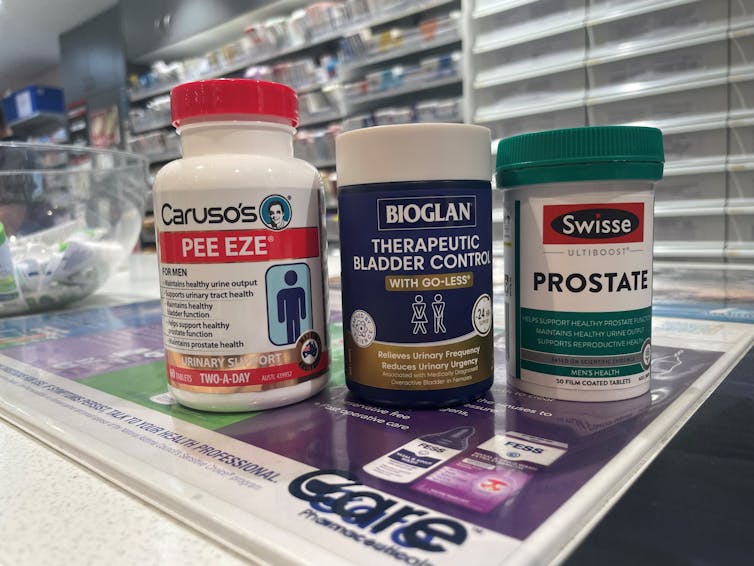
What’s in the supplements that claim to help you cut down on bathroom breaks? And do they work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With one in four Australian adults experiencing problems with incontinence, some people look to supplements for relief.
With ingredients such as pumpkin seed oil and soybean extract, a range of products promise relief from frequent bathroom trips.
But do they really work? Let’s sift through the claims and see what the science says about their efficacy.

What is incontinence?
Incontinence is the involuntary loss of bladder or bowel control, leading to the unintentional leakage of urine or faeces. It can range from occasional minor leaks to a complete inability to control urination and defecation.
This condition can significantly impact daily activities and quality of life, and affects women more often than it affects men.
Some people don’t experience bladder leakage but can sometimes feel an urgent need to go to the bathroom. This is known as overactive bladder syndrome, and occurs when the muscles around the bladder tighten on their own, which greatly reduces its capacity. The result is the person feels the need to go to the bathroom much more frequently.
There are many potential causes of incontinence and overactive bladders, including menopause, pregnancy and child birth, urinary tract infections, pelvic floor disorders, and an enlarged prostate. Conditions such as diabetes, neurological disorders and certain medications (such as diuretics, sleeping pills, antidepressants and blood-pressure drugs) can also contribute.
While pelvic muscle rehabilitation and behavioural techniques for bladder retraining can be helpful, some people are interested in pharmaceutical solutions.
What’s in these products?
A number of supplements are available in Australia that include ingredients used in traditional medicine for urinary incontinence and overactive bladders. The three most common ingredients are:
- Cucurbita pepo (pumpkin seed extract)
- glycine max (soybean extract)
- an extract from the bark of the Crateva magna or nurvala (Varuna) tree.
How are they supposed to work?
Pumpkin seeds are rich in plant sterols that are thought to reduce the testosterone-related enlargement of the prostate, as well as having broader anti-inflammatory effects. The seed extracts can also contain oleic acid, which may help increase bladder capacity by relaxing the muscles around the organ.
Soybean extracts are rich in isoflavones, especially daidzen and genistein. Like olieic acid, these are thought to act on the muscles around the bladder. Because isoflavones are similar in structure to the female hormone oestrogen, soy extracts may be most beneficial for postmenopausal women who have overactive bladders.
Crateva extract is rich in lupeol- and sterol-based chemicals which have strong anti-inflammatory effects. This has benefits not just for enlarged prostates but possibly also for reducing urinary tract infections.
Do they actually work?
It’s important to note that the government has only approved these types of supplements as “listed medicines”. This means the ingredients have only been assessed for safety. The companies behind the products have not had to provide evidence they actually work.
A 2014 clinical trial examined a combined pumpkin seed and soybean extract called cucurflavone on people with overactive bladders. The 120 participants received either a placebo or a daily 1,000mg dose of the herbal mixture over a period of 12 weeks.
By the end of study, those in the cucurflavone group went to the bathroom around three fewer times per day, compared with people in the control group, who only went to the bathroom on average one fewer time each day.
In a different trial, researchers examined a combination of Crateva bark extract with herbal extracts of horsetail and Japanese evergreen spicebush, called Urox.
For the 150 participants, the Urox formulation helped participants go to the bathroom less frequently when compared with placebo treatment.
After eight weeks of treatment, participants in the placebo group were going to the bathroom to urinate 11 times per day. Those in the Urox group were only going around to 7.5 times per day. And those who took Urox also needed to go to the bathroom one fewer time during the night.
Finally, another study also examined a Creteva, horsetail and Japanese spicebush combination, but this time in children. They were given either a 420mg dose of the supplement or a placebo, and then monitored for how many times they wet the bed.
After two months of taking the supplement, slightly more than 40% of the 24 kids in the supplement group wet the bed less often.
While these results may look promising, there are considerable limitations to the studies which means the data may not be reliable. For example, the trials didn’t include enough participants to have reliable data. To conclusively provide efficacy, final-stage clinical trials require data for between 300 and 3,000 patients.
From the studies, it is also not clear whether some participants were also taking other medicines as well as the supplement. This is important, as medications can interfere with how the supplements work, potentially making them less or more effective.
What if you want to take them?
If you have incontinence or an overactive bladder, you should always discuss this with your doctor, as it may due to a serious or treatable underlying condition.
Otherwise, your GP may give you strategies or exercises to improve your bladder control, prescribe medications or devices, or refer you to a specialist.
If you do decide to take a supplement, discuss this with your doctor and local pharmacist so they can check that any product you choose will not interfere with any other medications you may be taking.
Nial Wheate, Professor of Pharmaceutical Chemistry, Macquarie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Loving Someone Who Has Dementia – by Dr. Pauline Boss
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed Dr. Boss’s excellent book “Loss, Trauma, and Resilience: Therapeutic Work With Ambiguous Loss”, which partially overlaps in ideas with this one. In that case, it was about grief when a loved one is “gone, but are they really?”, which can include missing persons, people killed in ways that weren’t 100% confirmed (e.g. no body to bury), and in contrast, people who are present in body but not entirely present mentally: perhaps in a coma, for example. It also includes people are for other reasons not entirely present in the way they used to be, which includes dementia. And that latter case is what this book focuses on.
In the case of dementia, we cannot, of course, simply focus on ourselves. Well, not if we care about the person with dementia, anyway. Much like with the other kinds of ambiguous loss, we cannot fully come to terms with things while on the cusp of presence and absence, and we cannot, as such, “give up” on our loved one.
What then, of hope? The author makes the case for—in absence of any kind of closure—making our peace with the situation as it is, making our peace with the uncertainty of things. And that means not only “at any moment could come a more clearly complete loss”, but also on the flipside at least a faint candle of hope, that we should not grasp with both hands (that is not how to treat a candle, literally or metaphorically), but rather, hold gently, and enjoy its gentle light.
Dr. Boss also covers more practical considerations; family rituals, celebrations, gatherings, and the idea of “the good-enough relationship”. Particularly helpfully, she gives her “seven guidelines for the journey”, which even if one decides against adopting them all, are definitely all good things to at least have considered.
The style is much more tailored to the lay reader than the other book of hers that we reviewed, which was intended more for clinicians, but useful also for those of us who have been hit by such kinds of grief. In this case, however, her intention is first and foremost for the family of a person who has dementia—there are still footnotes throughout though, for those who still want to read scientific papers that support the various ideas discussed in the book.
Bottom line: if a loved one has dementia or that seems a likely possibility for you, this book can help a lot!
Share This Post
-
Honeydew vs Cantaloupe – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing honeydew to cantaloupe, we picked the cantaloupe.
Why?
In terms of macros, there’s not a lot between them—they’re both mostly water. Nominally, honeydew has more carbs while cantaloupe has more fiber and protein, but the differences are very small. So, a very slight win for cantaloupe.
Looking at vitamins: honeydew has slightly more of vitamins B5 and B6 (so, the vitamins that are in pretty much everything), while cantaloupe has a more of vitamins A, B1, B2, B3, C, and E (especially notably 67x more vitamin A, whence its color). A more convincing win for cantaloupe.
The minerals category is even more polarized: honeydew has more selenium (and for what it’s worth, more sodium too, though that’s not usually a plus for most of us in the industrialized world), while cantaloupe has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and zinc. An overwhelming win for cantaloupe.
No surprises: adding up the slight win for cantaloupe, the convincing win for cantaloupe, and the overwhelming win for cantaloupe, makes cantaloupe the overall best pick here.
Enjoy!
Want to learn more?
You might like to read:
From Apples to Bees, and High-Fructose Cs: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Share This Post
-
Chickpeas vs Black-Eyed Peas – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to black-eyed peas, we picked the chickpeas.
Why?
In terms of macros, chickpeas have more protein, carbs, and fiber, the ratio of the latter two also giving them the lower glycemic index. An easy win for chickpeas.
In the category of vitamins, chickpeas have more of vitamins B2, B6, C, E, K, and choline, while black-eyed peas have more of vitamins B1, B5, and B9. Another victory for chickpeas.
When it comes to minerals, things are even more pronounced: chickpeas have more calcium, copper, iron, manganese, phosphorus, potassium, selenium, and zinc, while black-eyed peas have (barely) more magnesium. An overwhelming win for chickpeas.
Adding up the sections makes for a very evident overall win for chickpeas; as ever, do enjoy either or both though; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
Cabbage vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing cabbage to carrots, we picked the carrots.
Why?
Both are top-tier vegetables! But as the Highlander said, “there can be only one”, and we say carrots get a marginal victory;
In terms of macros, nominally cabbage has slightly more protein (but it’s a tiny amount, and thus an even tinier difference) while carrots have slightly more fiber and carbs (but again, not big differences), as well as the lower glycemic index (but nobody is getting metabolic disease from eating cabbage). We could call this category a tie because it’s all so close, but by the numbers, it’s a slender victory for carrots.
In the category of vitamins, carrots have more of vitamins A, B1, B2, B3, B5, B6, and E, while cabbage has more of vitamins B9, C, K, and choline. Thus, a win for carrots, especially as carrots’ vitamin A is 167x what cabbage has.
When it comes to minerals, cabbage has more calcium, iron, manganese, and selenium, while carrots have more copper, phosphorus, potassium, and zinc. They’re both equal on magnesium, and their respective margins of difference for the other minerals were not big, so this round’s a clear tie.
Adding up the sections makes for an overall win for carrots, but by all means enjoy either or both (together, even, if you like!); diversity is good!
Want to learn more?
You might like:
12 Most Powerful Supplements and Foods to Increase Energy & Slow Down Aging
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Elegant Defense – by Matt Richtel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In a way, Richtel got the best and worst of the publication date lottery. This book, which he’d obviously been working on for however long, was published in March 2020. Yes, that March 2020. So, it obviously got a huge boost in sales that launced it to bestseller status, and/but it doesn’t actually discuss COVID at all.
What it does discuss, is—as one might expect—the immune system. Or really, the immune systems, plural, several systems working alongside each other. How we got to have such, how our immune functions work, where all the various immune cells come from and what part they play. What pathogens can do to fight and/or confuse (or even co-opt) our immune response, and what modern medicine can do to counteract the pathogens’ anti-countermeasure countermeasures. And how it can still go wrong.
The “Four Lives” promised in the subtitle are stories, and Richtel explains the immune system through specific people’s specific battles. In particular, a friend of his who had quite a remarkable battle against cancer, which was of course terrible for him, but illustrative for us.
The style of the book is very readably journalistic. The author is a Pulitzer-winning NYT journalist, and not normally a science writer. Here at 10almonds, “we like big bibliographies and we cannot lie”, and we didn’t get to enjoy that in this case. The book contained no bibliography (nor appropriate inline citations, nor equivalent footnotes). Maybe a future addition will include this.
Bottom line: there’s a lot of “science for the lay reader” here. While the lack of references is a big oversight, the book does give a very good overview of what both sides (immune response and pathogenic invasion) bring to the battle of your body.
Click here to check out Elegant Defense, and demystify immunology!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood-Stuffed Squash
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This stuffed squash recipe is packed with so many nutrient-dense ingredients, yet it feels delightfully decadent—a great recipe to have up your sleeve ready for fall.
You will need
- 1 large or two medium butternut squashes, halved lengthways and seeds removed (keep them; they are full of nutrients! You can sprout them, or dry them to use them at your leisure), along with some of the flesh from the central part above where the seeds are, so that there is room for stuffing
- 2 cups low-sodium vegetable stock
- 1 cup wild rice, rinsed
- 1 medium onion, finely chopped
- ½ cup walnuts, roughly chopped
- ½ cup dried
cranberriesgoji berries ← why goji berries? They have even more healthful properties than cranberries, and cranberries are hard to buy without so much added sugar that the ingredients list looks like “cranberries (51%), sugar (39%), vegetable oil (10%)”, whereas when buying goji berries, the ingredients list says “goji berries”, and they do the same culinary job. - ¼ cup pine nuts
- ½ bulb garlic, minced
- 1 tbsp dried thyme or 2 tsp fresh thyme, destalked
- 1 tbsp dried rosemary or 2 tsp fresh rosemary, destalked
- 1 generous handful fresh parsley, chopped
- 1 tbsp chia seeds
- 1 tbsp nutritional yeast
- 1 tbsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil, for brushing and frying
- Aged balsamic vinegar, to serve (failing this, make a balsamic vinegar reduction and use that; it should have a thicker texture but still taste acidic and not too sweet; the thickness should come from the higher concentration of grape must and its natural sugars; no need to add sugar)
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400°F / 200°C.
2) Brush the cut sides of the squash with olive oil; sprinkle with a pinch of MSG/salt and a little black pepper (grind it directly over the squash if you are using a grinder; hold the grinder high though so that it distributes evenly—waiters in restaurants aren’t just being dramatic when they do that with pepper or Parmesan or such)
3) Arrange them cut-sides-down on a baking tray lined with baking paper, and roast for at least 30 minutes or until tender.
4) While that is roasting, add the chia seeds to the wild rice, and cook them in the low-sodium vegetable stock, using a rice cooker if available. It should take about the same length of time, but if the rice is done first, set it aside, and if the squash is done first, turn the oven down low to keep it warm.
5) Heat some oil in a sauté pan (not a skillet without high sides; we’re going to need space in a bit), and fry the chopped onion until translucent and soft. We could say “about 5 minutes” but honestly it depends on your pan as well as the heat and other factors.
6) Add the seasonings (herbs, garlic, black pepper, MSG/salt, nooch), and cook for a further 2 minutes, stirring thoroughly to distribute evenly.
7) Add the rice, berries, and nuts, cooking for a further 2 minutes, stirring constantly, ensuring everything is heated evenly.
8) Remove the squash halves from the oven, turn them over, and spoon the mixture we just made into them, filling generously.
9) Drizzle a lashing of the aged balsamic vinegar (or balsamic vinegar reduction), to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Brown Rice vs Wild Rice – Which is Healthier?
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- Chia: The Tiniest Seeds With The Most Value
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: