Waist Size Worries: Age-Appropriate Solutions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝My BMI is fine, but my waist is too big. What do I do about that? I am 5′ 5″ tall and 128 pounds and 72 years old.❞
It’s hard to say without knowing about your lifestyle (and hormones, for that matter)! But, extra weight around the middle in particular is often correlated with high levels of cortisol, so you might find this of benefit:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Savor: Mindful Eating, Mindful Life – by Thich Nhat Hanh and Dr. Lilian Cheung
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked about mindful eating before at 10almonds, so here’s a book about it. You may wonder how much there is to say!
As it happens, there’s quite a bit. The authors, a Buddhist monk (Hanh) and a Harvard nutritionist (Dr. Cheung) explore the role of mindful eating in our life.
There is an expectation that we the reader want to lose weight. If we don’t, those parts of the book will be a “miss” for us, but still contain plenty of other value.
Most of the same advices can be applied equally to other aspects of health, in any case. A lot of that comes from the book’s Buddhist principles, including the notion that:
- We are experiencing suffering
- Suffering has a cause
- What has a cause can have an end
- The way to this end is mindfulness
As such, the process itself is also mindfulness all the way through:
- To be mindful of our suffering (and not let it become background noise to be ignored)
- To be mindful of the cause of our suffering (rather than dismissing it as just how things are)
- To be mindful of how to address that, and thus end the suffering (rather than despairing in inaction)
- To engage mindfully in the process of doing so (and thus not fall into the trap of thinking “job done”)
And, as for Dr. Cheung? She also has input throughout, with practical advice about the more scientific side of rethinking one’s diet.
Bottom line: this is an atypical book, and/but perhaps an important one. Certainly, at the very least it may be one to try if more conventional approaches have failed!
Click here to check out “Savor” on Amazon today, and get mindful!
Share This Post
-
Foods That Cause You to Lose Weight – by Dr. Neal Barnard
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed Dr. Barnard’s “The Power Foods Diet”, and this time his work is about weight loss.
This time there are more recipes (which take up most of the book, so this one could be reasonably described as a cookbook), but not until after nearly a hundred pages of concepts, principles, and tips.
The recipes themselves are again very respectable, even if some may be a little redundant (e.g. the double-page recipe for blueberry muffins is followed by a double-page recipe for banana and date muffins, instead of just saying “or substitute this”—things like that) and run the gamut from salad dressings to hearty main meals.
A strength of the book is that it’s about what you eat, not how much of it you eat, so if you love eating (which is a very healthy trait to have in general), then you’ll enjoy that aspect.
Bottom line: if you’d like to eat more and weigh less, then this is a top-tier book for you.
Click here to check out “Foods That Cause You To Lose Weight”, and enjoy eating!
Share This Post
-
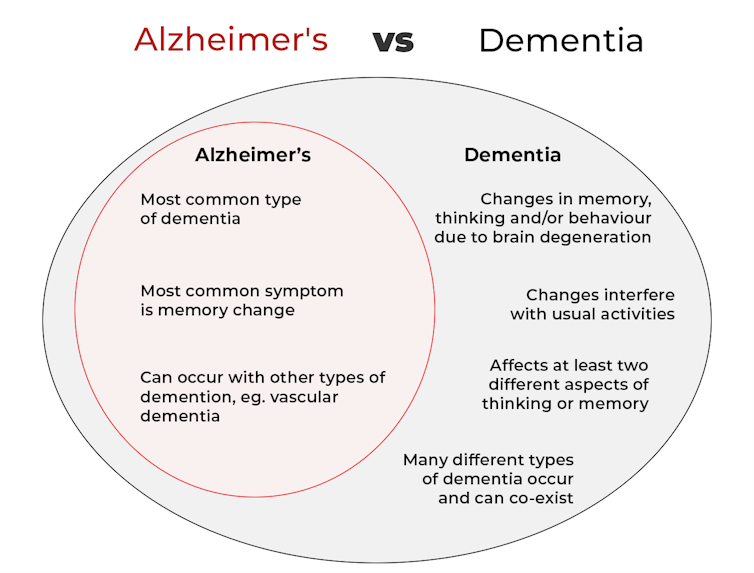
What’s the difference between Alzheimer’s and dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Changes in thinking and memory as we age can occur for a variety of reasons. These changes are not always cause for concern. But when they begin to disrupt daily life, it could indicate the first signs of dementia.
Another term that can crop up when we’re talking about dementia is Alzheimer’s disease, or Alzheimer’s for short.
So what’s the difference?
Lightspring/Shutterstock What is dementia?
Dementia is an umbrella term used to describe a range of syndromes that result in changes in memory, thinking and/or behaviour due to degeneration in the brain.
To meet the criteria for dementia these changes must be sufficiently pronounced to interfere with usual activities and are present in at least two different aspects of thinking or memory.
For example, someone might have trouble remembering to pay bills and become lost in previously familiar areas.
It’s less-well known that dementia can also occur in children. This is due to progressive brain damage associated with more than 100 rare genetic disorders. This can result in similar cognitive changes as we see in adults.
So what’s Alzheimer’s then?
Alzheimer’s is the most common type of dementia, accounting for about 60-80% of cases.
So it’s not surprising many people use the terms dementia and Alzheimer’s interchangeably.
Changes in memory are the most common sign of Alzheimer’s and it’s what the public most often associates with it. For instance, someone with Alzheimer’s may have trouble recalling recent events or keeping track of what day or month it is.
People with dementia may have trouble keeping track of dates. Daisy Daisy/Shutterstock We still don’t know exactly what causes Alzheimer’s. However, we do know it is associated with a build-up in the brain of two types of protein called amyloid-β and tau.
While we all have some amyloid-β, when too much builds up in the brain it clumps together, forming plaques in the spaces between cells. These plaques cause damage (inflammation) to surrounding brain cells and leads to disruption in tau. Tau forms part of the structure of brain cells but in Alzheimer’s tau proteins become “tangled”. This is toxic to the cells, causing them to die. A feedback loop is then thought to occur, triggering production of more amyloid-β and more abnormal tau, perpetuating damage to brain cells.
Alzheimer’s can also occur with other forms of dementia, such as vascular dementia. This combination is the most common example of a mixed dementia.
Vascular dementia
The second most common type of dementia is vascular dementia. This results from disrupted blood flow to the brain.
Because the changes in blood flow can occur throughout the brain, signs of vascular dementia can be more varied than the memory changes typically seen in Alzheimer’s.
For example, vascular dementia may present as general confusion, slowed thinking, or difficulty organising thoughts and actions.
Your risk of vascular dementia is greater if you have heart disease or high blood pressure.
Frontotemporal dementia
Some people may not realise that dementia can also affect behaviour and/or language. We see this in different forms of frontotemporal dementia.
The behavioural variant of frontotemporal dementia is the second most common form (after Alzheimer’s disease) of younger onset dementia (dementia in people under 65).
People living with this may have difficulties in interpreting and appropriately responding to social situations. For example, they may make uncharacteristically rude or offensive comments or invade people’s personal space.
Semantic dementia is also a type of frontotemporal dementia and results in difficulty with understanding the meaning of words and naming everyday objects.
Dementia with Lewy bodies
Dementia with Lewy bodies results from dysregulation of a different type of protein known as α-synuclein. We often see this in people with Parkinson’s disease.
So people with this type of dementia may have altered movement, such as a stooped posture, shuffling walk, and changes in handwriting. Other symptoms include changes in alertness, visual hallucinations and significant disruption to sleep.
Do I have dementia and if so, which type?
If you or someone close to you is concerned, the first thing to do is to speak to your GP. They will likely ask you some questions about your medical history and what changes you have noticed.
Sometimes it might not be clear if you have dementia when you first speak to your doctor. They may suggest you watch for changes or they may refer you to a specialist for further tests.
There is no single test to clearly show if you have dementia, or the type of dementia. A diagnosis comes after multiple tests, including brain scans, tests of memory and thinking, and consideration of how these changes impact your daily life.
Not knowing what is happening can be a challenging time so it is important to speak to someone about how you are feeling or to reach out to support services.
Dementia is diverse
As well as the different forms of dementia, everyone experiences dementia in different ways. For example, the speed dementia progresses varies a lot from person to person. Some people will continue to live well with dementia for some time while others may decline more quickly.
There is still significant stigma surrounding dementia. So by learning more about the various types of dementia and understanding differences in how dementia progresses we can all do our part to create a more dementia-friendly community.
The National Dementia Helpline (1800 100 500) provides information and support for people living with dementia and their carers. To learn more about dementia, you can take this free online course.
Nikki-Anne Wilson, Postdoctoral Research Fellow, Neuroscience Research Australia (NeuRA), UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Can a drug like Ozempic help treat addictions to alcohol, opioids or other substances?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Semaglutide (sold as Ozempic, Wegovy and Rybelsus) was initially developed to treat diabetes. It works by stimulating the production of insulin to keep blood sugar levels in check.
This type of drug is increasingly being prescribed for weight loss, despite the fact it was initially approved for another purpose. Recently, there has been growing interest in another possible use: to treat addiction.
Anecdotal reports from patients taking semaglutide for weight loss suggest it reduces their appetite and craving for food, but surprisingly, it also may reduce their desire to drink alcohol, smoke cigarettes or take other drugs.
But does the research evidence back this up?
Animal studies show positive results
Semaglutide works on glucagon-like peptide-1 receptors and is known as a “GLP-1 agonist”.
Animal studies in rodents and monkeys have been overwhelmingly positive. Studies suggest GLP-1 agonists can reduce drug consumption and the rewarding value of drugs, including alcohol, nicotine, cocaine and opioids.
Out team has reviewed the evidence and found more than 30 different pre-clinical studies have been conducted. The majority show positive results in reducing drug and alcohol consumption or cravings. More than half of these studies focus specifically on alcohol use.
However, translating research evidence from animal models to people living with addiction is challenging. Although these results are promising, it’s still too early to tell if it will be safe and effective in humans with alcohol use disorder, nicotine addiction or another drug dependence.
What about research in humans?
Research findings are mixed in human studies.
Only one large randomised controlled trial has been conducted so far on alcohol. This study of 127 people found no difference between exenatide (a GLP-1 agonist) and placebo (a sham treatment) in reducing alcohol use or heavy drinking over 26 weeks.
In fact, everyone in the study reduced their drinking, both people on active medication and in the placebo group.
However, the authors conducted further analyses to examine changes in drinking in relation to weight. They found there was a reduction in drinking for people who had both alcohol use problems and obesity.
For people who started at a normal weight (BMI less than 30), despite initial reductions in drinking, they observed a rebound increase in levels of heavy drinking after four weeks of medication, with an overall increase in heavy drinking days relative to those who took the placebo.
There were no differences between groups for other measures of drinking, such as cravings.
Some studies show a rebound increase in levels of heavy drinking. Deman/Shutterstock In another 12-week trial, researchers found the GLP-1 agonist dulaglutide did not help to reduce smoking.
However, people receiving GLP-1 agonist dulaglutide drank 29% less alcohol than those on the placebo. Over 90% of people in this study also had obesity.
Smaller studies have looked at GLP-1 agonists short-term for cocaine and opioids, with mixed results.
There are currently many other clinical studies of GLP-1 agonists and alcohol and other addictive disorders underway.
While we await findings from bigger studies, it’s difficult to interpret the conflicting results. These differences in treatment response may come from individual differences that affect addiction, including physical and mental health problems.
Larger studies in broader populations of people will tell us more about whether GLP-1 agonists will work for addiction, and if so, for whom.
How might these drugs work for addiction?
The exact way GLP-1 agonists act are not yet well understood, however in addition to reducing consumption (of food or drugs), they also may reduce cravings.
Animal studies show GLP-1 agonists reduce craving for cocaine and opioids.
This may involve a key are of the brain reward circuit, the ventral striatum, with experimenters showing if they directly administer GLP-1 agonists into this region, rats show reduced “craving” for oxycodone or cocaine, possibly through reducing drug-induced dopamine release.
Using human brain imaging, experimenters can elicit craving by showing images (cues) associated with alcohol. The GLP-1 agonist exenatide reduced brain activity in response to an alcohol cue. Researchers saw reduced brain activity in the ventral striatum and septal areas of the brain, which connect to regions that regulate emotion, like the amygdala.
In studies in humans, it remains unclear whether GLP-1 agonists act directly to reduce cravings for alcohol or other drugs. This needs to be directly assessed in future research, alongside any reductions in use.
Are these drugs safe to use for addiction?
Overall, GLP-1 agonists have been shown to be relatively safe in healthy adults, and in people with diabetes or obesity. However side effects do include nausea, digestive troubles and headaches.
And while some people are OK with losing weight as a side effect, others aren’t. If someone is already underweight, for example, this drug might not be suitable for them.
In addition, very few studies have been conducted in people with addictive disorders. Yet some side effects may be more of an issue in people with addiction. Recent research, for instance, points to a rare risk of pancreatitis associated with GLP-1 agonists, and people with alcohol use problems already have a higher risk of this disorder.
Other drugs treatments are currently available
Although emerging research on GLP-1 agonists for addiction is an exciting development, much more research needs to be done to know the risks and benefits of these GLP-1 agonists for people living with addiction.
In the meantime, existing effective medications for addiction remain under-prescribed. Only about 3% of Australians with alcohol dependence, for example, are prescribed medication treatments such as like naltrexone, acamprosate or disulfiram. We need to ensure current medication treatments are accessible and health providers know how to prescribe them.
Continued innovation in addiction treatment is also essential. Our team is leading research towards other individualised and effective medications for alcohol dependence, while others are investigating treatments for nicotine addiction and other drug dependence.
Read the other articles in The Conversation’s Ozempic series here.
Shalini Arunogiri, Addiction Psychiatrist, Associate Professor, Monash University; Leigh Walker, , Florey Institute of Neuroscience and Mental Health, and Roberta Anversa, , The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Teenage Brain – by Dr. Frances Jensen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We realize that we probably have more grandparents of teenagers than parents of teenagers here, but most of us have at least some teenage relative(s). Which makes this book interesting.
There are a lot of myths about the teenage brain, and a lot of popular assumptions that usually have some basis in fact but are often misleading.
Dr. Jensen gives us a strong foundational grounding in the neurophysiology of adolescence, from the obvious-but-often-unclear (such as the role of hormones) to less-known things like the teenage brain’s general lack of myelination. Not just “heightened neuroplasticity” but, if you imagine the brain as an electrical machine, then think of myelin as the insulation between the wires. Little wonder some wires may get crossed sometimes!
She also talks about such things as the teenage circadian rhythm’s innate differences, the impact of success and failure on the brain, and harder topics such as addiction—and the adolescent cortisol functions that can lead to teenagers needing to seek something to relax in the first place.
In criticism, we can only say that sometimes the author makes sweeping generalizations without acknowledging such, but that doesn’t detract from what she has to say on the topic of neurophysiology.
Bottom line: if there’s a teenager in your life whose behavior and/or moods are sometimes baffling to you, and whose mysteries you’d like to unravel, this is a great book.
Click here to check out the Teenage Brain, and better understand those around you!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Turmeric (Curcumin) Dos and Don’ts With Dr. Kim
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Turmeric is a fabulous spice, most well-known for its anti-inflammatory powers; its antioxidant effects benefit all of the body, including the brain. While it fights seemingly everything from arthritis to atherosclerosis to Alzheimer’s and more, it also boosts brain-derived neurotrophic factor, looks after your cardiovascular health, holds back diabetes, reduces the risk of cancer, fights depression, slows aging, and basically does everything short of making you sing well too.
Dr. Leonid Kim goes over the scientific evidence for these, and also talks about some of the practicalities of taking turmeric, and safety considerations.
For the most part, turmeric is very safe even at high doses (up to 8g at least); indeed, at smaller doses (e.g. 500mg) it largely does the same job as non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, with fewer problems.
It also does the job of several antidiabetic medications, by increasing uptake of glucose (thus reducing blood sugar levels) while simultaneously decreasing the glucose secretion from the liver. It does this by regulating the AMPK signalling pathway, just like metformin—while again, being safer.
Dr. Kim also looks at the (good!) evidence for turmeric in managing PCOS and undoing NAFLD; so far, so good.
Dosage: he bids us pay attention whether we’re taking it as turmeric itself or as curcumin standardized extract. The latter is the active compound, and in principle more powerful, but in practice it can get metabolized too quickly and easily—before it can have its desired effect. So, turmeric itself is a very good choice.
Absorption: since we do want it to be absorbed well, though, he does recommend taking it with piperine (as in black pepper).
You may be thinking: isn’t this going to cause the same problem you were just talking about, and cause it to be metabolized too quickly? And the answer is: no! How piperine works is almost the opposite; it protects the curcumin in the turmeric from our digestive enzymes, and thus allows them to get absorbed without being broken down too quickly—thus increasing the bioavailability by slowing the process down.
Lipophilia: no, that’s not a disease (or a fetish), rather it means that curcumin is soluble in fats, so we should take it near in time to a meal that contains at least a tablespoon of oil in total (so if you’re cooking a curry with your turmeric, this need is covered already, for example).
Supplement provenance: he recommends picking a supplement that’s been tested by a reputable 3rd party, as otherwise turmeric can be quite prone to impurities (which can include lead and arsenic, so, not great).
Contraindications: for some people, curcumin can cause gastrointestinal issues (less likely if taking with meals), and also, it can interact with blood-thinners. While taking aspirin or curcumin alone might help avoid circulatory problems, taking both could increase the bleeding risk for some people, for example. Similarly, if taking curcumin and metformin while diabetic, one must watch out for the combination being too effective at lowering blood sugar levels, and thus causing hypoglycemia instead. Similar deal with blood pressure medications.
There’s more in the video though (yes really; we know we wrote a lot but it’s information-dense), so do check it out:
Click Here If The Embedded Video Doesn’t Load Automatically
Want to know more?
You can also check out our related articles:
Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Black Pepper’s Impressive Anti-Cancer Arsenal (And More)Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: