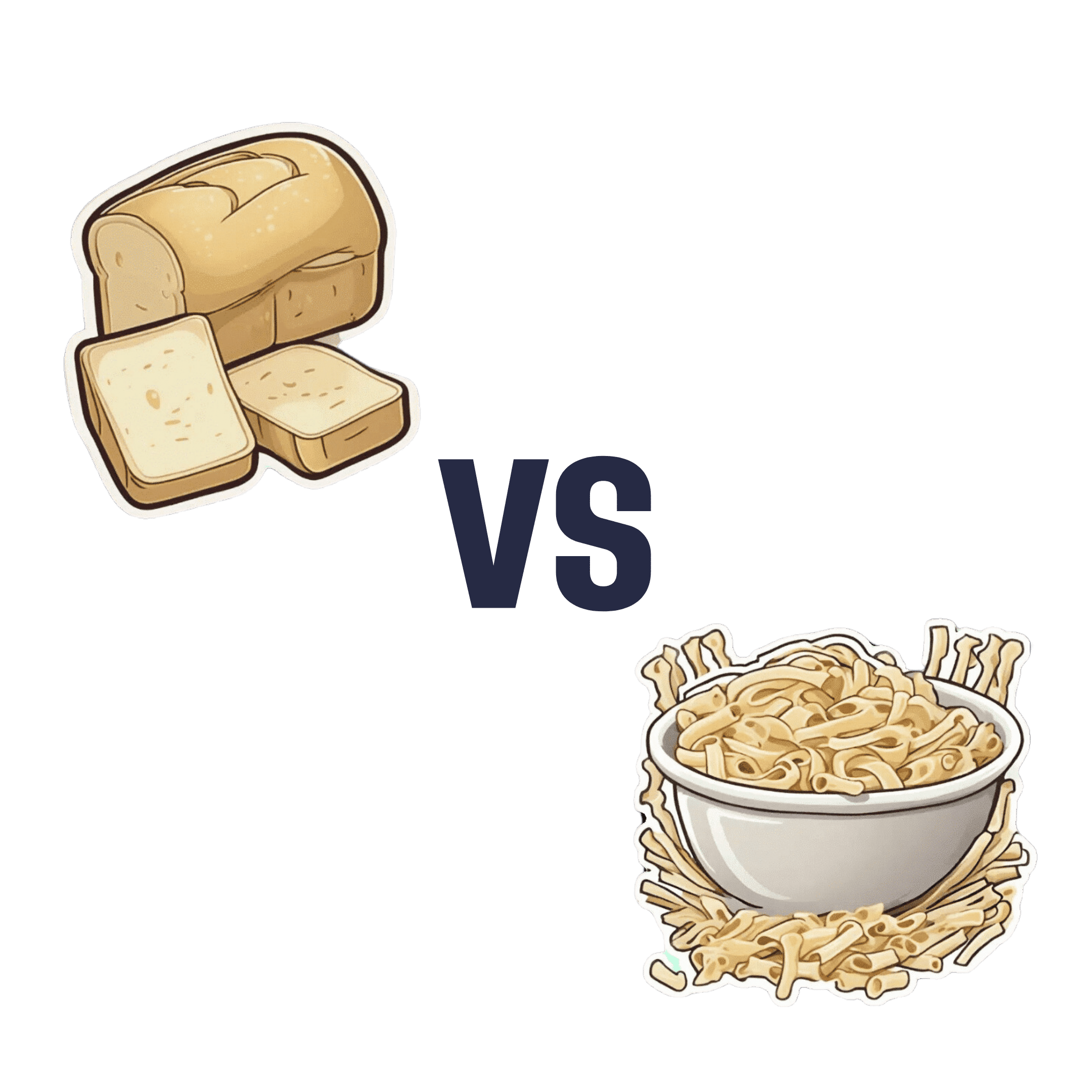
White Bread vs White Pasta – Which Is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing a white bread to a white pasta, we picked the pasta.
Why?
Neither are great for the health! But like for like, the glycemic index of the bread is usually around 150% of the glycemic index for pasta.
All that said, we heartily recommend going for wholegrain in either case!
Bonus tip: cooking pasta “al dente”, so it is still at least a little firm to the bite, results in a lower GI compared to being boiled to death.
Bonus bonus tip: letting pasta cool increases resistant starches. You can then reheat the pasta without losing this benefit.
Please don’t put it in the microwave though; you will make an Italian cry. Instead, simply put it in a colander and pour boiling water over it, and then serve in your usual manner (a good approach if serving it separately is: put it in the serving bowl/dish/pan, drizzle a little extra virgin olive oil and a little cracked black pepper, stir to mix those in, and serve)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Brain Health Kitchen – by Dr. Annie Fenn
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a cookbook built around the MIND diet, which we talked about in our “Four Ways To Upgrade The Mediterranean Diet” article.
As such, it’s a top-tier gold-standard diet to be following for brain health, and having it as a book of recipes makes actually eating this way a lot easier!
The book does talk about the science first before getting to the recipes, so don’t worry, you won’t have to reverse engineer the dietary guidelines from the recipes; everything is explained well.
The recipes (of which there are 100) are diverse enough to be interesting without being so complicated as to be difficult. The ingredients are largely nutritional powerhouses, and most if not all can be found in your nearest reasonable-sized supermarket. Also, the recipes are (as you might reasonably expect), very plant-forward, but not entirely plant-based (as you might have guessed from the salmon on the front cover).
Bottom line: if you’d like to eat more healthily for your brain, but are a little stumped on what to do with the four ingredients you remember are brain-healthy, this book will help expand your horizons—not to mention your culinary repertoire!
Share This Post
-
The Pain-Free Mindset – by Dr. Deepak Ravindran
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First: please ignore the terrible title. This is not the medical equivalent of “think and grow rich”. A better title would have been something like “The Pain-Free Plan”.
Attentive subscribers may notice that this author was our featured expert yesterday, so you can learn about his “seven steps” described in our article there, without us repeating that in our review here.
This book’s greatest strength is also potentially its greatest weakness, depending on the reader: it contains a lot of detailed medical information.
This is good or bad depending on whether you like lots of detailed medical information. Dr. Ravindran doesn’t assume prior knowledge, so everything is explained as we go. However, this means that after his well-referenced clinical explanations, high quality medical diagrams, etc, you may come out of this book feeling like you’ve just done a semester at medical school.
Knowledge is power, though, so understanding the underlying processes of pain and pain management really does help the reader become a more informed expert on your own pain—and options for reducing that pain.
Bottom line: this, disguised by its cover as a “think healing thoughts” book, is actually a science-centric, information-dense, well-sourced, comprehensive guide to pain management from one of the leading lights in the field.
Click here to check out The Pain-Free Mindset, and manage yours more comfortably!
Share This Post
-
Which B Vitamins? It Makes A Difference
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Everyone knows “B vitamins are for energy!” and that is definitely a theme, but there’s a lot more to it than that, and in some cases, there are big mistakes that people make when it comes to supplementing their diet.
First, let’s do a quick overview of what each of the B vitamins do, by number, and putting names to them:
B1 (Thiamine)
- Function: helps convert carbohydrates into energy, supports nerve function
- Forms: thiamine hydrochloride, thiamine mononitrate, benfotiamine (fat-soluble form)
- Example foods: lentils, sunflower seeds
B2 (Riboflavin)
- Function: supports energy production, skin health, and eye function, turns your pee fluorescent yellow (the latter is really only if you consume exciting amounts of it; this will usually occur from supplementation, not from normal diet)
- Forms: riboflavin, riboflavin-5’-phosphate
- Example foods: almonds, mushrooms
B3 (Niacin)
- Function: aids metabolism, supports skin, nerves, and cholesterol levels
- Forms: niacin (nicotinic acid), niacinamide (nicotinamide), inositol hexanicotinate (flush-free niacin)
- Example foods: whole grains, peanuts (literally the best nut for this)
B5 (Pantothenic Acid)
- Function: essential for fatty acid metabolism and hormone production
- Forms: pantothenic acid, calcium pantothenate, panthenol (alcohol form!)
- Example foods: it’s in pretty much everything (hence the name); it’s almost impossible to be deficient in this vitamin unless you are literally starving
B6 (Pyridoxine)
- Function: needed for red blood cell production, supports brain function, as well as specifically being a part of neurotransmitter production (including dopamine and serotonin, despite them being made in different places—the brain and the gut, respectively),
- Forms: pyridoxine hydrochloride, pyridoxal-5’-phosphate (active form)
- Example foods: bananas, potatoes
B7 (Biotin)
- Function: helps with fatty acid synthesis, skin, hair, and nail health
- Forms: d-biotin, biotinylated compounds of various kinds
- Example foods: fava beans, walnuts
B9 (Folate/Folic Acid)
- Function: crucial for DNA synthesis, cell division, and fetal development
- Forms: folic acid, folinic acid, 5-methyltetrahydrofolate (5-MTHF, active form)
- Example foods: chickpeas, spinach ← we only mentioned one leafy green here for fairness, but leafy greens in general are great sources of vitamin B9, hence the name, from the Latin “folium”, meaning leaf.
B12 (Cobalamin)
- Function: supports red blood cell formation, nerve function, and DNA synthesis
- Forms: cyanocobalamin, methylcobalamin (active), hydroxocobalamin (active), adenosylcobalamin (active)
- Example foods: nutritional yeast, nori
You may be wondering: what about vitamins B4, B8, B10, and B11? Those are now vacant spots, that once contained things that are no longer considered vitamins.
Three Critical Vitamin B Mistakes That May Be Sabotaging Your Health
Some mistakes that people make include:
Not supplementing when necessary
This occurs most often after midlife, especially in women, and the most common deficiencies are B1, B9, and B12.
See also: These Signs Often Mean These Nutrient Deficiencies (Do You Have Any?)
While it’s tempting to think “if I have a good balanced diet, I won’t need…” but the fact is sometimes our diet isn’t as nutrient dense as we hope—often through no fault of our own! But many modern farming methods prioritize yield over nutritional value, and that can result in plants and animals that do not have the nutritional qualities they “should”.
We wrote about this a while back, weighing up the “supplementation vs diet alone” dilemma:
Does Our Diet Need A Little Help? ← this also has a very useful chart of which vitamins people usually get too little or too much of. Note however that the statement of marginally excessive folate is slightly misleading, as the data pool contains men and women aged 18–65, while B9 is mostly needed more by women, and especially around childbirth or menopause, so B9 is actually a very common deficiency, but here it’s being balanced out lots of men getting too much (because every multivitamin has it).
Supplementing to excess
Most B vitamins have a very high maximum tolerable dose, because (with the exception of where we marked otherwise) they are water-soluble, which means that if you take more than you need, you’ll just pee it out later. Hence the famous fluorescence, for example.
However, the fat soluble form of vitamin B1 is harder to get in and harder to get out.
As for the others, problems usually only occur if you take enough to cause toxicity, faster than you pee it out. In other words, go easy on those Berocca drinks!
Nevertheless, there are other problems that can arise:
Vitamin B6 is essential—but too much can be toxic. Here’s what to know to stay safe ← tl;dr: there are issues with it causing peripheral neuropathy at doses over 10mg (the safe dose is disputed, so we’re mentioning the lowest safe dose here, but you can read about the others in the article)
Getting forms that don’t work so well
Those different forms we listed? They are not all created equal! For example:
- Folic acid is cheap; unfortunately, it’s not absorbed or used well
- Cyanocobalamin is cheap; unfortunately, it’s not absorbed or used well
Let us quote a recent book review of ours:
❝Rather, the most common forms of vitamins B9 and B12 provided in supplements are folic acid and cyanocobalamin, respectively, which as he demonstrates with extensive research to back up his claims, cannot be easily absorbed or used especially well.
About those vitamers: a vitamer is simply a form of a vitamin—most vitamins we need can arrive in a variety of forms. In the case of vitamins B9 and B12, he advocates for ditching vitamers folic acid and cyanocobalamin, cheap as they are, and springing for bioactive vitamers L-methylfolate, methylcobalamin, and adenosylcobalamin.
He also discusses (again, just as well-evidenced as the above things) why we might struggle to get enough from our diet after a certain age. For example, if trying to get these vitamins from meat, 50% of people over 50 cannot manufacture enough stomach acid to break down that protein to release the vitamins.
And as for methyl-B12 vitamers, you might expect you can get those from meat, and technically you can, but they don’t occur in all animals, just in one kind of animal. Specifically, the kind that has the largest brain-to-body ratio. However, eating the meat of this animal can result in protein folding errors in general and Creutzfeldt–Jakob disease in particular, so the author does not recommend eating humans, however nutritionally convenient that would be.
All this means that supplementation after a certain age really can be a sensible way to do it—but do it wisely, and pick the right vitamers.❞
You can read that review in full here: Your Vitamins are Obsolete: The Vitamer Revolution – by Dr. Sheldon Zablow
Want to try those latter two?
We don’t sell them, but here for your convenience are example products on Amazon:
L-methylfolate (active form of vitamin B9)
Methylcobalamin, adenosylcobalamin, & hydroxocobalamin (active forms of vitamin B12)
Take care!
Share This Post
Related Posts
-
Why do I keep getting urinary tract infections? And why are chronic UTIs so hard to treat?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dealing with chronic urinary tract infections (UTIs) means facing more than the occasional discomfort. It’s like being on a never ending battlefield against an unseen adversary, making simple daily activities a trial.
UTIs happen when bacteria sneak into the urinary system, causing pain and frequent trips to the bathroom.
Chronic UTIs take this to the next level, coming back repeatedly or never fully going away despite treatment. Chronic UTIs are typically diagnosed when a person experiences two or more infections within six months or three or more within a year.
They can happen to anyone, but some are more prone due to their body’s makeup or habits. Women are more likely to get UTIs than men, due to their shorter urethra and hormonal changes during menopause that can decrease the protective lining of the urinary tract. Sexually active people are also at greater risk, as bacteria can be transferred around the area.
Up to 60% of women will have at least one UTI in their lifetime. While effective treatments exist, about 25% of women face recurrent infections within six months. Around 20–30% of UTIs don’t respond to standard antibiotic. The challenge of chronic UTIs lies in bacteria’s ability to shield themselves against treatments.
Why are chronic UTIs so hard to treat?
Once thought of as straightforward infections cured by antibiotics, we now know chronic UTIs are complex. The cunning nature of the bacteria responsible for the condition allows them to hide in bladder walls, out of antibiotics’ reach.
The bacteria form biofilms, a kind of protective barrier that makes them nearly impervious to standard antibiotic treatments.
This ability to evade treatment has led to a troubling increase in antibiotic resistance, a global health concern that renders some of the conventional treatments ineffective.
Some antibiotics no longer work against UTIs.
Michael Ebardt/ShutterstockAntibiotics need to be advanced to keep up with evolving bacteria, in a similar way to the flu vaccine, which is updated annually to combat the latest strains of the flu virus. If we used the same flu vaccine year after year, its effectiveness would wane, just as overused antibiotics lose their power against bacteria that have adapted.
But fighting bacteria that resist antibiotics is much tougher than updating the flu vaccine. Bacteria change in ways that are harder to predict, making it more challenging to create new, effective antibiotics. It’s like a never-ending game where the bacteria are always one step ahead.
Treating chronic UTIs still relies heavily on antibiotics, but doctors are getting crafty, changing up medications or prescribing low doses over a longer time to outwit the bacteria.
Doctors are also placing a greater emphasis on thorough diagnostics to accurately identify chronic UTIs from the outset. By asking detailed questions about the duration and frequency of symptoms, health-care providers can better distinguish between isolated UTI episodes and chronic conditions.
The approach to initial treatment can significantly influence the likelihood of a UTI becoming chronic. Early, targeted therapy, based on the specific bacteria causing the infection and its antibiotic sensitivity, may reduce the risk of recurrence.
For post-menopausal women, estrogen therapy has shown promise in reducing the risk of recurrent UTIs. After menopause, the decrease in estrogen levels can lead to changes in the urinary tract that makes it more susceptible to infections. This treatment restores the balance of the vaginal and urinary tract environments, making it less likely for UTIs to occur.
Lifestyle changes, such as drinking more water and practising good hygiene like washing hands with soap after going to the toilet and the recommended front-to-back wiping for women, also play a big role.
Some swear by cranberry juice or supplements, though researchers are still figuring out how effective these remedies truly are.
What treatments might we see in the future?
Scientists are currently working on new treatments for chronic UTIs. One promising avenue is the development of vaccines aimed at preventing UTIs altogether, much like flu shots prepare our immune system to fend off the flu.
Emerging treatments could help clear chronic UTIs.
guys_who_shoot/ShutterstockAnother new method being looked at is called phage therapy. It uses special viruses called bacteriophages that go after and kill only the bad bacteria causing UTIs, while leaving the good bacteria in our body alone. This way, it doesn’t make the bacteria resistant to treatment, which is a big plus.
Researchers are also exploring the potential of probiotics. Probiotics introduce beneficial bacteria into the urinary tract to out-compete harmful pathogens. These good bacteria work by occupying space and resources in the urinary tract, making it harder for harmful pathogens to establish themselves.
Probiotics can also produce substances that inhibit the growth of harmful bacteria and enhance the body’s immune response.
Chronic UTIs represent a stubborn challenge, but with a mix of current treatments and promising research, we’re getting closer to a day when chronic UTIs are a thing of the past.
Iris Lim, Assistant Professor, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Intuitive Eating – by Evelyn Tribole and Elyse Resch
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You may be given to wonder: if this is about intuitive eating, and an anti-diet approach, why a whole book?
There’s a clue in the other part of the title: “4th Edition”.
The reason there’s a 4th edition (and before it, a 3rd and 2nd edition) is because this book is very much full of science, and science begets more science, and the evidence just keeps on rolling in.
While neither author is a doctor, each has a sizeable portion of the alphabet after their name (more than a lot of doctors), and this is an incredibly well-evidenced book.
The basic premise from many studies is that restrictive dieting does not work well long-term for most people, and instead, better is to make use of our bodies’ own interoceptive feedback.
You see, intuitive eating is not “eat randomly”. We do not call a person “intuitive” because they speak or act randomly, do we? Same with diet.
Instead, the authors give us ten guiding principles (yes, still following the science) to allow us a consistent “finger on the pulse” of what our body has to say about what we have been eating, and what we should be eating.
Bottom line: if you want to be a lot more in tune with your body and thus better able to nourish it the way it needs, this book is literally on the syllabus for many nutritional science classes, and will stand you in very good stead!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Princess of Wales wants to stay cancer-free. What does this mean?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Catherine, Princess of Wales, has announced she has now completed a course of preventive chemotherapy.
The news comes nine months after the princess first revealed she was being treated for an unspecified form of cancer.
In the new video message released by Kensington Palace, Princess Catherine says she’s focused on doing what she can to stay “cancer-free”. She acknowledges her cancer journey is not over and the “path to recovery and healing is long”.
While we don’t know the details of the princess’s cancer or treatment, it raises some questions about how we declare someone fully clear of the disease. So what does being – and staying – “cancer-free” mean?
Pete Hancock/Shutterstock What’s the difference between being cancer-free and in remission?
Medically, “cancer-free” means two things. First, it means no cancer cells are able to be detected in a patient’s body using the available testing methods. Second, there is no cancer left in the patient.
These might sound basically the same. But this second aspect of “cancer-free” can be complicated, as it’s essentially impossible to be sure no cancer cells have survived a treatment.
Testing can’t completely rule out the chance some cancer cells have survived treatment. Andrewshots/Shutterstock It only takes a few surviving cells for the cancer to grow back. But these cells may not be detectable via testing, and can lie dormant for some time. The possibility of some cells still surviving means it is more accurate to say a patient is “in remission”, rather than “cancer-free”.
Remission means there is no detectable cancer left. Once a patient has been in remission for a certain period of time, they are often considered to be fully “cancer-free”.
Princess Catherine was not necessarily speaking in the strict medical sense. Nonetheless, she is clearly signalling a promising step in her recovery.
What happens during remission?
During remission, patients will usually undergo surveillance testing to make sure their cancer hasn’t returned. Detection tests can vary greatly depending on both the patient and their cancer type.
Many tests involve simply looking at different organs to see if there are cancer cells present, but at varying levels of complexity.
Some cancers can be detected with the naked eye, such as skin cancers. In other cases, technology is needed: colonoscopies for colorectal cancers, X-ray mammograms for breast cancers, or CT scans for lung cancers. There are also molecular tests, which test for the presence of cancer cells using protein or DNA from blood or tissue samples.
For most patients, testing will continue for years at regular intervals. Surveillance testing ensures any returning cancer is caught early, giving patients the best chance of successful treatment.
Remaining in remission for five years can be a huge milestone in a patient’s cancer journey. For most types of cancer, the chances of cancer returning drop significantly after five years of remission. After this point, surveillance testing may be performed less frequently, as the patients might be deemed to be at a lower risk of their cancer returning.
Skin cancer may be detected by the naked eye, but many other cancers require technology for detection and monitoring. wavebreakmedia/Shutterstock Measuring survival rates
Because it is very difficult to tell when a cancer is “cured”, clinicians may instead refer to a “five-year survival rate”. This measures how likely a cancer patient is to be alive five years after their diagnosis.
For example, data shows the five-year survival rate for bowel cancer among Australian women (of all ages) is around 70%. That means if you had 100 patients with bowel cancer, after five years you would expect 70 to still be alive and 30 to have succumbed to the disease.
These statistics can’t tell us much about individual cases. But comparing five-year survival rates between large groups of patients after different cancer treatments can help clinicians make the often complex decisions about how best to treat their patients.
The likelihood of cancer coming back, or recurring, is influenced by many factors which can vary over time. For instance, approximately 30% of people with lung cancer develop a recurrent disease, even after treatment. On the other hand, breast cancer recurrence within two years of the initial diagnosis is approximately 15%. Within five years it drops to 10%. After ten, it falls below 2%.
These are generalisations though – recurrence rates can vary greatly depending on things such as what kind of cancer the patient has, how advanced it is, and whether it has spread.
Staying cancer-free
Princess Catherine says her focus now is to “stay cancer-free”. What might this involve?
How a cancer develops and whether it recurs can be influenced by things we can’t control, such as age, ethnicity, gender, genetics and hormones.
However, there are sometimes environmental factors we can control. That includes things like exposure to UV radiation from the sun, or inhaling carcinogens like tobacco.
Lifestyle factors also play a role. Poor diet and nutrition, a lack of exercise and excessive alcohol consumption can all contribute to cancer development.
Research estimates more than half of all cancers could potentially be prevented through regular screening and maintaining a healthy lifestyle (not to mention preventing other chronic conditions such as heart disease and diabetes).
Recommendations to reduce cancer risk are the same for everyone, not just those who’ve had treatment like Princess Catherine. They include not smoking, eating a nutritious and balanced diet, exercising regularly, cutting down on alcohol and staying sun smart.
Amali Cooray, PhD Candidate in Genetic Engineering and Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research) ; John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research) , and Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: