When should you get the updated COVID-19 vaccine?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Updated COVID-19 vaccines are now available: They’re meant to give you the best protection against the strain of the virus that is making people severely sick and also causing deaths.
Many people were infected during the persistent summer wave, which may leave you wondering when you should get the updated vaccine. The short answer is that it depends on when you last got infected or vaccinated and on your particular level of risk.
We heard from six experts—including medical doctors and epidemiologists—about when they recommend getting an updated vaccine. Read on to learn what they said. And to make it easy, check out the flowchart below.

If I was infected with COVID-19 this summer, when should I get the updated vaccine?
All the experts we spoke to agreed that if you were infected this summer, you should wait at least three months since you were infected to get vaccinated.
“Generally, an infection may be protective for about three months,” Dr. Ziyad Al-Aly, chief of research and development at the Veterans Affairs St. Louis Health Care System, tells PGN. “If they got infected three or more months ago, it is a good idea to get vaccinated sooner than later.”
This three-month rule applies if you got vaccinated over the summer, which may be the case for some immunocompromised people, adds Dr. Peter Chin-Hong, professor of medicine at the University of California, San Francisco.
If I didn’t get infected with COVID-19 this summer, when should I get vaccinated?
Most of the experts we talked to say that if you didn’t get infected with COVID-19 this summer, you should get the vaccine as soon as possible. Dr. Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine, emphasizes that if this applies to you, you should get vaccinated as soon as possible, especially given the current COVID-19 surge.
Al-Aly agrees. “Vaccine-derived immunity lasts for several months, and it should cover the winter season. Plus, the current vaccine is a KP.2-adapted vaccine, so it will work most optimally against KP.2 and related subvariants [such as] KP.3 that are circulating now,” Al-Aly says. “We don’t know when the virus will mutate to a variant that is not compatible with the KP.2 vaccine.”
Al-Aly adds that if you’d rather take the protection you can get right now, “It may make more sense to get vaccinated sooner than later.”
This especially applies if you’re over 65 or immunocompromised and you haven’t received a COVID-19 vaccine in a year or more because, as Chin-Hong adds, “that is the group that is being hospitalized and disproportionately dying now.”
Some experts—including epidemiologist Katelyn Jetelina, author of newsletter Your Local Epidemiologist—also say that if you’re younger than 65 and not immunocompromised, you can consider waiting and aiming to get vaccinated before Halloween to get the best protection in the winter, when we’re likely to experience another wave because of the colder weather, gathering indoors, and the holidays.
“I am more worried about the winter than the summer, so I would think of October (some time before Halloween) as the ‘Goldilocks moment’—not too early, not too late, but just right,” Chin-Hong adds. Time it “such that your antibodies peak during the winter when COVID-19 cases are expected to exceed what we are seeing this summer.”
My children are starting school—should I get them vaccinated now?
According to most experts we spoke to, now is a good time to get your children vaccinated.
Jennifer Nuzzo, professor of epidemiology and director of the Pandemic Center at the Brown University School of Public Health, adds that “with COVID-19 infection levels as high as they are and increased exposures in school,” now is a particularly good time to get an updated vaccine if people haven’t gotten COVID-19 recently.
Additionally, respiratory viruses spike when kids are back in school, so “doing everything you can to reduce your child’s risk of infection can help protect families and communities,” says epidemiologist Jessica Malaty Rivera, science communications advisor at the de Beaumont Foundation.
For more information, talk to your health care provider.
(Disclosure: The de Beaumont Foundation is a partner of The Public Good Projects, the organization that owns Public Good News.)
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oscar contender Poor Things is a film about disability. Why won’t more people say so?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Readers are advised this article includes an offensive and outdated disability term in a quote from the film.
Poor Things is a spectacular film that has garnered critical praise, scooped up awards and has 11 Oscar nominations. That might be the problem. Audiences become absorbed in another world, so much so our usual frames of reference disappear.
There has been much discussion about the film’s feminist potential (or betrayal). What’s not being talked about in mainstream reviews is disability. This seems strange when two of the film’s main characters are disabled.
Set in a fantasy version of Victorian London, unorthodox Dr Godwin Baxter (William Dafoe) finds the just-dead body of a heavily pregnant woman in the Thames River. In keeping with his menagerie of hybrid animals, Godwin removes the unborn baby’s brain and puts it into the skull of its mother, who becomes Bella Baxter (Emma Stone).
Is Bella really disabled?
Stone has been praised for her ability to embody a small child who rapidly matures into a hypersexual person – one who has not had time to absorb the restrictive rules of gender or patriarchy.
But we also see a woman using her behaviour to express herself because she has complex communication barriers. We see a woman who is highly sensitive and responsive to the sensory world around her. A woman moving through and seeing the world differently – just like the fish-eye lens used in many scenes.
Women like this exist and they have historically been confined, studied and monitored like Bella. When medical student Max McCandless (Ramy Youssef) first meets Bella, he offensively exclaims “what a very pretty retard!” before being told the truth and promptly declared her future husband.
Even if Bella is not coded as disabled through her movements, speech and behaviour, her onscreen creator and guardian is. Godwin Baxter has facial differences and other impairments which require assistive technology.
So ignoring disability as a theme of the film seems determined and overt. The absurd humour for which the film is being lauded is often at Bella’s “primitive”, “monstrous” or “damaged” actions: words which aren’t usually used to describe children, but have been used to describe disabled people throughout history.
In reviews, Bella’s walk and speech are compared to characters like the Scarecrow in The Wizard of Oz, rather than a disabled woman. So why the resistance?
Freak shows and displays
Disability studies scholar Rosemarie Gardland-Thomson writes “the history of disabled people in the Western world is in part the history of being on display”.
In the 19th century, when Poor Things is set, “freak shows” featuring disabled people, Indigenous people and others with bodily differences were extremely popular.
Doctors used freak shows to find specimens – like Joseph Merrick (also known as the Elephant Man and later depicted on screen) who was used for entertainment before he was exhibited in lecture halls. In the mid-1800s, as medicine became a profession, observing the disabled body shifted from a public spectacle to a private medical gaze that labelled disability as “sick” and pathologised it.
Poor Things doesn’t just circle around these discourses of disability. Bella’s body is a medical experiment, kept locked away for the private viewing of male doctors who take notes about her every move in small pads. While there is something glorious, intimate and familiar about Bella’s discovery of her own sexual pleasure, she immediately recognises it as worth recording in the third person:
I’ve discovered something that I must share […] Bella discover happy when she want!
The film’s narrative arc ends with Bella herself training to be a doctor but one whose more visible disabilities have disappeared.
Framing charity and sexual abuse
Even the film’s title is an expression often used to describe disabled people. The charity model of disability sees disabled people as needing pity and support from others. Financial poverty is briefly shown at a far-off port in the film and Bella initially becomes a sex worker in Paris for money – but her more pressing concern is sexual pleasure.
Disabled women’s sexuality is usually seen as something that needs to be controlled. It is frequently assumed disabled women are either hypersexual or de-gendered and sexually innocent.
In the real world disabled people experience much higher rates of abuse, including sexual assault, than others. Last year’s Royal Commission into Violence, Abuse, Neglect and Exploitation of People with Disability found women with disability are nearly twice as likely as women without disability to have been assaulted. Almost a third of women with disability have experienced sexual assault by the age of 15. Bella’s hypersexual curiosity appears to give her some layer of protection – but that portrayal denies the lived experience of many.
Watch but don’t ignore
Poor Things is a stunning film. But ignoring disability in the production ignores the ways in which the representation of disabled bodies play into deep and historical stereotypes about disabled people.
These representations continue to shape lives.
Louisa Smith, Senior lecturer, Deakin University; Gemma Digby, Lecturer – Health & Social Development, Deakin University, and Shane Clifton, Associate Professor of Practice, School of Health Sciences and the Centre for Disability Research and Policy, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Keep Your Mind From Wandering
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether your mind keeps wandering more as you get older, or you’re a young student whose super-active brain is more suited to TikTok than your assigned reading, sustained singular focus can be a challenge for everyone—and yet (alas!) it remains a required skill for so much in life.
Today’s edition of 10Almonds presents a nifty trick to get yourself through those tasks! We’ll also be taking some time to reply to your questions and comments, in our weekly interactive Q&A.
First of all though, we’ve a promise to make good on, so…
How To Stay On The Ball (Or The Tomato?) The Easy Way
For most of us, we face three main problems when it comes to tackling our to-dos:
- Where to start?
- The task seems intimidating in its size
- We get distracted and/or run out of energy
If you’re really not sure where to start, we recommended a powerful tool in last Friday’s newsletter!
For the rest, we love the Pomodoro Technique:
- Set a timer for 25 minutes, and begin your task.
- Keep going until the timer is done! No other tasks, just focus.
- Take a 5-minute break.
- Repeat
This approach has three clear benefits:
- No matter the size of the task, you are only committing to 25 minutes—everything is much less overwhelming when there’s an end in sight!
- Being only 25 minutes means we are much more likely to stay on track; it’s easier to defer other activities if we know that there will be a 5-minute break for that soon.
- Even without other tasks to distract us, it can be difficult to sustain attention for long periods; making it only 25 minutes at a time allows us to approach it with a (relatively!) fresh mind.
Have you heard that a human brain can sustain attention for only about 40 minutes before focus starts to decline rapidly?
While that’s been a popular rationale for school classroom lesson durations (and perhaps coincidentally ties in with Zoom’s 40-minute limit for free meetings), the truth is that focus starts dropping immediately, to the point that one-minute attention tests are considered sufficient to measure the ability to focus.
So a 25-minute Pomodoro is a more than fair compromise!
Why’s it called the “Pomodoro” technique?
And why is the 25-minute timed work period called a Pomodoro?
It’s because back in the 80s, university student Francesco Cirillo was struggling to focus and made a deal with himself to focus just for a short burst at a time—and he used a (now “retro” style) kitchen timer in the shape of a tomato, or “pomodoro”, in Italian.
If you don’t have a penchant for kitsch kitchenware, you can use this free, simple Online Pomodoro Timer!
(no registration/login/download necessary; it’s all right there on the web page)
Share This Post
-
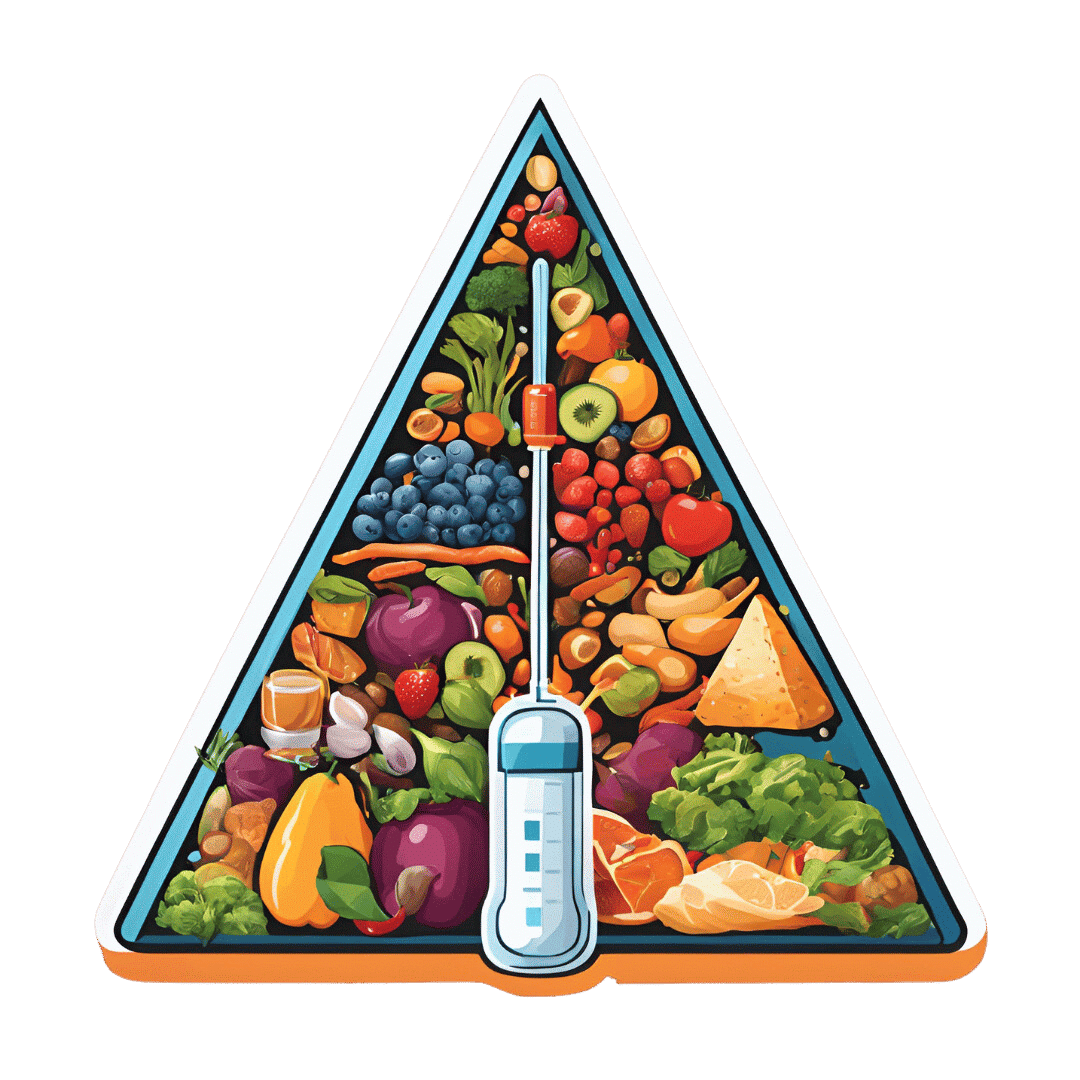
The Great Cholesterol Myth, Revised and Expanded – by Dr. Jonny Bowden and Dr. Stephen Sinatra
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The topic of cholesterol, and saturated fat for that matter, is a complex and often controversial one. How does this book treat it?
With strong opinions, is how—but backed by good science. The authors, a nutritionist and a cardiologist, pull no punches about outdated and/or cherry-picked science, and instead make the case for looking at what, statistically speaking, appear to be the real strongest risk factors.
So, are they advocating for Dave Asprey-style butter-guzzling, or “the carnivore diet”? No, no they are not. Those things remain unhealthy, even if they give some short-term gains (of energy levels, weight loss, etc).
They do advocate, however, for enjoying saturated fats in moderation, and instead of certain polyunsaturated seed oils that do far worse. They also advocate strongly for avoiding sugar, stress, and (for different reasons) statins (in most people’s cases).
They also demystify in clear terms, and often with diagrams and infographics, the various kinds of fats and their components, broken down in far more detail than any other pop-science source this reviewer has seen.
Bottom line: if you want to take a scientific approach to heart health, this book can help you to focus on what will actually make the biggest difference.
Share This Post
Related Posts
-
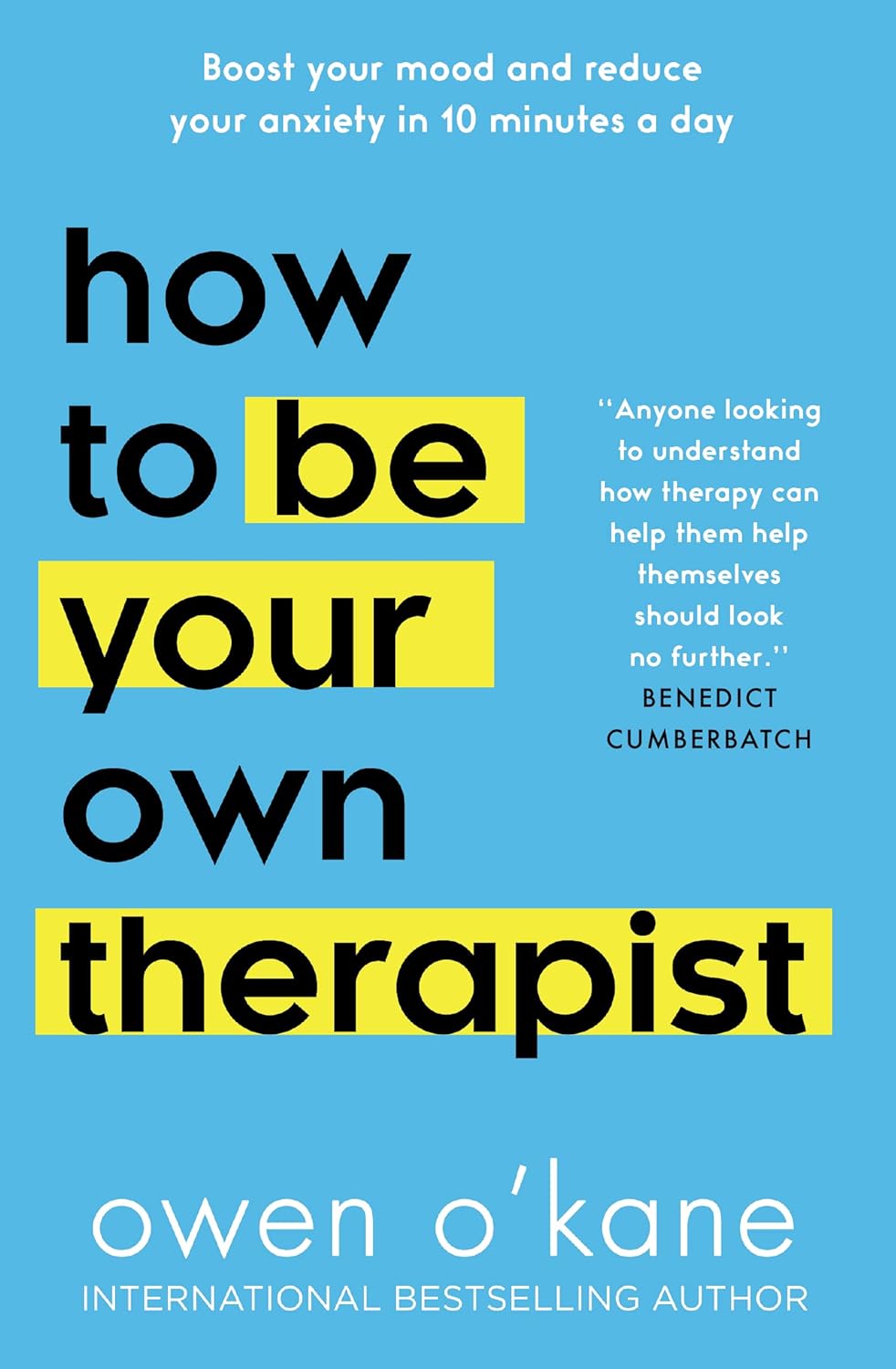
How to Be Your Own Therapist – by Owen O’Kane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Finding the right therapist can be hard. Sometimes, even just accessing a therapist, any therapist, can be hard, if circumstances are adverse. Sometimes we’d like therapy, but want to feel “better prepared for it” before we do.
Owen O’Kane, a highly qualified and well-respected psychotherapist, wants to put some tools in our hands. The premise of this book is that “in 10 minutes a day” one can give oneself an amount of therapy that will be beneficial.
Naturally, in 10 minutes a day, this isn’t going to be the kind of therapy that will work through major traumas, so what can it do?
Those 10 minutes are spread into three sessions:
- 4 minutes in the morning
- 3 minutes in the afternoon
- 3 minutes in the evening
The idea is:
- To do a quick mental health “check-in” before the day gets started, ascertain what one needs in that context, and make a simple plan to get/have it.
- To keep one’s mental health on track by taking a little pause to reassess and adjust if necessary
- To reflect on the day, amplify the positive, and let go of the negative to what extent is practical, in order to rest well ready for the next day
Where O’Kane excels is in explaining how to do those things in a way that is neither overly simplistic and wishy-washy, nor so arcane and convoluted as to create more work and render the day more difficult.
In short, this book is a great prelude to (or adjunct to) formal therapy, and for those for whom therapy isn’t accessible and/or desired, a great way to keep oneself on a mentally healthy track.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Going for a bushwalk? 3 handy foods to have in your backpack (including muesli bars)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This time of year, many of us love to get out and spend time in nature. This may include hiking through Australia’s many beautiful national parks.
Walking in nature is a wonderful activity, supporting both physical and mental health. But there can be risks and it’s important to be prepared.
You may have read the news about hiker, Hadi Nazari, who was recently found alive after spending 13 days lost in Kosciuszko National Park.
He reportedly survived for almost two weeks in the Snowy Mountains region of New South Wales by drinking fresh water from creeks, and eating foraged berries and two muesli bars.
So next time you’re heading out for a day of hiking, what foods should you pack?
Here are my three top foods to carry on a bushwalk that are dense in nutrients and energy, lightweight and available from the local grocery store.
Leah-Anne Thompson/Shutterstock 1. Muesli bars
Nazari reportedly ate two muesli bars he found in a mountain hut. Whoever left the muesli bars there made a great choice.
Muesli bars come individually wrapped, which helps them last longer and makes them easy to transport.
They are also a good source of energy. Muesli bars typically contain about 1,500–1,900 kilojoules per 100 grams. The average energy content for a 35g bar is about 614kJ.
This may be a fraction of what you’d usually need in a day. However, the energy from muesli bars is released at a slow to moderate pace, which will help keep you going for longer.
Muesli bars are also packed with nutrients. They contain all three macronutrients (carbohydrate, protein and fat) that our body needs to function. They’re a good source of carbohydrates, in particular, which are a key energy source. An average Australian muesli bar contains 14g of whole grains, which provide carbohydrates and dietary fibre for long-lasting energy.
Muesli bars that contain nuts are typically higher in fat (19.9g per 100g) and protein (9.4g per 100g) than those without.
Fat and protein are helpful for slowing down the release of energy from foods and the protein will help keep you feeling full for longer.
There are many different types of muesli bars to choose from. I recommend looking for those with whole grains, higher dietary fibre and higher protein content.
2. Nuts
Nuts are nature’s savoury snack and are also a great source of energy. Cashews, pistachios and peanuts contain about 2,300-2,400kJ per 100g while Brazil nuts, pecans and macadamias contain about 2,700-3,000kJ per 100g. So a 30g serving of nuts will provide about 700-900kJ depending on the type of nut.
Just like muesli bars, the energy from nuts is released slowly. So even a relatively small quantity will keep you powering on.
Nuts are also full of nutrients, such as protein, fat and fibre, which will help to stave off hunger and keep you moving for longer.
When choosing which nuts to pack, almost any type of nut is going to be great.
Peanuts are often the best value for money, or go for something like walnuts that are high in omega-3 fatty acids, or a nut mix.
Whichever nut you choose, go for the unsalted natural or roasted varieties. Salted nuts will make you thirsty.
Nut bars are also a great option and have the added benefit of coming in pre-packed serves (although nuts can also be easily packed into re-usable containers).
If you’re allergic to nuts, roasted chickpeas are another option. Just try to avoid those with added salt.
Nuts are nature’s savoury snack and are also a great source of energy. Eakrat/Shutterstock 3. Dried fruit
If nuts are nature’s savoury snack, fruit is nature’s candy. Fresh fruits (such as grapes, frozen in advance) are wonderfully refreshing and perfect as an everyday snack, although can add a bit of weight to your hiking pack.
So if you’re looking to reduce the weight you’re carrying, go for dried fruit. It’s lighter and will withstand various conditions better than fresh fruit, so is less likely to spoil or bruise on the journey.
There are lots of varieties of dried fruits, such as sultanas, dried mango, dried apricots and dried apple slices.
These are good sources of sugar for energy, fibre for fullness and healthy digestion, and contain lots of vitamins and minerals. So choose one (or a combination) that works for you.
Don’t forget water
Next time you head out hiking for the day, you’re all set with these easily available, lightweight, energy- and nutrient-dense snacks.
This is not the time to be overly concerned about limiting your sugar or fat intake. Hiking, particularly in rough terrain, places demands on your body and energy needs. For instance, an adult hiking in rough terrain can burn upwards of about 2,000kJ per hour.
And of course, don’t forget to take plenty of water.
Having access to even limited food, and plenty of fresh water, will not only make your hike more pleasurable, it can save your life.
Margaret Murray, Senior Lecturer, Nutrition, Swinburne University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Paving The Way To Good Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Dr. Michelle Tollefson. She’s a gynecologist, and a menopause and lifestyle medicine expert. She’s also a breast cancer survivor, and, indeed, thriver.
So, what does she want us to know?
A Multivector Approach To Health
There’s a joke that goes: a man is trapped in a flooding area, and as the floodwaters rise, he gets worried and begins to pray, but he is interrupted when some people come by on a raft and offer him to go with them. He looks at the rickety raft and says “No, you go on, God will spare me”. He returns to his prayer, and is further interrupted by a boat and finally a helicopter, and each time he gives the same response. He drowns, and in the afterlife he asks God “why didn’t you spare me from the flood?”, and God replies “I sent a raft, a boat, and a helicopter; what more did you want?!”
People can be a bit the same when it comes to different approaches to cancer and other serious illness. They are offered chemotherapy and say “No, thank you, eating fruit will spare me”.
Now, this is not to trivialize those who decline aggressive cancer treatments for other reasons such as “I am old and would rather not go through that; I’d rather have a shorter life without chemo than a longer life with it”—for many people that’s a valid choice.
But it is to say: lifestyle medicine is, mostly, complementary medicine.
It can be very powerful! It can make the difference between life and death! Especially when it comes to things like cancer, diabetes, heart disease, etc.
But it’s not a reason to decline powerful medical treatments if/when those are appropriate. For example, in Dr. Tollefson’s case…
Synergistic health
Dr. Tollefson, herself a lifestyle medicine practitioner and gynecologist (and having thus done thousands of clinical breast exams for other people, screening for breast cancer), says she owes her breast cancer survival to two things, or rather two categories of things:
- a whole-food, plant predominant diet, daily physical activity, prioritizing sleep, minimizing stress, and a strong social network
- a bilateral mastectomy, 16 rounds of chemotherapy, removal of her ovaries, and several reconstructive surgeries
Now, one may wonder: if the first thing is so good, why need the second?
Or on the flipside: if the second thing was necessary, what was the point of the first?
And the answer she gives is: the first thing was the reason she was able to make it through the second thing.
And on the next level: the second thing was the reason she’s still around to talk about the first thing.
In other words: she couldn’t have done it with just one or the other.
A lot of medicine in general, and lifestyle medicine in particular, is like this. If we note that such-and-such a thing decreases our risk of cancer mortality by 4%, that’s a small decrease, but it can add up (and compound!) if it’s surrounded by other things that also each decrease the risk by 12%, 8%, 15%, and so on.
Nor is this only confined to cancer, nor only to the positives.
Let’s take cardiovascular disease: if a person smokes, drinks, eats red meat, stresses, and has a wild sleep schedule, you can imagine those risk factors add up and compound.
If this person and another with a heart-healthy lifestyle both have a stroke (it can happen to anyone, even if it’s less likely in this case), and both need treatment, then two things are true:
- They are both still going to need treatment (medicines, and possibly a thrombectomy)
- The second person is most likely to recover, and most likely to recover more quickly and easily
The second person can be said to have paved the way to their recovery, with their lifestyle.
Which is really important, because a lot of people think “what’s the point in living so healthily if [disease] strikes anyway?” and the answer is:
A very large portion of your recovery is predicated on how you lived your life before The Bad Thing™ happened, and that can be the difference between bouncing back quickly and a long struggle back to health.
Or the difference between a long struggle back to health, or a short struggle followed by rapid decline and death.
In short:
Play the odds, improve your chances with lifestyle medicine. Enjoy those cancer-fighting fruits:
Top 8 Fruits That Prevent & Kill Cancer
…but also, get your various bits checked when appropriate; we know, mammograms and prostate checks etc are not usually the highlight of most people’s days, but they save lives. And if it turns out you need serious medical interventions, consider them seriously.
And, by all means, enjoy mood-boosting nutraceuticals such as:
12 Foods That Fight Depression & Anxiety
…but also recognize that sometimes, your brain might have an ongoing biochemical problem that a tablespoon of pumpkin seeds isn’t going to fix.
And absolutely, you can make lifestyle adjustments to reduce the risks associated with menopause, for example:
Menopause, & How Lifestyle Continues To Matter “Postmenopause”
…but also be aware that if the problem is “not enough estrogen”, sometimes to solution is “take estrogen”.
And so on.
Want to know Dr. Tollefson’s lifestyle recommendations?
Most of them will not be a surprise to you, and we mentioned some of them above (a whole-food, plant predominant diet, daily physical activity, prioritizing sleep, minimizing stress, and a strong social network), but for more specific recommendations, including numbers etc, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: