Vibration Plate, Review After 6 Months: Is It Worth It?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is it push-button exercise, or an expensive fad, or something else entirely? Robin, from “The Science of Self-Care”, has insights:
Science & Experience
According to the science (studies cited in the video and linked-to in the video description, underneath it on YouTube), vibration therapy does have some clear benefits, namely:
- Bone health (helps with bone density, particularly beneficial for postmenopausal women)
- Muscle recovery (reduces lactate levels, aiding faster recovery)
- Joint health (reduces pain and improves function in osteoarthritis patients)
- Muscle stimulation (helps older adults maintain muscle mass)
- Cognitive function (due to increased blood flow to the brain)
And from her personal experience, the benefits included:
- Improved recovery after exercise, reducing muscle soreness and stiffness
- Reduced back pain and improved posture (not surprising, given the need for stabilizing muscles when using one of these)
- Better circulation and (likely resulting from same) skin clarity
She did not, however, notice:
- Any reduction in cellulite
- Any change in body composition (fat loss or muscle gain)
For a deeper look into these things and more, plus a demonstration of how the machine actually operates, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How to Permanently Loosen a Tight Psoas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Is Your Psoas?
Your psoas is a deep muscle in your lower back and hip area that connects your spine to your thigh bone. It helps you bend your hips and spine, making it a hip flexor.
In today’s video, Your Wellness Nerd (the YouTube channel behind the video below) has revealed some great tips on loosening said tight hip flexors!
How to loosen them
First off, the big reveal…your tight psoas is likely stemming from an overlooked cause: your lower back! The video kicks off with a simple technique to loosen up that stiff area in your lower back. All you need is a foam roller.
But, before diving into the exercises, it’s essential to gauge your current flexibility. A basic hip flexor stretch serves as a pre-test.
Note: the goal here isn’t to stretch, but rather to feel how tight you are.
After testing, it’s time to roll…literally. Working through the lower back, use your roller or tennis ball to any find stiff spots and loosen them out; those spots are likely increasing the tension on your psoas.
After some rolling, retest with the hip flexor stretch. Chances are, you’ll feel more mobility and less tightness right away.
Note: this video focuses on chronic psoas issues. If you have sore psoas from a muscular workout, you may want to read our piece on speeding up muscle recovery.
Is That All?
But wait, there’s more! The video also covers two more exercises specifically targeting the psoas. This one’s hard to describe, so we recommend watching the video. However, to provide an overview, you’re doing the “classic couch stretch”, but with a few alterations.
Next, the tennis ball technique zeroes in on specific tight spots in the psoas. By lying on the ball and adjusting its position around the hip area, you can likely release some deeply held tension.
Additionally, some of our readers advocate for acupuncture for psoas relief – we’ve done an acupuncture myth-busting article here for reference.
Other Sources
If you’re looking for some more in-depth guides on stretching your psoas, and your body in general, we’ve made a range of 1-minute summaries of books that specifically target stretching:
- 11 Minutes to Pain-Free Hips (perfect for psoas muscles)
- Stretching Scientifically
- Stretching & Mobility
- Stretching to Stay Young
The final takeaway? If you’re constantly battling tight psoas muscles despite trying different exercises and stretches, it might be time to look at your lower back and your daily habits. This video isn’t just a band-aid fix; it’s about addressing the root cause for long-term relief:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Calm Your Inflammation – by Dr. Brenda Tidwell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book starts with an overview of inflammation, both acute and chronic, before diving into how to reduce the latter kind (acute inflammation being usually necessary and helpful, usually fighting disease rather than creating it).
The advice in the book is not just dietary, and covers lifestyle interventions too, including exercise etc—and how to strike the right balance, since the wrong kind of exercise or too much of it can sabotage our efforts. Similarly, Dr. Tidwell doesn’t just say such things as “manage stress” but also provides 10 ways of doing so, and so forth for other vectors of inflammation-control. She does cover dietary things as well though, including supplements where applicable, and the role of gut health, sleep, and other factors.
The style of the book is quite entry-level pop-science, designed to be readable and comprehensible to all, without unduly dumbing-down. In terms of hard science or jargon, there are 6 pages of bibliography and 3 pages of glossary, so it’s neither devoid of such nor overwhelmed by it.
Bottom line: if fighting inflammation is a priority for you, then this book is an excellent primer.
Click here to check out Calm Your Inflammation, and indeed calm your inflammation!
Share This Post
-
Overcome Front-Of-Hip Pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Alyssa Kuhn, physiotherapist, demonstrates how:
One, two, three…
One kind of pain affects a lot of related things: hip pain has an impact on everything that’s connected to the pelvis, which is basically the rest of the body, but especially the spine itself. For this reason, it’s critical to keep it in as good condition as possible.
Two primary causes of hip stiffness and pain:
- Anterior pelvic tilt due to posture, weight distribution, or pain. This tightens the front muscles and weakens the back muscles.
- Prolonged sitting, which tightens the hip muscles due to inactivity.
Three exercises are recommended by Dr. Kuhn to relieve pain and stiffness:
- Bridge exercise:
- Lie on a firm surface with your knees bent.
- Push through your feet, engage your hamstrings, and flatten your lower back.
- Hold for 3–5 seconds, relax, and repeat (10–20 reps).
- Wall exercise with arms:
- Stand with your lower back against the wall, feet a step away.
- Tilt your hips backwards, keeping your lower back in contact with the wall.
- Alternate lifting one arm at a time while maintaining back contact with the wall (10–20 reps).
- Wall exercise with legs:
- Same stance as the previous exercise but wider now.
- Lift one heel at a time while keeping your hips stable and your back against the wall.
- Practice for 30–60 seconds, maintaining good form.
As ever, consistency is key for long-term relief. Dr. Kuhn recommends doing these regularly, especially before any expected periods of prolonged sitting (e.g. at desk, or driving, etc). And of course, do try to reduce, or at least break up, those sitting marathons if you can.
For more on all of this plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
The Unchaste Berry
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Chasteberry, By Any Other Name…
Vitex agnus castus, literally “chaste lamb vine”, hence its modern common English name “chasteberry”, gets its name from its traditional use as an anaphrodisiac for monks (indeed, it’s also called “monk’s pepper”), which traditional use is not in the slightest backed up by modern science.
Nor is its second most popular traditional use (the increase in production of milk) well-supported by science either:
❝Its traditional use as a galactagogue (i.e., a substance that enhances breast milk production) is not well supported in the literature and should be discouraged. There are no clinical data to support the use of chasteberry for reducing sexual desire, which has been a traditional application❞
Source: American Family Physician | Chasteberry
Both of those supposed effects of the chasteberry go against the fact that it has a prolactin-lowering effect:
❝It appears that [chasteberry] may represent a potentially useful and safe phytotherapic option for the management of selected patients with mild hyperprolactinaemia who wish to be treated with phytotherapy.❞
Source: Vitex agnus castus effects on hyperprolactinaemia
Prolactin, by the way, is the hormone that (as the name suggests) stimulates milk production, and also reduces sexual desire (and motivation in general)
- In most women, it spikes during breastfeeding
- In most men, it spikes after orgasm
- In both, it can promote anhedonic depression, as it antagonizes dopamine
In other words, the actual pharmacological effect of chasteberry, when it comes to prolactin, is the opposite of what we would expect from its traditional use.
Ok, so it’s an unchaste berry after all…. Does it have any other claims to examine?
Yes! It genuinely does help relieve PMS, for those who have it, and reduce menopause symptoms, for those who have those, for example:
❝Dry extract of agnus castus fruit is an effective and well tolerated treatment for the relief of symptoms of the premenstrual syndrome.❞
❝That [Vitex agnus castus] trial indicated strong symptomatic relief of common menopausal symptoms❞
Source: Vitex agnus castus essential oil and menopausal balance: a research update
Is it safe?
Generally speaking, yes. It has been described as “well-tolerated” in the studies we mentioned above, which means it has a good safety profile.
However, it may interfere with some antipsychotic medications, certain kinds of hormone replacement therapy, or hormonal birth control.
As ever, speak with your doctor/pharmacist if unsure!
Where can I get some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Little Treatments, Big Effects – by Dr. Jessica Schleider
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a clinical psychologist, discusses how mental healthcare has come a very long way, yet still has a long way to go. While advocating for top-down reforms, she does have a stopgap solution:
Find ways to significantly improve people’s mental health in a single-session intervention.
This seems like a tall order, but her method is based on good science, and also, most people will agree from experience that big changes can happen to someone in the space of moments, at pivotal turning points in life—they just have to be the right moments.
Dr. Schleider recommends that therapists train in (and then offer) this method, but she does also give comprehensive advice for self-therapy of this kind too.
These self-therapy directions, ways to induce those life-pivoting moments for the better, are perhaps the greatest value that the book gives us.
Bottom line: if you’d like a lot of the benefits of therapy without getting therapy, this book can definitely point you in the right direction, in a manner that won’t be a drain on your time or your wallet.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Detox: What’s Real, What’s Not, What’s Useful, What’s Dangerous?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Detox: What’s Real, What’s Not, What’s Useful, What’s Dangerous?
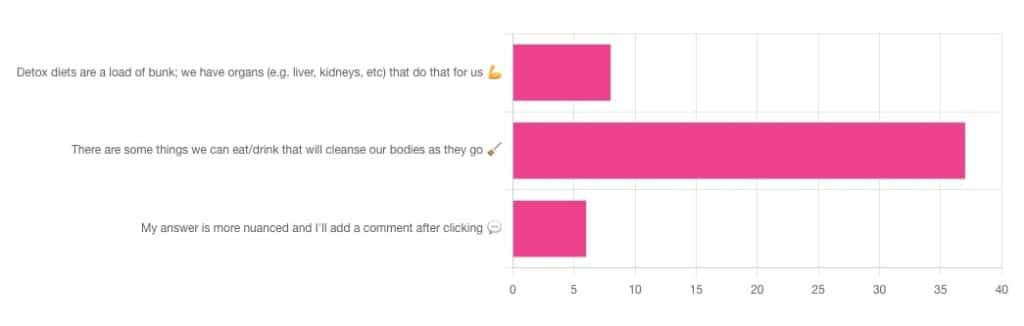
Out of the subscribers who engaged in the poll, it looks like we have a lot of confidence in at least some detox approaches being useful!
Celery juice is most people’s go-to, and indeed it was the only one to get mentioned in the comments added. So let’s take a look at that first…
Celery juice
Celery juice is enjoyed by many people, with many health benefits in mind, including to:
- reduce inflammation
- lower blood pressure
- heal the liver
- fight cancer
- reduce bloating
- support the digestive system
- increase energy
- support weight loss
- promote good mental health
An impressive list! With such an impressive list, we would hope for an impressive weight of evidence, so regular readers might be wondering why those bullet-pointed items aren’t all shiny hyperlinks to studies backing those claims. The reason is…
There aren’t any high-quality studies that back any of those claims.
We found one case study (so, a study with a sample size of one; not amazing) that observed a blood pressure change in an elderly man after drinking celery juice.
Rather than trawl up half of PubMed to show the lacklustre results in a way more befitting of Research Review Monday, though, here’s a nice compact article detailing the litany of disappointment that is science’s observations regards celery juice:
Why Are People Juicing Their Celery? – by Allison Webster, PhD, RD
A key take-away is: juicing destroys the fiber that is celery’s biggest benefit, and its phytochemicals are largely unproven to be of use.
If you enjoy celery, great! It (when not juiced) is a great source of fiber and water. If you juice it, it’s a great source of water.
Activated Charcoal
Unlike a lot of greenery—whose “cleansing” benefits mostly come from fiber and disappear when juiced—activated charcoal has a very different way of operating.
Activated charcoal is negatively charged on a molecular level*, and that—along with its porous nature—traps toxins. It really is a superpowered detox that actually works very well indeed.
But…
It works very well indeed. It will draw out toxins so well, that it’s commonly used to treat poisonings. “Wait”, we hear you say, “why was that a but”?
It doesn’t know what a toxin is. It just draws out all of the things. You took medicine recently? Not any more you didn’t. You didn’t even take that medication orally, you took it some other way? Activated charcoal does not care:
- The effect of activated charcoal on drug exposure following intravenous administration: A meta-analysis
- Activated charcoal for acute overdose: a reappraisal
Does this mean that activated charcoal can be used to “undo” a night of heavy drinking?
Sadly not. That’s one of the few things it just doesn’t work for. It won’t work for alcohol, salts, or metals:
The Use of Activated Charcoal to Treat Intoxications
*Fun chemistry mnemonic about ions:
Cations are pussitive
Anions (by process of elimination) are negative
Onions taste good in salad (remember also: Cole’s Law)
Bottom line on detox foods/drinks:
- Fiber is great; juicing removes fiber. Eat your greens (don’t drink them)!
- Activated charcoal is the heavy artillery of detoxing
- Sometimes it will remove things you didn’t want removed, though
- It also won’t help against alcohol, sadly
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: