What Different Kinds of Hair Loss/Thinning Say About Your Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Siobhan Deshauer shows us different kinds of hair loss, what causes them, and what can be done about them:
Many different causes
Here’s how to tell them apart:
- Alopecia areata is an autoimmune condition where the immune system mistakenly attacks hair follicles, causing hair loss that can occur at any age and affects about 1 in 50 people. It often presents as smooth patches of hair loss and can be treated with steroid injections. Severe cases may require high-dose prednisone, which can restore hair growth over time.
- Discoid lupus is an autoimmune disease that affects the skin, leading to inflammation, scarring, and permanent hair loss. Unlike alopecia areata, it causes visible damage to the scalp and hair follicles. This type of lupus typically does not involve internal organs, unlike systemic lupus.
- Telogen effluvium occurs when a major systemic shock, such as an infection, surgery, or significant stress, triggers many hair follicles to enter the resting phase simultaneously, resulting in delayed hair shedding. The condition is diagnosed with a “hair pull test” and is typically temporary, as the resting phase is followed by normal hair growth phases.
- Allergic reactions to products, such as hair dye containing PPD, can cause hair loss due to scalp irritation and inflammation. An allergic response may trigger hair follicles to enter a resting phase, leading to hair loss by the same mechanism as telogen effluvium. Treatment with steroids can calm the reaction, and hair usually regrows after recovery.
- Syphilis, a sexually transmitted infection, can present with varied symptoms, including hair loss in a distinct moth-eaten pattern. Hair loss due to syphilis is reversible and curable with penicillin treatment, with hair regrowth typically occurring a few months after treatment.
- Biotin deficiency is rare due to its production by gut bacteria and presence in foods such as nuts, seeds, and beans such as soybeans. Deficiency can result from excessive consumption of raw egg whites, which block absorption. Severe deficiency causes hair loss and skin issues but can be treated effectively with biotin supplements.
- Iron deficiency anemia can cause hair thinning along with symptoms like fatigue and breathlessness. It often results from inadequate dietary intake, but can also occur after heavy menstrual bleeding. Treatment with iron supplements, or blood transfusions in severe cases, can restore both hair and energy levels, leading to significant improvements.
- Trichotillomania is a psychological condition marked by an uncontrollable urge to pull out one’s hair, often associated with anxiety or depression. Hair patches may show different stages of regrowth. While it can be challenging to manage, the condition can be treated with appropriate psychological and medical support.
- Traction alopecia results from hairstyles that exert prolonged tension on the hair, causing it to thin or fall out. This type of hair loss can be prevented by reducing the strain on the hair. Loosening hairstyles and giving the scalp a break can help hair regrow over time.
- Hypothyroidism causes symptoms like fatigue, dry skin, and hair thinning due to insufficient thyroid hormone production—however, it can be managed with diet, and if necessary, thyroid medications.
- Zinc deficiency may also cause hair loss and a characteristic rash. Treatment with zinc supplements can significantly improve hair growth and other symptoms.
- Medications, such as chemotherapy drugs, Accutane, and anti-seizure medications like valproic acid, are known to cause hair loss as a side effect. This type of hair loss is often reversible once the medication is stopped.
- Male pattern hair loss, or androgenic alopecia, is influenced by testosterone and genetic risk factors—which, contrary to popular belief, can come from either or both sides of the family. Early onset, especially before age 40, is linked to an increased risk of heart disease. However, effective treatments are available, and early intervention is beneficial.
- Female pattern hair loss is basically the same thing as male pattern hair loss (indeed, it is literally still androgenic alopecia), just a) almost always much less severe and b) with a gender-appropriate name. It affects up to 40% of women by age 50 and is characterized by thinning hair at the top of the head. It’s related to hormonal imbalances involving testosterone, such as those seen in PCOS and menopause, amongst other less common causes. Early treatment can be effective, and research is ongoing to develop more targeted therapies.
Dr. Siobhan Deshauer advises, if you’re experiencing hair loss, to monitor other symptoms too if applicable, take photos for tracking, and consult a doctor early for diagnosis and potential treatment.
For more on all of this plus visual illustrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Joy Of Missing Out
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What this is not going to be: a sour grapes thing.
What this is going to be: an exploration of how the grass is greener
on the other side of the fencewherever you water itIt’s easy to feel lonely and isolated, even in today’s increasingly-connected world. We’ve tackled that topic before:
How To Beat Loneliness & Isolation
One of the more passive (but still reasonable) ways of reducing isolation is to simply say “yes” more, which we discussed (along with other more active strategies) here:
When The World Moves Without Us… Can We Side-Step Age-Related Alienation?
But, is there any benefit to be gained from not being in the thick of things?
Sometimes some things associated with isolation are not, in reality, necessarily isolating. See for example:
But, the implications of embracing the “joy of missing out” are much more wide-reaching:
Wherever you are, there you are
You’ve probably read before the phrase “wherever you go, there you are”, but this phrasing brings attention to the fact that you already are where you are.
There are quite possibly aspects of your current life/situation that are not ideal, but take a moment to appreciate where you are in life. At the very least, you are probably in a safe warm dry house with plenty of food available; chances are you have plenty of luxuries too.
See also: How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
And yet, it’s easy to have a fear of missing out. Even billionaires fear they do not have enough and must acquire more in order to be truly secure and fulfilled.
As it goes for material wealth, so it also goes for social wealth—in other words, we may worry about such questions as: on whom can we rely, and who will be there for us if we need them? Do we, ultimately, have enough social capital to be secure?
- For social media influencers, it’ll be follower counts and engagement.
- For the family-oriented, it might be the question of whose house a given holiday gets celebrated at, and who attends, and who does it best.
- In more somber matters, think about funerals, and those where “there was such a huge turnout” vs “almost nobody attended”.
It sure sounds a lot like a dog-eat-dog world in which missing out sucks! But it doesn’t have to.
So let’s recap: your current situation is probably, all things considered, not bad. There is probably much in life to enjoy. If people do not come to your holiday event, then those are not people who would have improved things for you. If people do not attend your funeral even, then well, you yourself will be late, so hey.
Right now though, you are alive, so…
Enjoy the moment; enjoy your life for you.
Invest in yourself. Better yourself. Improve your environment for yourself little by little.
We spend a lot of time in life living up to everyone’s expectations, often without stopping to question whether it is what we want, or sometimes putting aside what we want in favor of what is wanted of us.
- Sometimes, such ostensible altruism is laudable and good (the point of today’s article is not “be a selfish jerk”; sometimes we should indeed shelve our self-interest in favour of doing something for the common good)
- Sometimes, it’s just pointless sacrifice that benefits nobody (the point of today’s article is “there is no point in playing stressful, stacked games when you could have a better time not doing that”)
If you are about to embark on an endeavor that you don’t really want to, take a moment to seriously consider which of the above two situations this is, and then act accordingly.
For a deeper dive into that, you might like this book that we reviewed a while back:
The Joy of Saying No – by Natalie Lue
Enjoy!
Share This Post
-
Who will look after us in our final years? A pay rise alone won’t solve aged-care workforce shortages
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Aged-care workers will receive a significant pay increase after the Fair Work Commission ruled they deserved substantial wage rises of up to 28%. The federal government has committed to the increases, but is yet to announce when they will start.
But while wage rises for aged-care workers are welcome, this measure alone will not fix all workforce problems in the sector. The number of people over 80 is expected to triple over the next 40 years, driving an increase in the number of aged care workers needed.
How did we get here?
The Royal Commission into Aged Care Quality and Safety, which delivered its final report in March 2021, identified a litany of tragic failures in the regulation and delivery of aged care.
The former Liberal government was dragged reluctantly to accept that a total revamp of the aged-care system was needed. But its weak response left the heavy lifting to the incoming Labor government.
The current government’s response started well, with a significant injection of funding and a promising regulatory response. But it too has failed to pursue a visionary response to the problems identified by the Royal Commission.
Action was needed on four fronts:
- ensuring enough staff to provide care
- building a functioning regulatory system to encourage good care and weed out bad providers
- designing and introducing a fair payment system to distribute funds to providers and
- implementing a financing system to pay for it all and achieve intergenerational equity.
A government taskforce which proposed a timid response to the fourth challenge – an equitable financing system – was released at the start of last week.
Consultation closed on a very poorly designed new regulatory regime the week before.
But the big news came at end of the week when the Fair Work Commission handed down a further determination on what aged-care workers should be paid, confirming and going beyond a previous interim determination.
What did the Fair Work Commission find?
Essentially, the commission determined that work in industries with a high proportion of women workers has been traditionally undervalued in wage-setting. This had consequences for both care workers in the aged-care industry (nurses and Certificate III-qualified personal-care workers) and indirect care workers (cleaners, food services assistants).
Aged-care staff will now get significant pay increases – 18–28% increase for personal care workers employed under the Aged Care Award, inclusive of the increase awarded in the interim decision.
The commission determined aged care work was undervalued.
Shutterstock/Toa55Indirect care workers were awarded a general increase of 3%. Laundry hands, cleaners and food services assistants will receive a further 3.96% on the grounds they “interact with residents significantly more regularly than other indirect care employees”.
The final increases for registered and enrolled nurses will be determined in the next few months.
How has the sector responded?
There has been no push-back from employer groups or conservative politicians. This suggests the uplift is accepted as fair by all concerned.
The interim increases of up to 15% probably facilitated this acceptance, with the recognition of the community that care workers should be paid more than fast food workers.
There was no criticism from aged-care providers either. This is probably because they are facing difficulty in recruiting staff at current wage rates. And because government payments to providers reflect the actual cost of aged care, increased payments will automatically flow to providers.
When the increases will flow has yet to be determined. The government is due to give its recommendations for staging implementation by mid-April.
Is the workforce problem fixed?
An increase in wages is necessary, but alone is not sufficient to solve workforce shortages.
The health- and social-care workforce is predicted to grow faster than any other sector over the next decade. The “care economy” will grow from around 8% to around 15% of GDP over the next 40 years.
This means a greater proportion of school-leavers will need to be attracted to the aged-care sector. Aged care will also need to attract and retrain workers displaced from industries in decline and attract suitably skilled migrants and refugees with appropriate language skills.
Aged care will need to attract workers from other sectors.
nastya_ph/ShutterstockThe caps on university and college enrolments imposed by the previous government, coupled with weak student demand for places in key professions (such as nursing), has meant workforce shortages will continue for a few more years, despite the allure of increased wages.
A significant increase in intakes into university and vocational education college courses preparing students for health and social care is still required. Better pay will help to increase student demand, but funding to expand place numbers will ensure there are enough qualified staff for the aged-care system of the future.
Stephen Duckett, Honorary Enterprise Professor, School of Population and Global Health, and Department of General Practice and Primary Care, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Yoga for Better Sleep – by Mark Stephens
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book has, as you might expect:
- postural exercises
- breathing exercises
- meditation exercises
Instructions given in all of the above categories are clear and easy to follow, and there are photographic illustrations too where appropriate.
What sets it apart from many books of this kind is that it also has chapters dedicated to various specific circumstances; the many actual reasons people seriously struggle to sleep; not just “screentime too late”, but for example deprepression, sleep apnea, hyperarousal, or even just aging.
As well as the comprehensive exercises, there are also many tips, tricks, hacks, and workarounds—it’s a practical guidebook with practical advice.
While the book is about yogic practices, the author also does tackle this holistically, acknowledging that there are many factors going on, and that yogic practices should be one more string to our sleep-improving bow—as we continue with other general good advice for good sleep too, have medical tests if it seems appropriate, that kind of thing. Basically, to have one’s assorted approaches work together with synergistic effect.
Bottom line: this book will quite possibly put you to sleep! But only in the best possible way.
Click here to check out Yoga for Better Sleep, and get those valuable Zs in, healthily!
Share This Post
Related Posts
-
Health Simplified – by Daniel Cottmeyer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Simplified – by Daniel Cottmeyer
A lot of books focus on the most marketable aspects of health, such as fat loss or muscle gain. Instead, Cottmeyer takes a “birds-eye-view” of health in all its aspects, and then boils it down to the most critical key parts.
Rather than giving a science-dense tome that nobody reads, or a light motivational piece that everyone reads but it amounts to “you can do it!”, here we get substance… but in a digestible form.
Which we at 10almonds love.
The book presents a simple action plan to:
- Improve your relationship with food/exercise
- Actually get better sleep
- Understand how nutrition really works
- Set up helpful habits that are workable and sustainable
- Bring these components together synergistically
Bottom line: if you’re going to buy only one health/fitness book, this is a fine contender.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
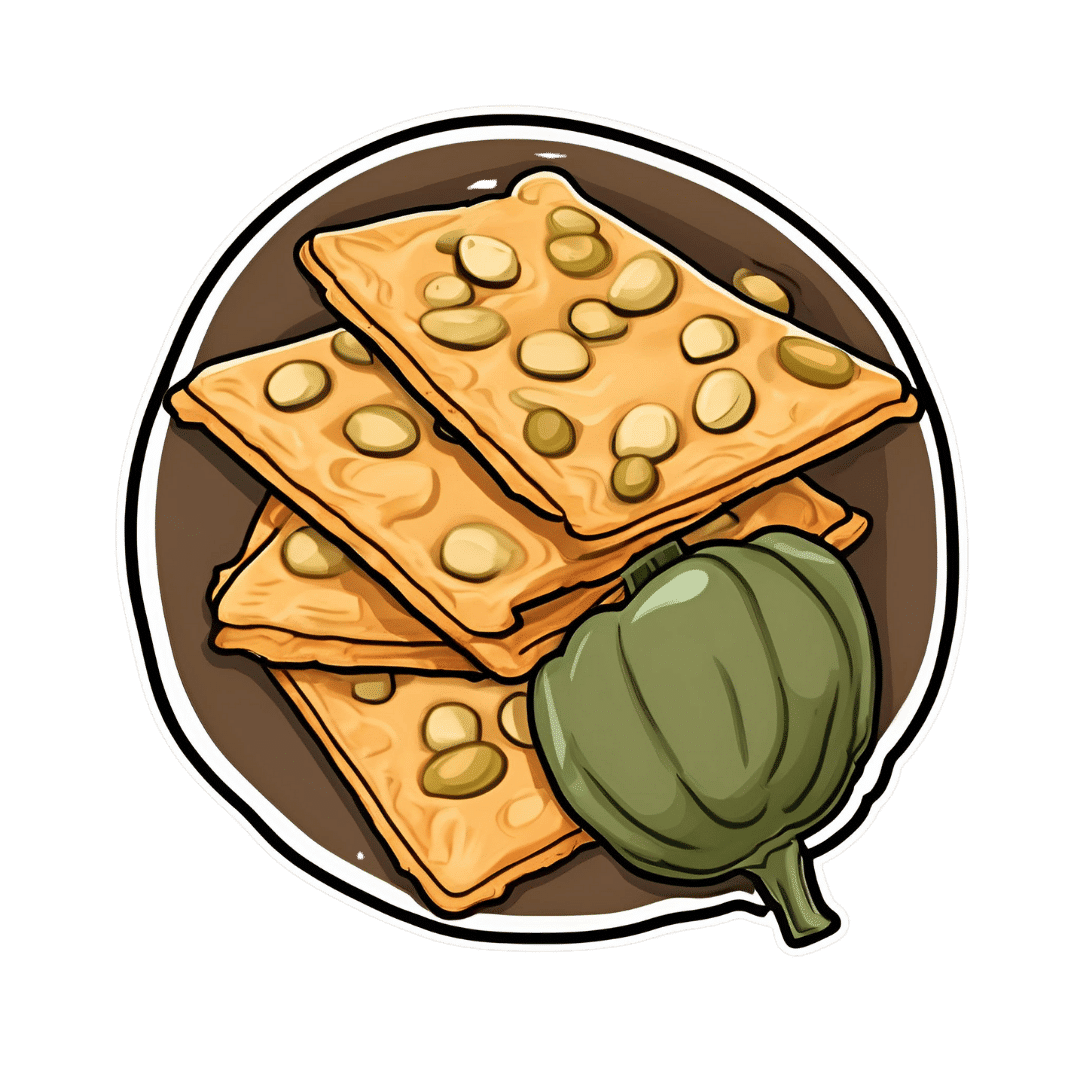
Pumpkin Protein Crackers
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ten of these (give or take what size you make them) will give you the 20g protein that most people’s body’s can use at a time. Five of these plus some of one of the dips we list at the bottom will also do it:
You will need
- 1 cup chickpea flour (also called gram flour or garbanzo bean flour)
- 2 tbsp pumpkin seeds
- 1 tbsp chia seeds
- 1 tsp baking powder
- ¼ tsp MSG or ½ tsp low-sodium salt
- 2 tbsp extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Combine the dry ingredients in a mixing bowl, and mix thoroughly.
3) Add the oil, and mix thoroughly.
4) Add water, 1 tbsp at a time, mixing thoroughly until the mixture comes together and you have a dough ball. You’ll probably need 3–4 tbsp in total, but do add them one at a time.
5) Roll out the dough as thinly and evenly as you can between two sheets of baking paper. Remove the top layer of the paper, and slice the dough into squares or triangles. You could use a cookie-cutter to make other shapes if you like, but then you’ll need to repeat the rolling to use up the offcuts. So we recommend squares or triangles at least for your first go.
6) Bake them in the oven for 12–15 minutes or until golden and crispy. Enjoy immediately or keep in an airtight container.
Enjoy!
Want to learn more?
For those interested in some things to go with what we have going on today:
- Muhammara ← this is a very nutritionally-dense dip (not to mention tasty; seriously, check out these flavors)
- Hero Homemade Hummus ← a classic
- Plant-Based Healthy Cream Cheese ← also a very respectable option
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Power of Fun – by Catherine Price
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s said that nobody’s dying regret is to wish they’d spent more time at the office, yet many of don’t make enough time for fun.
This book has been published with two different subtitles:
- Why fun is the key to a happy and healthy life
- How to feel alive again
One offers a sensible reason to read this book; the other offers a deeply emotional reason. Both are entirely valid.
Catherine Price sets out in this work to identify what fun actually is (she puts it at the intersection of playfulness, connection and flow) and how to have more of it (she gives a five-step method to build and integrate it into life).
In the category of criticism, this 334-page book is (in this reviewer’s opinion) a little padded and could have been an article instead. But the advice contained within it is sound, and the impact it can have might be profound.
Bottom line: if you find you’ve settled into a routine that’s perhaps comfortable, but not actually that much fun, this book will help you to liven things up.
Click here to check out The Power Of Fun, and feel more alive!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: