa)
Gentlemen-readers, thank you for your attention to this one even if it was mostly not about you! Maybe someone you love will benefit from being aware of this
On a lighter note…
Since it’s Valentine’s Day, a little more on affairs of the heart…
Is chocolate good for the heart? And is it really an aphrodisiac?
We answered these questions and more in our previous main feature:
Chocolate & Health: Fact or Fiction?
Enjoy!
Share This Post
Related Posts
-
The Herbal Supplement That Rivals Prozac
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Flower Power: St. John’s Wort’s Drug-Level Effectiveness
St. John’s wort is a small yellow flower, extract of which can be bought inexpensively off-the-shelf in pretty much any pharmacy in most places.
It’s sold and used as a herbal mood-brightener.
Does it work?
Yes! It’s actually very effective. This is really uncontroversial, so we’ll keep it brief.
The main findings of studies are that St. John’s wort not only gives significant benefits over placebo, but also works about as well as prescription anti-depressants:
A systematic review of St. John’s wort for major depressive disorder
They also found that fewer people stop taking it, compared to how many stop taking antidepressants. It’s not known how much of this is because of its inexpensive, freely-accessible nature, and how much might be because it gave them fewer adverse side effects:
Clinical use of Hypericum perforatum (St John’s wort) in depression: A meta-analysis
How does it work?
First and foremost, it’s an SSRI—a selective serotonin reuptake inhibitor. Basically, it doesn’t add serotonin, but it makes whatever serotonin you have, last longer. Same as most prescription antidepressants. It also affects adenosine and GABA pathways, which in lay terms, means it promotes feelings of relaxation, in a similar way to many prescription antianxiety medications.
Mechanism of action of St John’s wort in depression: what is known?
Any problems we should know about?
Yes, definitely. To quote directly from the National Center for Complementary and Integrative Health:
St. John’s wort can weaken the effects of many medicines, including crucially important medicines such as:
- Antidepressants
- Birth control pills
- Cyclosporine, which prevents the body from rejecting transplanted organs
- Some heart medications, including digoxin and ivabradine
- Some HIV drugs, including indinavir and nevirapine
- Some cancer medications, including irinotecan and imatinib
- Warfarin, an anticoagulant (blood thinner)
- Certain statins, including simvastatin
I’ve read all that, and want to try it!
As ever, we don’t sell it (or anything else), but here’s an example product on Amazon.
Please be safe and do check with your doctor and/or pharmacist, though!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The S.T.E.P.S. To A Healthier Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stepping Into Better Heart Health
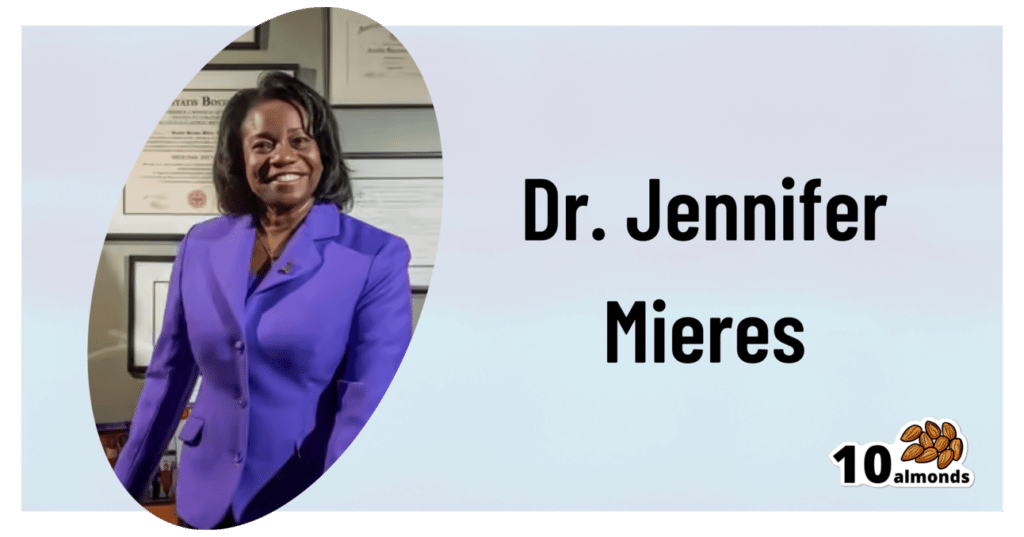
This is Dr. Jennifer H. Mieres, FACC, FAHA, MASNC. she’s an award-winning (we counted 9 major awards) professor of cardiology, and a leading advocate for women’s heart health. This latter she’s done via >70 scientific publications, >100 research presentations at national and international conferences, 3 books so far, and 4 documentaries, including the Emmy-nominated “A Woman’s Heart”.
What does she want us to know?
A lot of her work is a top-down approach, working to revolutionize the field of cardiology in its application, to result in far fewer deaths annually. Which is fascinating, but unless you’re well-placed in that industry, not something too actionable as an individual (if you are well-placed in that industry, do look her up, of course).
For the rest of us…
Dr. Mieres’ S.T.E.P.S. to good heart health
She wants us to do the following things:
1) Stock your kitchen with heart health in mind
This is tied to the third item in the list of course, but it’s a critical step not to be overlooked. It’s all very well to know “eat more fiber; eat less red meat” and so forth, but if you go to your kitchen and what’s there is not conducive to heart health, you’re just going to do the best with what’s available.
Instead, actually buy foods that are high in fiber, and preferably, foods that you like. Not a fan of beans? Don’t buy them. Love pasta? Go wholegrain. Like leafy greens in principle, but they don’t go with what you cook? Look up some recipes, and then buy them.
Love a beef steak? Well we won’t lie to you, that is not good for your heart, but make it a rare option—so to speak—and enjoy it mindfully (see also: mindful eating) once in a blue moon for a special occasion, rather than “I don’t know what to cook tonight, so sizzle sizzle I guess”.
Meal planning goes a long way for this one! And if meal-planning sounds like an overwhelming project to take on, then consider trying one of the many healthy-eating meal kit services that will deliver ingredients (and their recipes) to your door—opting for a plants-forward plan, and the rest should fall into place.
2) Take control of your activity
Choose to move! Rather than focusing on what you can’t do (let’s say, those 5am runs, or your regularly-scheduled, irregularly attended, gym sessions), focus on what you can do, and do it.
See also: No-Exercise Exercise!
3) Eat for a healthier heart
This means following through on what you did on the first step, and keeping it that way. Buying fresh fruit and veg is great, but you also have to actually eat it. Do not let the perishables perish!
For you too, dear reader, are perishable (and would presumably like to avoid perishing).
This item in the list may seem flippant, but actually this is about habit-forming, and without it, the whole plan will grind to a halt a few days after your first heart-health-focused shopping trip.
See also: Where Nutrition Meets Habits!
4) Partner with your doctor, family, and friends
Good relationships, both professional and personal, count for a lot. Draw up a plan with your doctor; don’t just guess at when to get this or that checked—or what to do about it if the numbers aren’t to your liking.
Partnership with your doctor goes both ways, incidentally. Read up, have opinions, discuss them! Doing so will ultimately result in better care than just going in blind and coming out with a recommendation you don’t understand and just trust (but soon forget, because you didn’t understand).
And as for family and friends, this is partly about social factors—we tend to influence, and be influenced by, those around us. It can be tricky to be on a health kick if your partner wants take-out every night, so some manner of getting everyone on the same page is important, be it by compromise or, in an ideal world, gradually trending towards better health. But any such changes must come from a place of genuine understanding and volition, otherwise at best they won’t stick, and at worst they’ll actively create a pushback.
Same goes for exercise as for diet—exercising together is a good way to boost commitment, especially if it’s something fun (dance classes are a fine example that many couples enjoy, for example).
5) Sleep more, stress less, savor life
These things matter a lot! Many people focus on cutting down salt or saturated fat, and that can be good if otherwise consumed to excess, but for most people they’re not the most decisive factors:
Hypertension: Factors Far More Relevant Than Salt ← sleep features here!
Stress is also a huge one, and let’s put it this way: people more often have heart attacks during a moment of excessive emotional stress—not during a moment when they had a bit too much butter on their toast.
It’s not even just that acute stress is the trigger, it’s that chronic stress is a contributory factor that erodes the body’s ability to handle the acute stress.
Changing this may seem “easier said than done” because often the stressors are external (e.g. work pressure, financial worries, caring for a sick relative, relationship troubles, major life change, etc), but it is possible to find peace even in the chaos of life:
Want to know more from Dr. Mieres?
You might like this book of hers, which goes into each of the above items in much more depth than we have room to here:
Heart Smarter for Women: Six Weeks to a Healthier Heart – by Dr. Jennifer Mieres
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- the leaky blood vessels are breaching the blood-brain-barrier