When supplies resume, should governments subsidise drugs like Ozempic for weight loss? We asked 5 experts
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hundreds of thousands of people worldwide are taking drugs like Ozempic to lose weight. But what do we actually know about them? This month, The Conversation’s experts explore their rise, impact and potential consequences.
You’ve no doubt heard of Ozempic but have you heard of Wegovy? They’re both brand names of the drug semaglutide, which is currently in short supply worldwide.
Ozempic is a lower dose of semaglutide, and is approved and used to treat diabetes in Australia. Wegovovy is approved to treat obesity but is not yet available in Australia. Shortages of both drugs are expected to last throughout 2024.
Both drugs are expensive. But Ozempic is listed on Australia’s Pharmaceutical Benefits Schedule (PBS), so people with diabetes can get a three-week supply for A$31.60 ($7.70 for concession card holders) rather than the full price ($133.80).
Wegovy isn’t listed on the PBS to treat obesity, meaning when it becomes available, users will need to pay the full price. But should the government subsidise it?
Wegovy’s manufacturer will need to make the case for it to be added to the PBS to an independent advisory committee. The company will need to show Wegovy is a safe, clinically effective and cost-effective treatment for obesity compared to existing alternatives.
In the meantime, we asked five experts: when supplies resume, should governments subsidise drugs like Ozempic for weight loss?
Four out of five said yes
This is the last article in The Conversation’s Ozempic series. Read the other articles here.
Disclosure statements: Clare Collins is a National Health and Medical Research Council (NHMRC) Leadership Fellow and has received research grants from the National Health and Medical Research Council (NHMRC), the Australian Research Council (ARC), the Medical Research Future Fund (MRFF), the Hunter Medical Research Institute, Diabetes Australia, Heart Foundation, Bill and Melinda Gates Foundation, nib foundation, Rijk Zwaan Australia, the Western Australian Department of Health, Meat and Livestock Australia, and Greater Charitable Foundation. She has consulted to SHINE Australia, Novo Nordisk (for weight management resources and an obesity advisory group), Quality Bakers, the Sax Institute, Dietitians Australia and the ABC. She was a team member conducting systematic reviews to inform the 2013 Australian Dietary Guidelines update, the Heart Foundation evidence reviews on meat and dietary patterns and current co-chair of the Guidelines Development Advisory Committee for Clinical Practice Guidelines for Treatment of Obesity; Emma Beckett has received funding for research or consulting from Mars Foods, Nutrition Research Australia, NHMRC, ARC, AMP Foundation, Kellogg and the University of Newcastle. She works for FOODiQ Global and is a fat woman. She is/has been a member of committees/working groups related to nutrition or food, including for the Australian Academy of Science, the NHMRC and the Nutrition Society of Australia; Jonathan Karnon does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment; Nial Wheate in the past has received funding from the ACT Cancer Council, Tenovus Scotland, Medical Research Scotland, Scottish Crucible, and the Scottish Universities Life Sciences Alliance. He is a fellow of the Royal Australian Chemical Institute, a member of the Australasian Pharmaceutical Science Association and a member of the Australian Institute of Company Directors. Nial is the chief scientific officer of Vaihea Skincare LLC, a director of SetDose Pty Ltd (a medical device company) and a Standards Australia panel member for sunscreen agents. Nial regularly consults to industry on issues to do with medicine risk assessments, manufacturing, design and testing; Priya Sumithran has received grant funding from external organisations, including the NHMRC and MRFF. She is in the leadership group of the Obesity Collective and co-authored manuscripts with a medical writer provided by Novo Nordisk and Eli Lilly.
Fron Jackson-Webb, Deputy Editor and Senior Health Editor, The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Margarine vs Butter – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing margarine to butter, we picked the butter.
Why?
Once upon a time, when margarines were filled with now-banned trans fats, this would have been an easy win for butter.
Nowadays, the macronutrient/lipid profiles are generally more similar (although margarine often has a little less saturated fat), except one thing that butter has in its favor:
More micronutrients. What exactly they are (and how much) depends on the diet and general health of the cows from whom the milk to make the butter came, but they’re not something found in plant-based butter alternatives at this time.
Nevertheless, because of the saturated fat content, it’s not advisable to use more than a very small amount of either (two tablespoons of butter would put one at the daily limit already, without eating any other saturated fat that day).
Read more: Butter vs Margarine
Share This Post
-
How an Idaho vaccine advocacy org plans its annual goals
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The start of a new year means many nonprofits and community health workers are busy setting goals and reflecting on what’s worked and what hasn’t. For those engaged in vaccine outreach, it also means reflecting on the tools and tactics that help them communicate better with their communities about why vaccines matter.
Across the country, childhood vaccination rates have declined since the COVID-19 pandemic, resulting in a resurgence of preventable diseases like pertussis.
Also known as whooping cough, pertussis has surged in states like Idaho, said Karen Jachimowski Sharpnack, executive director of the Idaho Immunization Coalition, in a conversation with PGN about the organization’s 2025 priorities.
Sharpnack shared how spikes in infectious respiratory illnesses can create opportunities to listen better and understand the nuances of the communities they serve.
Here’s more of what Sharpnack said.
[Editor’s note: The contents of this interview have been edited for length and clarity.]
PGN: Whooping cough cases are up in your state. Can you share an example of how your organization is responding?
Karen Jachimowski Sharpnack: If you look at Treasure Valley and Northern Idaho, the majority of those cases have been reported, and it’s like five times as much as we had the previous year.
So, two things that the Coalition is doing in response: First, we put out radio public service announcements throughout those particular areas about what whooping cough is, how contagious it is, and what you should do if you think your child or anyone you know has it.
Second, we are contacting every school superintendent, principal, school nurse, with a letter from us at the Coalition [to warn about] the whooping cough outbreaks in schools right now. Here’s what the symptoms are, here’s what you can do, and then here’s how you can protect yourself and your families.
It doesn’t mean the health district wouldn’t do it, or the Department of Health and Welfare can’t do it. But from our standpoint, at least we are bringing an awareness to the schools that this is happening.
PGN: How does your organization decide when outreach is needed? How do you take a pulse of your communities’ vaccine attitudes?
K.J.S.: We consistently hold listening sessions. We do them in English and Spanish if we need to, and we go around—and I’m talking about the southern part of the state—and bring people together.
We’ve done adults, we’ve done teenagers, we’ve done college students, we’ve done seniors, we’ve done all age groups.
So, we’ll bring eight or 10 people together, and we’ll spend a couple of hours with them. We feed them and we also pay them to be there. We say, ‘We want to hear from you about what you’re hearing about vaccines, what your views are if you’re vaccinated.’ Anytime, by the way, they can get up and leave and still get paid.
We want to hear what they’re hearing on the ground. And these sessions are extremely informational. For one, we learn about the misinformation that goes out there, like immediately. And two, we’re able to then focus [on how to respond]. If we’re hearing this, what kind of media campaign do we need to get together?
PGN: How do these listening sessions inform your work?
K.J.S.: So, a couple times a year we also pay a professional poller to do a poll. And when we get those results we check them against our listening sessions. We want to see: Are we on target? Are we ahead?
We just finished putting a one-pager together for legislators, so we’re ready to go with the new [legislative] session. We do this poll every year in August-September to know how Idahoans are feeling about vaccines. We get the results in October, because we’re getting ready for the next year.
We actually poll 19-to-64-year-olds, really honing in on questions like, ‘Do you believe vaccines are safe and effective?’ ‘Do you believe that school vaccination rules should still be in place?’
And what’s pretty cool is that two-thirds of Idahoans still believe vaccines are safe and effective, want to keep school rules in place, and believe that the infrastructure systems that we have in place for our vaccine registry should remain the same. Those are important to hear, so this is really good information that we can pull out and do something with.
PGN: Like what?
K.J.S.: Here’s the bottom line. It takes money to do this work, so you have to be able to say what you are going to do with the results.
Doing a poll costs anywhere from $15,000 to $35,000. This is an expensive investment, but we know that the polling is so important to us, along with the time that I have my staff go out and do the listening sessions and get feedback.
We take those results to educate, to talk to our legislators, and advocate for vaccines. We actually do these high-level media campaigns around the state. So, we are actually doing something with the polling. We’re not just sharing the results out.
And then we actually ask, what can we do to make a change? What are we hearing that we need to focus on?
That’s why it’s really important, because we are actually pushing this out for 2025. We know where we’re going in 2025 programmatically with marketing, and we know where we’re going with advocacy work.
We’re not guessing. We’re actually listening to people. And then we’re making really concrete decisions on how we’re going to move the organization forward to be able to help our communities.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Share This Post
-
Hair-Loss Remedies, By Science
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
10almonds Gets Hairy
Hair loss is a thing that at some point affects most men and a large minority of women. It can be a source of considerable dysphoria for both, as it’s often seen as a loss of virility/femininity respectively, and is societally stigmatized in various ways.
Today we’re going to focus on the most common kind: androgenic alopecia, which is called “male pattern baldness” in men and “female pattern baldness” in women, despite being the same thing.
We won’t spend a lot of time on the science of why this happens (we’re going to focus on the remedies instead), but suffice it to say that genes and hormones both play a role, with dihydrogen testosterone (DHT) being the primary villain in this case.
We’ve talked before about the science of 5α-reductase inhibitors to block the conversion of regular testosterone* to DHT, its more potent form:
One Man’s Saw Palmetto Is Another Woman’s Serenoa Repens…
*We all make this to a greater or lesser degree, unless we have had our ovaries/testes removed.
Finasteride
Finasteride is a 5α-reductase inhibitor that performs similarly to saw palmetto, but comes in tiny pills instead of needing to take a much higher dose of supplement (5mg of finasteride is comparable in efficacy to a little over 300mg of saw palmetto).
Does it work? Yes!
Any drawbacks? A few:
- It’ll take 3–6 months to start seeing effects. This is because of the hormonal life-cycle of human hairs.
- Common side-effects include ED.
- It is popularly labelled/prescribed as “only for men”
On that latter point: the warnings about this are severe, detailing how women must not take it, must not even touch it if it has been cut up or crushed.
However… That’s because it can carry a big risk to our unborn fetuses. So, if we are confident we definitely don’t have one of those, it’s not actually applicable to us.
That said, finasteride’s results in women aren’t nearly so clear-cut as in men (though also, there has been less research, largely because of the above). Here’s an interesting breakdown in more words than we have room for here:
Finasteride for Women: Everything You Need to Know
Spironolactone
This one’s generally prescribed to women, not men, largely because it’s the drug sometimes popularly known as a “chemical castration” drug, which isn’t typically great marketing for men (although it can be applied topically, which will have less of an effect on the rest of the body). For women, this risk is simply not an issue.
We’ll be brief on this one, but we’ll just drop this, so that you know it’s an option that works:
❝Spironolactone is an effective and safe treatment of androgenic alopecia which can enhance the efficacy when combined with other conventional treatments such as minoxidil.
Topical spironolactone is safer than oral administration and is suitable for both male and female patients, and is expected to become a common drug for those who do not have a good response to minoxidil❞
Minoxidil
This one is available (to men and women) without prescription. It’s applied topically, and works by shortcutting the hair’s hormonal growth cycle, to reduce the resting phase and kick it into a growth phase.
Does it work? Yes!
Any drawbacks? A few:
- Whereas you’ll remember finasteride takes 3–6 months to see any effect, this one will have an effect very quickly
- Specifically, the immediate effect is: your rate of hair loss will appear to dramatically speed up
- This happens because when hairs are kicked into their growth phase if they were in a resting phase, the first part of that growth phase is to shed each old hair to make room for the new one
- You’ll then need the same 3–6 months as with finasteride, to see the regrowth effects
- If you stop using it, you will immediately shed whatever hair you gained by this method
Why do people choose this over finasteride? For one of three reasons, mainly:
- They are women, and not offered finasteride
- They are men, and do not want the side effects of finasteride
- They just saw an ad and tried it
As to how it works:
Some final notes:
There are some other contraindications and warnings with each of these drugs by the way, so do speak with your doctor/pharmacist. For example:
- Finasteride can tax the liver a little
- Spironolactone can reduce bone turnover
- Minoxidil is a hypotensive; this shouldn’t be an issue for most people, but for some people it could be a problem
There are other hair loss remedies and practices, but the above three are the heavy-hitters, so that’s what we spent our time/space on today. We’ll perhaps cover the less powerful (but less risky) options one of these days.
Meanwhile, take care!
Share This Post
Related Posts
-
The Comfort Book – by Matt Haig
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book “is what it says on the tin”. Matt Haig, bestselling author of “Reasons to Stay Alive” (amongst other works) is here with “a hug in a book”.
The format of the book is an “open it at any page and you’ll find something of value” book. Its small chapters are sometimes a few pages long, but often just a page. Sometimes just a line. Always deep.
All of us, who live long enough, will ponder our mortality sometimes. The feelings we may have might vary on a range from “afraid of dying” to “despairing of living”… but Haig’s single biggest message is that life is full of wonder; each moment precious.
- That hope is an incredible (and renewable!) resource.
- That we are more than a bad week, or month, or year, or decade.
- That when things are taken from us, the things that remain have more value.
Bottom line: you might cry (this reviewer did!), but it’ll make your life the richer for it, and remind you—if ever you need it—the value of your amazing life.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Cashew Nuts vs Macadamia Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cashews to macadamias, we picked the cashews.
Why?
In terms of macros, cashews have more than 2x the protein, while macadamias have nearly 2x the fat. The fats are mostly monounsaturated, so it’s still healthy in moderation, but still, we’re going to prize the protein over it and call this category a nominal win for cashews.
When it comes to vitamins, things are fairly even; cashews have more of vitamins B5, B6, B9, and E, while macadamias have more of vitamins B1, B2, B3, and C.
In the category of minerals, cashews take the clear lead; cashews have more copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while macadamias have more calcium and manganese.
In short, enjoy both (as macadamias have their benefits too), but cashews win in total nutrient density.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How Much Can Hypnotherapy Really Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sit Back, Relax, And…
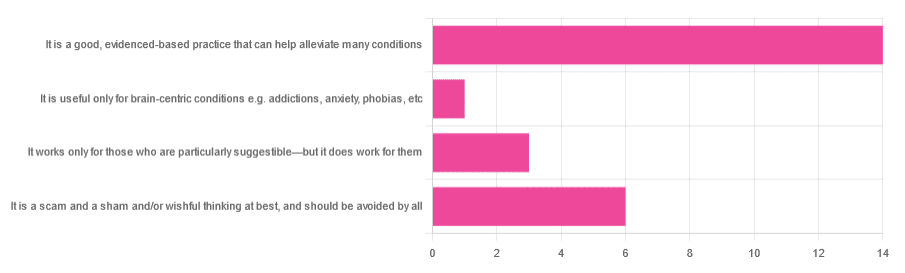
In Tuesday’s newsletter, we asked you for your opinions of hypnotherapy, and got the above-depicted, below-described, set of responses:
- About 58% said “It is a good, evidenced-based practice that can help alleviate many conditions”
- Exactly 25% said “It is a scam and sham and/or wishful thinking at best, and should be avoided by all”
- About 13% said “It works only for those who are particularly suggestible—but it does work for them”
- One (1) person said “It is useful only for brain-centric conditions e.g. addictions, anxiety, phobias, etc”
So what does the science say?
Hypnotherapy is all in the patient’s head: True or False?
True! But guess which part of your body controls much of the rest of it.
So while hypnotherapy may be “all in the head”, its effects are not.
Since placebo effect, nocebo effect, and psychosomatic effect in general are well-documented, it’s quite safe to say at the very least that hypnotherapy thus “may be useful”.
Which prompts the question…
Hypnotherapy is just placebo: True or False?
False, probably. At the very least, if it’s placebo, it’s an unusually effective placebo.
And yes, even though testing against placebo is considered a good method of doing randomized controlled trials, some placebos are definitely better than others. If a placebo starts giving results much better than other placebos, is it still a placebo? Possibly a philosophical question whose answer may be rooted in semantics, but happily we do have a more useful answer…
Here’s an interesting paper which: a) begins its abstract with the strong, unequivocal statement “Hypnosis has proven clinical utility”, and b) goes on to examine the changes in neural activity during hypnosis:
Brain Activity and Functional Connectivity Associated with Hypnosis
It works only for the very suggestible: True or False?
False, broadly. As with any medical and/or therapeutic procedure, a patient’s expectations can affect the treatment outcome.
And, especially worthy of note, a patient’s level of engagement will vastly affect it treatment that has patient involvement. So for example, if a doctor prescribes a patient pills, which the patient does not think will work, so the patient takes them intermittently, because they’re slow to get the prescription refilled, etc, then surprise, the pills won’t get as good results (since they’re often not being taken).
How this plays out in hypnotherapy: because hypnotherapy is a guided process, part of its efficacy relies on the patient following instructions. If the hypnotherapist guides the patient’s mind, and internally the patient is just going “nope nope nope, what a lot of rubbish” then of course it will not work, just like if you ask for directions in the street and then ignore them, you won’t get to where you want to be.
For those who didn’t click on the above link by the way, you might want to go back and have a look at it, because it included groups of individuals with “high/low hypnotizability” per several ways of scoring such.
It works only for brain-centric things, e.g. addictions, anxieties, phobias, etc: True or False?
False—but it is better at those. Here for example is the UK’s Royal College of Psychiatrists’ information page, and if you go to “What conditions can hypnotherapy help to treat”, you’ll see two broad categories; the first is almost entirely brain-stuff; the second is more varied, and includes pain relief of various kinds, burn care, cancer treatment side effects, and even menopause symptoms. Finally, warts and other various skin conditions get their own (positive) mention, per “this is possible through the positive effects hypnosis has on the immune system”:
RCPsych | Hypnosis And Hypnotherapy
Wondering how much psychosomatic effect can do?
You might like this previous article; it’s not about hypnotherapy, but it is about the difference the mind can make on physical markers of aging:
Aging, Counterclockwise: When Age Is A Flexible Number
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: