Want to sleep longer? Adding mini-bursts of exercise to your evening routine can help – new study
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Exercising before bed has long been discouraged as the body doesn’t have time to wind down before the lights go out.
But new research has found breaking up a quiet, sedentary evening of watching television with short bursts of resistance exercise can lead to longer periods of sleep.
Adults spend almost one third of the 24-hour day sleeping. But the quality and length of sleep can affect long-term health. Sleeping too little or waking often in the night is associated with an increased risk of heart disease and diabetes.
Physical activity during the day can help improve sleep. However, current recommendations discourage intense exercise before going to bed as it can increase a person’s heart rate and core temperature, which can ultimately disrupt sleep.
Nighttime habits
For many, the longest period of uninterrupted sitting happens at home in the evening. People also usually consume their largest meal during this time (or snack throughout the evening).
Insulin (the hormone that helps to remove sugar from the blood stream) tends to be at a lower level in the evening than in the morning.
Together these factors promote elevated blood sugar levels, which over the long term can be bad for a person’s health.
Our previous research found interrupting evening sitting every 30 minutes with three minutes of resistance exercise reduces the amount of sugar in the bloodstream after eating a meal.
But because sleep guidelines currently discourage exercising in the hours before going to sleep, we wanted to know if frequently performing these short bursts of light activity in the evening would affect sleep.
Activity breaks for better sleep
In our latest research, we asked 30 adults to complete two sessions based in a laboratory.
During one session the adults sat continuously for a four-hour period while watching streaming services. During the other session, they interrupted sitting by performing three minutes of body-weight resistance exercises (squats, calf raises and hip extensions) every 30 minutes.
After these sessions, participants went home to their normal life routines. Their sleep that evening was measured using a wrist monitor.
Our research found the quality of sleep (measured by how many times they woke in the night and the length of these awakenings) was the same after the two sessions. But the night after the participants did the exercise “activity breaks” they slept for almost 30 minutes longer.
Identifying the biological reasons for the extended sleep in our study requires further research.
But regardless of the reason, if activity breaks can extend sleep duration, then getting up and moving at regular intervals in the evening is likely to have clear health benefits.
Time to revisit guidelines
These results add to earlier work suggesting current sleep guidelines, which discourage evening exercise before bed, may need to be reviewed.
As the activity breaks were performed in a highly controlled laboratory environment, future research should explore how activity breaks performed in real life affect peoples sleep.
We selected simple, body-weight exercises to use in this study as they don’t require people to interrupt the show they may be watching, and don’t require a large space or equipment.
If people wanted to incorporate activity breaks in their own evening routines, they could probably get the same benefit from other types of exercise. For example, marching on the spot, walking up and down stairs, or even dancing in the living room.
The key is to frequently interrupt evening sitting time, with a little bit of whole-body movement at regular intervals.
In the long run, performing activity breaks may improve health by improving sleep and post-meal blood sugar levels. The most important thing is to get up frequently and move the body, in a way the works best for a person’s individual household.
Jennifer Gale, PhD candidate, Department of Human Nutrition, University of Otago and Meredith Peddie, Senior Lecturer, Department of Human Nutrition, University of Otago
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Spreading Mental Health Awareness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Request: more people need to be aware of suicidal tendencies and what they can do to ward them off
That’s certainly a very important topic! We’ll cover that properly in one of our Psychology Sunday editions. In the meantime, we’ll mention a previous special that we did, that was mostly about handling depression (in oneself or a loved one), and obviously there’s a degree of crossover:
The Mental Health First-Aid That You’ll Hopefully Never Need
Share This Post
-
Can you get sunburnt or UV skin damage through car or home windows?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When you’re in a car, train or bus, do you choose a seat to avoid being in the sun or do you like the sunny side?
You can definitely feel the sun’s heat through a window. But can you get sunburn or skin damage when in your car or inside with the windows closed?
Let’s look at how much UV (ultraviolet) radiation passes through different types of glass, how tinting can help block UV, and whether we need sunscreen when driving or indoors.
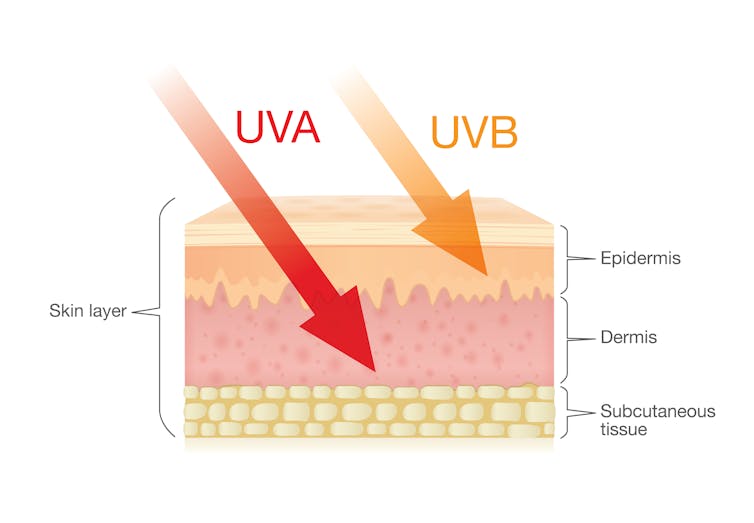
Zac Harris/Unsplash What’s the difference between UVA and UVB?
Of the total UV radiation that reaches Earth, about 95% is UVA and 5% is UVB.
UVB only reaches the upper layers of our skin but is the major cause of sunburn, cataracts and skin cancer.
UVA penetrates deeper into our skin and causes cell damage that leads to skin cancer.
UVA penetrates deeper than UVB. Shutterstock/solar22 Glass blocks UVA and UVB radiation differently
All glass used in house, office and car windows completely blocks UVB from passing through.
But only laminated glass can completely block UVA. UVA can pass through other glass used in car, house and office windows and cause skin damage, increasing the risk of cancer.
Car windscreens block UVA, but the side and rear windows don’t
A car’s front windscreen lets in lots of sunshine and light. Luckily it blocks 98% of UVA radiation because it is made of two layers of laminated glass.
But the side and rear car windows are made of tempered glass, which doesn’t completely block UVA. A study of 29 cars found a range from 4% to almost 56% of UVA passed through the side and rear windows.
The UVA protection was not related to the car’s age or cost, but to the type of glass, its colour and whether it has been tinted or coated in a protective film. Grey or bronze coloured glass, and window tinting, all increase UVA protection. Window tinting blocks around 95% of UVA radiation.
In a separate study from Saudi Arabia, researchers fitted drivers with a wearable radiation monitor. They found drivers were exposed to UV index ratings up to 3.5. (In Australia, sun protection is generally recommended when the UV index is 3 or above – at this level it takes pale skin about 20 minutes to burn.)
So if you have your windows tinted, you should not have to wear sunscreen in the car. But without tinted windows, you can accumulate skin damage.
UV exposure while driving increases skin cancer risk
Many people spend a lot of time in the car – for work, commuting, holiday travel and general transport. Repeated UVA radiation exposure through car side windows might go unnoticed, but it can affect our skin.
Indeed, skin cancer is more common on the driver’s side of the body. A study in the United States (where drivers sit on the left side) found more skin cancers on the left than the right side for the face, scalp, arm and leg, including 20 times more for the arm.
Another US study found this effect was higher in men. For melanoma in situ, an early form of melanoma, 74% of these cancers were on the on the left versus 26% on the right.
Earlier Australian studies reported more skin damage and more skin cancer on the right side.
Cataracts and other eye damage are also more common on the driver’s side of the body.
What about UV exposure through home or office windows?
We see UV damage from sunlight through our home windows in faded materials, furniture or plastics.
Most glass used in residential windows lets a lot of UVA pass through, between 45 and 75%.
Residential windows can let varied amounts of UVA through. Sherman Trotz/Pexels Single-pane glass lets through the most UVA, while thicker, tinted or coated glass blocks more UVA.
The best options are laminated glass, or double-glazed, tinted windows that allow less than 1% of UVA through.
Skylights are made from laminated glass, which completely stops UVA from passing through.
Most office and commercial window glass has better UVA protection than residential windows, allowing less than 25% of UVA transmission. These windows are usually double-glazed and tinted, with reflective properties or UV-absorbent chemicals.
Some smart windows that reduce heat using chemical treatments to darken the glass can also block UVA.
So when should you wear sunscreen and sunglasses?
The biggest risk with skin damage while driving is having the windows down or your arm out the window in direct sun. Even untinted windows will reduce UVA exposure to some extent, so it’s better to have the car window up.
For home windows, window films or tint can increase UVA protection of single pane glass. UVA blocking by glass is similar to protection by sunscreen.
When you need to use sunscreen depends on your skin type, latitude and time of the year. In a car without tinted windows, you could burn after one hour in the middle of the day in summer, and two hours in the middle of a winter’s day.
But in the middle of the day next to a home window that allows more UVA to pass through, it could take only 30 minutes to burn in summer and one hour in winter.
When the UV index is above three, it is recommended you wear protective sunglasses while driving or next to a sunny window to avoid eye damage.
Theresa Larkin, Associate Professor of Medical Sciences, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Can a drug like Ozempic help treat addictions to alcohol, opioids or other substances?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (sold as Ozempic, Wegovy and Rybelsus) was initially developed to treat diabetes. It works by stimulating the production of insulin to keep blood sugar levels in check.
This type of drug is increasingly being prescribed for weight loss, despite the fact it was initially approved for another purpose. Recently, there has been growing interest in another possible use: to treat addiction.
Anecdotal reports from patients taking semaglutide for weight loss suggest it reduces their appetite and craving for food, but surprisingly, it also may reduce their desire to drink alcohol, smoke cigarettes or take other drugs.
But does the research evidence back this up?
Animal studies show positive results
Semaglutide works on glucagon-like peptide-1 receptors and is known as a “GLP-1 agonist”.
Animal studies in rodents and monkeys have been overwhelmingly positive. Studies suggest GLP-1 agonists can reduce drug consumption and the rewarding value of drugs, including alcohol, nicotine, cocaine and opioids.
Out team has reviewed the evidence and found more than 30 different pre-clinical studies have been conducted. The majority show positive results in reducing drug and alcohol consumption or cravings. More than half of these studies focus specifically on alcohol use.
However, translating research evidence from animal models to people living with addiction is challenging. Although these results are promising, it’s still too early to tell if it will be safe and effective in humans with alcohol use disorder, nicotine addiction or another drug dependence.
What about research in humans?
Research findings are mixed in human studies.
Only one large randomised controlled trial has been conducted so far on alcohol. This study of 127 people found no difference between exenatide (a GLP-1 agonist) and placebo (a sham treatment) in reducing alcohol use or heavy drinking over 26 weeks.
In fact, everyone in the study reduced their drinking, both people on active medication and in the placebo group.
However, the authors conducted further analyses to examine changes in drinking in relation to weight. They found there was a reduction in drinking for people who had both alcohol use problems and obesity.
For people who started at a normal weight (BMI less than 30), despite initial reductions in drinking, they observed a rebound increase in levels of heavy drinking after four weeks of medication, with an overall increase in heavy drinking days relative to those who took the placebo.
There were no differences between groups for other measures of drinking, such as cravings.
Some studies show a rebound increase in levels of heavy drinking. Deman/Shutterstock In another 12-week trial, researchers found the GLP-1 agonist dulaglutide did not help to reduce smoking.
However, people receiving GLP-1 agonist dulaglutide drank 29% less alcohol than those on the placebo. Over 90% of people in this study also had obesity.
Smaller studies have looked at GLP-1 agonists short-term for cocaine and opioids, with mixed results.
There are currently many other clinical studies of GLP-1 agonists and alcohol and other addictive disorders underway.
While we await findings from bigger studies, it’s difficult to interpret the conflicting results. These differences in treatment response may come from individual differences that affect addiction, including physical and mental health problems.
Larger studies in broader populations of people will tell us more about whether GLP-1 agonists will work for addiction, and if so, for whom.
How might these drugs work for addiction?
The exact way GLP-1 agonists act are not yet well understood, however in addition to reducing consumption (of food or drugs), they also may reduce cravings.
Animal studies show GLP-1 agonists reduce craving for cocaine and opioids.
This may involve a key are of the brain reward circuit, the ventral striatum, with experimenters showing if they directly administer GLP-1 agonists into this region, rats show reduced “craving” for oxycodone or cocaine, possibly through reducing drug-induced dopamine release.
Using human brain imaging, experimenters can elicit craving by showing images (cues) associated with alcohol. The GLP-1 agonist exenatide reduced brain activity in response to an alcohol cue. Researchers saw reduced brain activity in the ventral striatum and septal areas of the brain, which connect to regions that regulate emotion, like the amygdala.
In studies in humans, it remains unclear whether GLP-1 agonists act directly to reduce cravings for alcohol or other drugs. This needs to be directly assessed in future research, alongside any reductions in use.
Are these drugs safe to use for addiction?
Overall, GLP-1 agonists have been shown to be relatively safe in healthy adults, and in people with diabetes or obesity. However side effects do include nausea, digestive troubles and headaches.
And while some people are OK with losing weight as a side effect, others aren’t. If someone is already underweight, for example, this drug might not be suitable for them.
In addition, very few studies have been conducted in people with addictive disorders. Yet some side effects may be more of an issue in people with addiction. Recent research, for instance, points to a rare risk of pancreatitis associated with GLP-1 agonists, and people with alcohol use problems already have a higher risk of this disorder.
Other drugs treatments are currently available
Although emerging research on GLP-1 agonists for addiction is an exciting development, much more research needs to be done to know the risks and benefits of these GLP-1 agonists for people living with addiction.
In the meantime, existing effective medications for addiction remain under-prescribed. Only about 3% of Australians with alcohol dependence, for example, are prescribed medication treatments such as like naltrexone, acamprosate or disulfiram. We need to ensure current medication treatments are accessible and health providers know how to prescribe them.
Continued innovation in addiction treatment is also essential. Our team is leading research towards other individualised and effective medications for alcohol dependence, while others are investigating treatments for nicotine addiction and other drug dependence.
Read the other articles in The Conversation’s Ozempic series here.
Shalini Arunogiri, Addiction Psychiatrist, Associate Professor, Monash University; Leigh Walker, , Florey Institute of Neuroscience and Mental Health, and Roberta Anversa, , The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Nine Pints – by Rose George
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Rose George is not a scientist, but an investigative journalist. As such, she’s a leave-no-stone-unturned researcher, and that shows here.
The style throughout is, as one might expect, journalistic. But, she’s unafraid of diving into the science of it, interviewing many medical professionals as part of her work. She also looks to people living with various blood-related conditions, ranging from hemophilia to HIV.
Speakling of highly-stigmatized yet very manageable conditions, there’s also a fair section devoted to menstruation, menstrual blood, and societies’ responses to such, from shunning to active support.
We also learn about the industrialization of blood—from blood banks to plasma labs to leech farms. You probably knew leeches are still used as a medical tool in even the most high-tech of hospitals, but you’ll doubtlessly learn a fascinating thing or two from the “insider views” along the way.
Bottom line: if you’d like to know more about the red stuff in all its marvelous aspects, with neither sensationalization nor sanitization (the topic needs neither!), this is the book for you.
Click here to check out Nine Pints, and learn more about yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anticancer: A New Way Of Life – by Dr. David Servan-Schreiber
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A cancer survivor himself, Dr. Servan-Schreiber found himself unimpressed with the advice he was given upon diagnosis, and set out to find better. This, he achieved.
He first provides an introductory overview of cancer, and then devotes most of the book to detailing how to create a “terrain” (the environment of your body and all that you do with/to it) that is hostile to cancer.
This includes things like diet, of course, but also exercise (the right way!), mindset, and much more. He doesn’t cover much about standard medical treatments, as he assumes the reader will already be advised about those by their oncologist, and in any case, such treatments are constantly changing as new discoveries are made. It’s worth mentioning that while he advocates strongly for complementary medicine, he does also make clear it should be just that—complementary—and not a replacement for regular treatments in cases where such are recommended.
The style is comprehensible pop-science, written for the lay reader, and yet with copious scientific references—more than 30 pages thereof. But as well as that, it’s a personal account, often revisiting his own cancer journey to illustrate one point or another, be it something that went well for him or badly, there’s always something to learn.
Bottom line: this book is important for anyone facing cancer, and useful for anyone who simply would like to improve their odds in a more informed fashion. As he notes, “all of us have cancer cells in our bodies, but not all of us will develop cancer”, and it’s good to try to be on the healthiest side of that.
Click here to check out Anticancer, and live an anticancer life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
This Is Your Brain on Food – by Dr. Uma Naidoo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Diet will fix your brain” is a bold claim that often comes from wishful thinking and an optimistic place where anecdote is louder than evidence. But, diet does incontrovertibly also affect brain health. So, what does Dr. Naidoo bring to the table?
The author is a Harvard-trained psychiatrist, a professional chef who graduated with her culinary school’s most coveted award, and a trained-and-certified nutritionist. Between those three qualifications, it’s safe to she knows her stuff when it comes to the niche that is nutritional psychiatry. And it shows.
She takes us through the neurochemistry involved, what chemicals are consumed, made, affected, inhibited, upregulated, etc, what passes through the blood-brain barrier and what doesn’t, what part the gut really plays in its “second brain” role, and how we can leverage that—as well as mythbusting a lot of popular misconceptions about certain foods and moods.
There’s hard science in here, but presented in quite a pop-science way, making for a very light yet informative read.
Bottom line: if you’d like to better understand what your food is doing to your brain (and what it could be doing instead), then this is a top-tier book for you!
Click here to check out This Is Your Brain On Food, and get to know yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: