What is mitochondrial donation? And how might it help people have a healthy baby one day?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Mitochondria are tiny structures in cells that convert the food we eat into the energy our cells need to function.
Mitochondrial disease (or mito for short) is a group of conditions that affect this ability to generate the energy organs require to work properly. There are many different forms of mito and depending on the form, it can disrupt one or more organs and can cause organ failure.
There is no cure for mito. But an IVF procedure called mitochondrial donation now offers hope to families affected by some forms of mito that they can have genetically related children free from mito.
After a law to allow mitochondrial donation in Australia was passed in 2022, scientists are now preparing for a clinical trial to see if mitochondrial donation is safe and works.

What is mitochondrial disease?
There are two types of mitochondrial disease.
One is caused by faulty genes in the nuclear DNA, the DNA we inherit from both our parents and which makes us who we are.
The other is caused by faulty genes in the mitochondria’s own DNA. Mito caused by faulty mitochondrial DNA is passed down through the mother. But the risk of disease is unpredictable, so a mother who is only mildly affected can have a child who develops serious disease symptoms.
Mitochondrial disease is the most common inherited metabolic condition affecting one in 5,000 people.
Some people have mild symptoms that progress slowly, while others have severe symptoms that progress rapidly. Mito can affect any organ, but organs that need a lot of energy such as brain, muscle and heart are more often affected than other organs.
Mito that manifests in childhood often involves multiple organs, progresses rapidly, and has poor outcomes. Of all babies born each year in Australia, around 60 will develop life-threatening mitochondrial disease.
What is mitochondrial donation?
Mitochondrial donation is an experimental IVF-based technique that offers people who carry faulty mitochondrial DNA the potential to have genetically related children without passing on the faulty DNA.
It involves removing the nuclear DNA from the egg of someone who carries faulty mitochondrial DNA and inserting it into a healthy egg donated by someone not affected by mito, which has had its nuclear DNA removed.
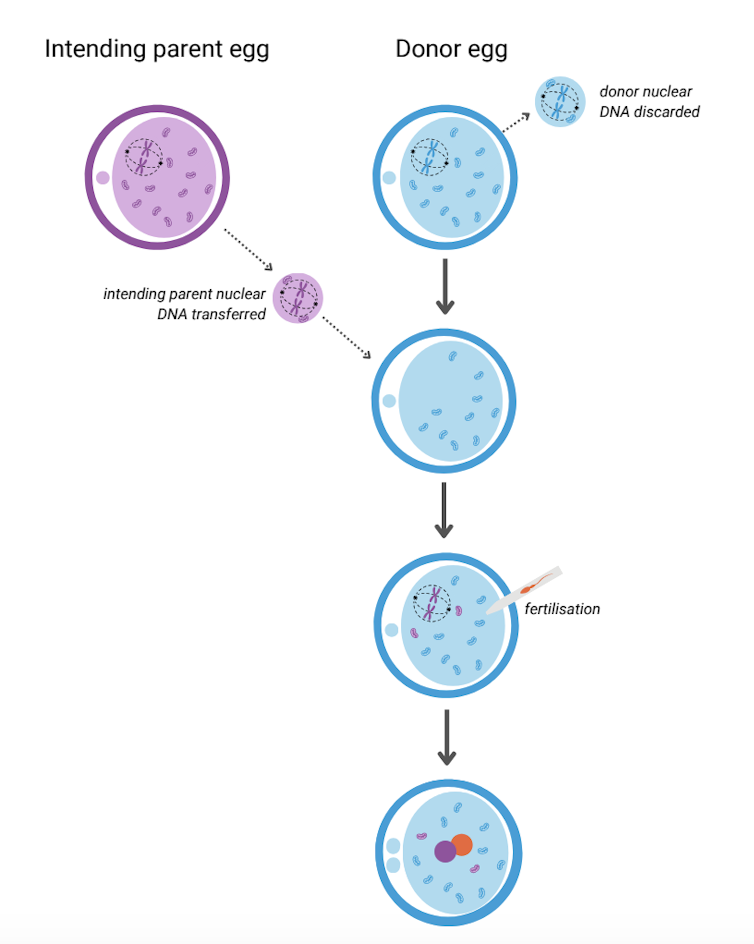
The resulting egg has the nuclear DNA of the intending parent and functioning mitochondria from the donor. Sperm is then added and this allows the transmission of both intending parents’ nuclear DNA to the child.
A child born after mitochondrial donation will have genetic material from the three parties involved: nuclear DNA from the intending parents and mitochondrial DNA from the egg donor. As a result the child will likely have a reduced risk of mito, or no risk at all.

This highly technical procedure requires specially trained scientists and sophisticated equipment. It also requires both the person with mito and the egg donor to have hormone injections to stimulate the ovaries to produce multiple eggs. The eggs are then retrieved in an ultrasound-guided surgical procedure.
Mitochondrial donation has been pioneered in the United Kingdom where a handful of babies have been born as a result. To date there have been no reports about whether they are free of mito.
Maeve’s Law
After three years of public consultation The Mitochondrial Donation Law Reform (Maeve’s Law) Bill 2021 was passed in the Australian Senate in 2022, making mitochondrial donation legal in a research and clinical trial setting.
Maeve’s law stipulates strict conditions including that clinics need a special licence to perform mitochondrial donation.
To make sure mitochondrial donation works and is safe before it’s introduced into Australian clinical practice, the law also specifies that initial licences will be issued for pre-clinical and clinical trial research and training.
We’re expecting one such licence to be issued for the mitoHOPE (Healthy Outcomes Pilot and Evaluation) program, which we are part of, to perfect the technique and conduct a clinical trial to make sure mitochondrial donation is safe and effective.
Before starting the trial, a preclinical research and training program will ensure embryologists are trained in “real-life” clinical conditions and existing mitochondrial donation techniques are refined and improved. To do this, many human eggs are needed.
The need for donor eggs
One of the challenges with mitochondrial donation is sourcing eggs. For the preclinical research and training program, frozen eggs can be used, but for the clinical trial “fresh” eggs will be needed.
One possible source of frozen eggs is from people who have stored eggs they don’t intend to use.
A recent study looked at data on the outcomes of eggs stored at a Melbourne clinic from 2012 to 2021. Over the ten-year period, 1,132 eggs from 128 patients were discarded. No eggs were donated to research because the clinics where the eggs were stored did not conduct research requiring donor eggs.
However, research shows that among people with stored eggs, the number one choice for what to do with eggs they don’t need is to donate them to research.
This offers hope that, given the opportunity, those who have eggs stored that they don’t intend to use might be willing to donate them to mitochondrial donation preclinical research.
As for the “fresh” eggs needed in the future clinical trial, this will require individuals to volunteer to have their ovaries stimulated and eggs retrieved to give those people impacted by mito a chance to have a healthy baby. Egg donors may be people who are friends or relatives of those who enter the trial, or it might be people who don’t know someone affected by mito but would like to help them conceive.
At this stage, the aim is to begin enrolling participants in the clinical trial in the next 12 to 18 months. However this may change depending on when the required licences and ethics approvals are granted.
Karin Hammarberg, Senior Research Fellow, Global and Women’s Health, School of Public Health & Preventive Medicine, Monash University; Catherine Mills, Professor of Bioethics, Monash University; Mary Herbert, Professor, Anatomy & Developmental Biology, Monash University, and Molly Johnston, Research fellow, Monash Bioethics Centre, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How light tells you when to sleep, focus and poo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is the next article in our ‘Light and health’ series, where we look at how light affects our physical and mental health in sometimes surprising ways. Read other articles in the series.
Exposure to light is crucial for our physical and mental health, as this and future articles in the series will show.
But the timing of that light exposure is also crucial. This tells our body to wake up in the morning, when to poo and the time of day to best focus or be alert. When we’re exposed to light also controls our body temperature, blood pressure and even chemical reactions in our body.
But how does our body know when it’s time to do all this? And what’s light got to do with it?
nymphoenix/Shutterstock What is the body clock, actually?
One of the key roles of light is to re-set our body clock, also known as the circadian clock. This works like an internal oscillator, similar to an actual clock, ticking away as you read this article.
But rather than ticking you can hear, the body clock is a network of genes and proteins that regulate each other. This network sends signals to organs via hormones and the nervous system. These complex loops of interactions and communications have a rhythm of about 24 hours.
In fact, we don’t have one clock, we have trillions of body clocks throughout the body. The central clock is in the hypothalamus region of the brain, and each cell in every organ has its own. These clocks work in concert to help us adapt to the daily cycle of light and dark, aligning our body’s functions with the time of day.
However, our body clock is not precise and works to a rhythm of about 24 hours (24 hours 30 minutes on average). So every morning, the central clock needs to be reset, signalling the start of a new day. This is why light is so important.
The central clock is directly connected to light-sensing cells in our retinas (the back of the eye). This daily re-setting of the body clock with morning light is essential for ensuring our body works well, in sync with our environment.
In parallel, when we eat food also plays a role in re-setting the body clock, but this time the clock in organs other than the brain, such as the liver, kidneys or the gut.
So it’s easy to see how our daily routines are closely linked with our body clocks. And in turn, our body clocks shape how our body works at set times of the day.
What time of day?
Matt Garrow/The Conversation. Adapted from Delos, CC BY Let’s take a closer look at sleep
The naturally occurring brain hormone melatonin is linked to our central clock and makes us feel sleepy at certain times of day. When it’s light, our body stops making melatonin (its production is inhibited) and we are alert. Closer to bedtime, the hormone is made, then secreted, making us feel drowsy.
Our sleep is also partly controlled by our genes, which are part of our central clock. These genes influence our chronotype – whether we are a “lark” (early riser), “night owl” (late sleeper) or a “dove” (somewhere in between).
But exposure to light at night when we are supposed to be sleeping can have harmful effects. Even dim light from light pollution can impair our heart rate and how we metabolise sugar (glucose), may lead to psychiatric disorders such as depression, anxiety and bipolar disorder, and increases the overall risk of premature death.
The main reason for these harmful effects is that light “at the wrong time” disturbs the body clock, and these effects are more pronounced for “night owls”.
This “misaligned” exposure to light is also connected to the detrimental health effects we often see in people who work night shifts, such as an increased risk of cancer, diabetes and heart disease.
How about the gut?
Digestion also follows a circadian rhythm. Muscles in the colon that help move waste are more active during the day and slow down at night.
The most significant increase in colon movement starts at 6.30am. This is one of the reasons why most people feel the urge to poo in the early morning rather than at night.
The gut’s day-night rhythm is a direct result of the action of the gut’s own clock and the central clock (which synchronises the gut with the rest of the body). It’s also influenced by when we eat.
At 6.30am, your gut really begins to get going for the day. Rendra Dria Septia Aji/Shutterstock How about focusing?
Our body clock also helps control our attention and alertness levels by changing how our brain functions at certain times of day. Attention and alertness levels improve in the afternoon and evening but dip during the night and early morning.
Those fluctuations impact performance and can lead to decreased productivity and an increased risk of errors and accidents during the less-alert hours.
So it’s important to perform certain tasks that require our attention at certain times of day. That includes driving. In fact, disruption of the circadian clock at the start of daylight savings – when our body hasn’t had a chance to adapt to the clocks changing – increases the risk of a car accident, particularly in the morning.
What else does our body clock control?
Our body clock influences many other aspects of our biology, including:
- physical performance by controlling the activity of our muscles
- blood pressure by controlling the system of hormones involved in regulating our blood volume and blood vessels
- body temperature by controlling our metabolism and our level of physical activity
- how our body handles drugs and toxins by controlling enzymes involved in how the liver and kidneys eliminate these substances from the body.
If you can, avoid driving long distances at night, as you’ll be less alert. trendobjects/Shutterstock Morning light is important
But what does this all mean for us? Exposure to light, especially in the morning, is crucial for synchronising our circadian clock and bodily functions.
As well as setting us up for a good night’s sleep, increased morning light exposure benefits our mental health and reduces the risk of obesity. So boosting our exposure to morning light – for example, by going for a walk, or having breakfast outside – can directly benefit our mental and metabolic health.
However, there are other aspects about which we have less control, including the genes that control our body clock.
Frederic Gachon, Associate Professor, Physiology of Circadian Rhythms, Institute for Molecular Bioscience, The University of Queensland and Benjamin Weger, NHMRC Emerging Leadership Fellow Institute for Molecular Bioscience, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Type 2 Diabetic Foot Problems
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: I’d like to know more about type 2 diabetic foot problems
You probably know that the “foot problems” thing has less to do with the feet and more to do with blood and nerves. So, why the feet?
The reason feet often get something like the worst of it, is because they are extremities, and in the case of blood sugars being too high for too long too often, they’re getting more damage as blood has to fight its way back up your body. Diabetic neuropathy happens when nerves are malnourished because the blood that should be keeping them healthy, is instead syrupy and sluggish.
We’ll definitely do a main feature sometime soon on keeping blood sugars healthy, for both types of diabetes plus pre-diabetes and just general advice for all.
In the meantime, here’s some very good advice on keeping your feet healthy in the context of diabetes. This one’s focussed on Type 1 Diabetes, but the advice goes for both:
! Share This Post
-
Breathe; Don’t Vent (At Least In The Moment)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Zen And The Art Of Breaking Things
We’ve talked before about identifying emotions and the importance of being able to express them:
Answering The Most Difficult Question: How Are You?
However, there can be a difference between “expressing how we feel” and “being possessed by how we feel and bulldozing everything in our path”
…which is, of course, primarily a problem in the case of anger—and by extension, emotions that are often contemporaneous with anger, such as jealousy, shame, fear, etc.
How much feeling is too much?
While this is in large part a subjective matter, clinically speaking the key question is generally: is it adversely affecting daily life to the point of being a problem?
For example, if you have to spend half an hour every day actively managing a certain emotion, that’s probably indicative of something unusual, but “unusual” is not inherently bad. If you’re managing it safely and in a way that doesn’t negatively affect the rest of your life, then that is generally considered fine, unless you feel otherwise about it.
A good example of this is complicated grief and/or prolonged grief.
But what about when it comes to anger? How much is ok?
When it comes to those around you, any amount of anger can seem like too much. Anger often makes us short-tempered even with people who are not the object of our anger, and it rarely brings out the best in us.
We can express our feelings in non-aggressive ways, for example:
and
Seriously Useful Communication Skills!
Sometimes, there’s another way though…
Breathe; don’t vent
That’s a great headline, but we can’t take the credit for it, because it came from:
Breathe, don’t vent: turning down the heat is key to managing anger
…in which it was found that, by all available metrics, the popular wisdom of “getting it off your chest” doesn’t necessarily stand up to scrutiny, at least in the short term:
❝The work was inspired in part by the rising popularity of rage rooms that promote smashing things (such as glass, plates and electronics) to work through angry feelings.
I wanted to debunk the whole theory of expressing anger as a way of coping with it,” she said. “We wanted to show that reducing arousal, and actually the physiological aspect of it, is really important.❞
And indeed, he and his team did find that various arousal-increasing activities (such as hitting a punchbag, breaking things, doing vigorous exercise) did not help as much as arousal-decreasing activities, such as mindfulness-based relaxation techniques.
If you’d like to read the full paper, then so would we, but we couldn’t get full access to this one yet. However, the abstract includes representative statistics, so that’s worth a once-over:
Caveat!
Did you notice the small gap between their results and their conclusion?
In a lab or similar short-term observational setting, their recommendation is clearly correct.
However, if the source of your anger is something chronic and persistent, it could well be that calming down without addressing the actual cause is just “kicking the can down the road”, and will still have to actually be dealt with eventually.
So, while “here be science”, it’s not a mandate for necessarily suffering in silence. It’s more about being mindful about how we go about tackling our anger.
As for a primer on mindfulness, feel free to check out:
No-Frills, Evidence-Based Mindfulness
Take care!
Share This Post
Related Posts
-
The Brain Alarm Signs That Warn Of Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to predicting age-related cognitive impairment:
First there are genetic factors to take into account (such as the APOE4 gene for Alzheimer’s), as well as things such as age and sex.
When it comes to sex, by the way, what matters here is hormones, which is why [it seems; this as technically as yet unproven with full rigor, but the hypothesis is sound and there is a body of evidence gradually being accumulated to support it] postmenopausal women with untreated menopause get Alzheimer’s at a higher rate and deteriorate more quickly:
Alzheimer’s Sex Differences May Not Be What They Appear
Next, there are obviously modifiable lifestyle factors to take into account, things that will reduce your risk such as getting good sleep, good diet, good exercise, and abstaining from alcohol and smoking, as well as oft-forgotten things such as keeping cognitively active and, equally importantly, socially active:
How To Reduce Your Alzheimer’s Risk
(the article outlines what matters the most in each of the above areas, by the way, so that you can get the most bang-for-buck in terms of lifestyle adjustments)
Lastly (in the category of risk factors), there are things to watch out for in the blood such as hypertension and high cholesterol.
Nipping it in the blood
In new research (so new it is still ongoing, but being at year 2 of a 4-year prospective study, they have published a paper with their results so far), researchers have:
- started with the premise “dementia is preceded by mild cognitive impairment”
- then, asked the question “what are the biometric signs of mild cognitive impairment?”
Using such tools as functional near-infrared spectroscopy (fNIRS) while the participants performed cognitive tasks, they were able to record changes in plasma levels of extracellular vesicles, assessing them with small-particle flow cytometry.
Translating from sciencese: they gave the participants mental tasks, and while they completed them, the researchers scanned their brains and monitored blood flow and the brain’s ability to compensate for any lack of it.
What they found:
- in young adults, blood flow increased, facilitating neurovascular coupling (this is good)
- in older adults, blood flow did not increase as much, but they engaged other areas of the brain to compensate, by what’s called functional connectivity (this is next best)
- in those with mild cognitive impairment, blood flow was reduced, and they did not have the ability to compensate by functional connectivity (this is not good)
They also performed a liquid biopsy, which sounds alarming but it just means they took some blood, and tested this for density of cerebrovascular endothelial extracellular vesicles (CEEVs), which—in more prosaic words—are bits from the cells lining the blood vessels in the brain.
People with mild cognitive impairment had more of these brain bits in their blood than those without.
You can read the paper itself here:
What this means
The science here is obviously still young (being as it is still in progress), but this will likely contribute greatly to early warning signs of dementia, by catching mild cognitive impairment in its early stages, by means of a simple blood test, instead of years of wondering before getting a dementia diagnosis.
And of course, forewarned is forearmed, so if this is something that could be done as a matter of routine upon hitting the age of, say, 65 and then periodically thereafter, it would catch a lot of cases while there’s still more time to turn things around.
As for how to turn things around, well, we imagine you have now read our “How To Reduce Your Alzheimer’s Risk” article linked up top (if not, we recommend checking it out), and there is also…
Do Try This At Home: The 12-Week Brain Fitness Program To Measurably Boost Your Brain
Take care!
When it comes to predicting age-related cognitive impairment:
First there are genetic factors to take into account (such as the APOE4 gene for Alzheimer’s), as well as things such as age and sex.
When it comes to sex, by the way, what matters here is hormones, which is why [it seems; this as technically as yet unproven with full rigor, but the hypothesis is sound and there is a body of evidence gradually being accumulated to support it] postmenopausal women with untreated menopause get Alzheimer’s at a higher rate and deteriorate more quickly:
Alzheimer’s Sex Differences May Not Be What They Appear
Next, there are obviously modifiable lifestyle factors to take into account, things that will reduce your risk such as getting good sleep, good diet, good exercise, and abstaining from alcohol and smoking, as well as oft-forgotten things such as keeping cognitively active and, equally importantly, socially active:
How To Reduce Your Alzheimer’s Risk
(the article outlines what matters the most in each of the above areas, by the way, so that you can get the most bang-for-buck in terms of lifestyle adjustments)
Lastly (in the category of risk factors), there are things to watch out for in the blood such as hypertension and high cholesterol.
Nipping it in the blood
In new research (so new it is still ongoing, but being at year 2 of a 4-year prospective study, they have published a paper with their results so far), researchers have:
- started with the premise “dementia is preceded by mild cognitive impairment”
- then, asked the question “what are the biometric signs of mild cognitive impairment?”
Using such tools as functional near-infrared spectroscopy (fNIRS) while the participants performed cognitive tasks, they were able to record changes in plasma levels of extracellular vesicles, assessing them with small-particle flow cytometry.
Translating from sciencese: they gave the participants mental tasks, and while they completed them, the researchers scanned their brains and monitored blood flow and the brain’s ability to compensate for any lack of it.
What they found:
- in young adults, blood flow increased, facilitating neurovascular coupling (this is good)
- in older adults, blood flow did not increase as much, but they engaged other areas of the brain to compensate, by what’s called functional connectivity (this is next best)
- in those with mild cognitive impairment, blood flow was reduced, and they did not have the ability to compensate by functional connectivity (this is not good)
They also performed a liquid biopsy, which sounds alarming but it just means they took some blood, and tested this for density of cerebrovascular endothelial extracellular vesicles (CEEVs), which—in more prosaic words—are bits from the cells lining the blood vessels in the brain.
People with mild cognitive impairment had more of these brain bits in their blood than those without.
You can read the paper itself here:
What this means
The science here is obviously still young (being as it is still in progress), but this will likely contribute greatly to early warning signs of dementia, by catching mild cognitive impairment in its early stages, by means of a simple blood test, instead of years of wondering before getting a dementia diagnosis.
And of course, forewarned is forearmed, so if this is something that could be done as a matter of routine upon hitting the age of, say, 65 and then periodically thereafter, it would catch a lot of cases while there’s still more time to turn things around.
As for how to turn things around, well, we imagine you have now read our “How To Reduce Your Alzheimer’s Risk” article linked up top (if not, we recommend checking it out), and there is also…
Do Try This At Home: The 12-Week Brain Fitness Program To Measurably Boost Your Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beetroot vs Carrot – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing beetroot to carrot, we picked the carrot.
Why?
It was close! And beetroot does have its advantages, but we say carrot wins on balance.
In terms of macros, these two root vegetables are close to identical, down to both having 9.57g carbs per 100g, and 2.8g fiber per 100g. Technically, beetroot has a smidgen more protein, but nobody’s eating these for their tiny protein content.
When it comes to vitamins, it’s not close and the margins are mostly huge: carrots have a lot more of vitamins A, B1, B2, B3, B5, B6, C, E, K, and choline, while beetroot has more vitamin B9.
In the category of minerals, superficially it swings the other way, but the margins this time are small. Nevertheless, beetroot has more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while carrots have more calcium.
This would make things, on balance, a tie: equal on macros, carrots win on vitamins, beetroot wins on minerals.
But because of the relative margins of difference, carrots win the day, because they’re almost as good as beetroot on those minerals, whereas beetroot doesn’t come close to carrot on the vitamins.
Want to learn more?
You might like to read:
From Apples to Bees, and high-fructose C’s: Which Sugars Are Healthier, And Which Are Just The Same?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Lessons For A Healthy Mind & Body
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sadia Badiei, food scientist of “Pick Up Limes” culinary fame, has advice in and out of the kitchen:
Pick up a zest for life
Here’s what she picked up, and we all can too:
- “I can’t do it… yet”: it’s never too late to adopt a growth mindset by adding “yet” to your self-doubt, focusing on progress and the possibility of improvement.
- The spotlight effect: people are generally too absorbed in their own lives to focus on you, so don’t worry too much about others’ perceptions.
- Nutrition by addition: focus on adding healthier foods to your diet rather than eliminating the less healthy ones to avoid restrictive mindsets. You can still eliminate the less healthy ones if you want to! It just shouldn’t be the primary focus. Focusing on a conceptually negative thing is rarely helpful.
- It’s ok to change: embrace change as a sign of growth and evolution, rather than seeing it as a failure or waste of time.
- The way you do one thing is the way you do everything: be mindful of how you approach small tasks, regular tasks, boring tasks, unwanted tasks—you can either create a habit of enthusiasm or a habit of suffering (it’s entirely your choice which)
- Setting goals for success: set goals based on actions you can control (inputs) rather than outcomes that are uncertain. Less “lose 10 lbs”, and more “eat fiber before starch”, for example.
- You probably can’t have it all at once: you can achieve all your dreams, but often not simultaneously; goals and desires unfold in stages over time.
- The five-year rule: before adopting a new lifestyle or habit, ask yourself if you can realistically sustain it for five years to ensure it’s not just a short-term fix. If you struggle with this prognostic, look backwards first instead. Which healthy habits have you maintained for decades, and which were you never able to make stick?
- Are you afraid or excited?: reframe fear as excitement, as both emotions share similar physical sensations and signify that you care about the outcome.
- The voice you hear most: speak kindly to yourself in self-talk to create a softer, more compassionate tone. Your subconscious is always listening, so reinforce healthy rather than unhealthy thought patterns.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
80-Year-Olds Share Their Biggest Regrets
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: