Tips for Improving Memory
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Q&A with 10almonds Subscribers!
Q: Any tips, other than supplements, for improving memory?
A: So many tips! Certainly enough to do a main feature on, so again maybe we’ll do that in another issue soon. Meanwhile, here are the absolute most critical things for you to know, understand, and apply:
- Memory is a muscle. Not literally, but in the sense that it will grow stronger if exercised and will atrophy if neglected.
- Counterpart of the above: your memory is not a finite vessel. You can’t “fill it up with useless things”, so no need to fear doing so.
- Your memory is the product of countless connections in your brain. The more connections lead to a given memory, the more memorable it will be. What use is this knowledge to you? It means that if you want to remember something, try to make as many connections to it as possible, so:
- Involve as many senses as possible.
- When you learn things, try to learn them in context. Then when your mind has reason to think about the context, it’ll be more likely to remember the thing itself too.
- Rehearsal matters. A lot. This means repeatedly going over something in your head. This brings about the neural equivalent of “muscle memory”.
- Enjoy yourself if you can. The more fun something is, the more you will mentally rehearse it, and the more mental connections you’ll make to it.
Have a question you’d like to see answered here? Hit reply to this email, or use the feedback widget at the bottom! We always love to hear from you
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What To Leave Off Your Table (To Stay Off This Surgeon’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Why we eat too much (and how we can fix that)
This is Dr. Andrew Jenkinson. He’s a Consultant Surgeon specializing in the treatment of obesity, gallstones, hernias, heartburn and abdominal pain. He runs regular clinics in both London and Dubai. What he has to offer us today, though, is insight as to what’s on our table that puts us on his table, and how we can quite easily change that up.
So, why do we eat too much?
First things first: some metabolic calculations. No, we’re not going to require you to grab a calculator here… Your body does it for you!
Our body’s amazing homeostatic system (the system that does its best to keep us in the “Goldilocks Zone” of all our bodily systems; not too hot or too cold, not dehydrated or overhydrated, not hyperglycemic or hypoglycemic, blood pressure not too high or too low, etc, etc) keeps track of our metabolic input and output.
What this means: if we increase or decrease our caloric consumption, our body will do its best to increase or decrease our metabolism accordingly:
- If we don’t give it enough energy, it will try to conserve energy (first by slowing our activities; eventually by shutting down organs in a last-ditch attempt to save the rest of us)
- If we give it too much energy, it will try to burn it off, and what it can’t burn, it will store
In short: if we eat 10% or 20% more or less than usual, our body will try to use 10% to 20% more or less than usual, accordingly.
So… How does this get out of balance?
The problem is in how our system does that, and how we inadvertently trick it, to our detriment.
For a system to function, it needs at its most base level two things—a sensor and a switch:
- A sensor: to know what’s going on
- A switch: to change what it’s doing accordingly
Now, if we eat the way we’re evolved to—as hunter-gatherers, eating mostly fruit and vegetables, supplemented by animal products when we can get them—then our body knows exactly what it’s eating, and how to respond accordingly.
Furthermore, that kind of food takes some eating! Most fruit these days is mostly water and fiber; in those days it often had denser fiber (before agricultural science made things easier to eat), but either way, our body knows when we are eating fruit and how to handle that. Vegetables, similarly. Unprocessed animal products, again, the gut goes “we know what this is” and responds accordingly.
But modern ultra-processed foods with trans-fatty acids, processed sugar and flour?
These foods zip calories straight into our bloodstream like greased lightning. We get them so quickly so easily and in such great caloric density, that our body doesn’t have the chance to count them on the way in!
What this means is: the body has no idea what it’s just consumed or how much or what to do with it, and doesn’t adjust our metabolism accordingly.
Bottom line:
Evolutionarily speaking, your body has no idea what ultra-processed food is. If you skip it and go for whole foods, you can, within the bounds of reason, eat what you like and your body will handle it by adjusting your metabolism accordingly.
Now, advising you “avoid ultra-processed foods and eat whole foods” was probably not a revelation in and of itself.
But: sometimes knowing a little more about the “why” makes the difference when it comes to motivation.
Want to know more about Dr. Jenkinson’s expert insights on this topic?
If you like, you can check out his website here—he has a book too
Why We Eat (Too Much) – Dr. Andrew Jenkinson on the Science of Appetite
Share This Post
-
How To Eat To Lose Belly Fat (3 Stages)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Belly fat is easier to gain than it is to lose, and it’s absolutely something that needs more attention in the kitchen than in the gym. Here’s one way of doing it:
By the numbers
First note: this video is by a man, and judging by the numbers mentioned, assumes that the viewer is also a man. An end goal of 10% body fat is a little on the low side for men, and would be dangerous for women. The magic 15% mark that he mentions as being a point where various metabolic things change, is more like 20% for women. All assuming normal hormones, of course, since it is hormones that direct this.
Healthy body fat percentages are (assuming normal hormones) in the range of 20–25% for women and 15–20% for men.
With that in mind…
The idea of this approach is to lose enough weight that your body gets rid of even the most awkward bits (e.g: visceral belly fat, which will often be the last to get used) before, if desired, then maintaining at a slightly higher body fat percentage.
- Stage 1: count calories (we don’t usually recommend this at 10almonds, but he does, so we’re reporting it here) and use your weight in pounds multiplied by 12 to give your daily calorie target. Make the majority of your diet foods that have a large volume:calorie ratio, such as fruits and vegetables, in order to feel full without overloading your metabolism. He has an interesting method of calculating a protein target; instead of the usual “1g/kg of body weight”, he says 1g per cm of height. Doing this consistently should get you to 15% body fat (so, 20%, for women).
- Stage 2: start counting fat intake too, and aim for 20–25% of your daily calories as fat. Continue, aside from that, with what you were doing in Stage 1. Doing this consistently should get you to 12% body fat (so, about 17%, for women). Being under the usual healthy level for a while should allow your body to start getting rid of visceral fat.
- Stage 3: track everything, levelling up your precision (no more “this little thing doesn’t count”), and planning ahead when it comes to social events etc. Doing this consistently should yet you to 10% body fat (so, about 15%, for women). This stage has a good chance of making most people miserable, so if that happens, consider the benefits of going back to the healthier 15% body fat (men) or 20% (women).
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Visceral Belly Fat & How To Lose It ← without calorie-counting! We prefer this 😉
Take care!
Share This Post
-
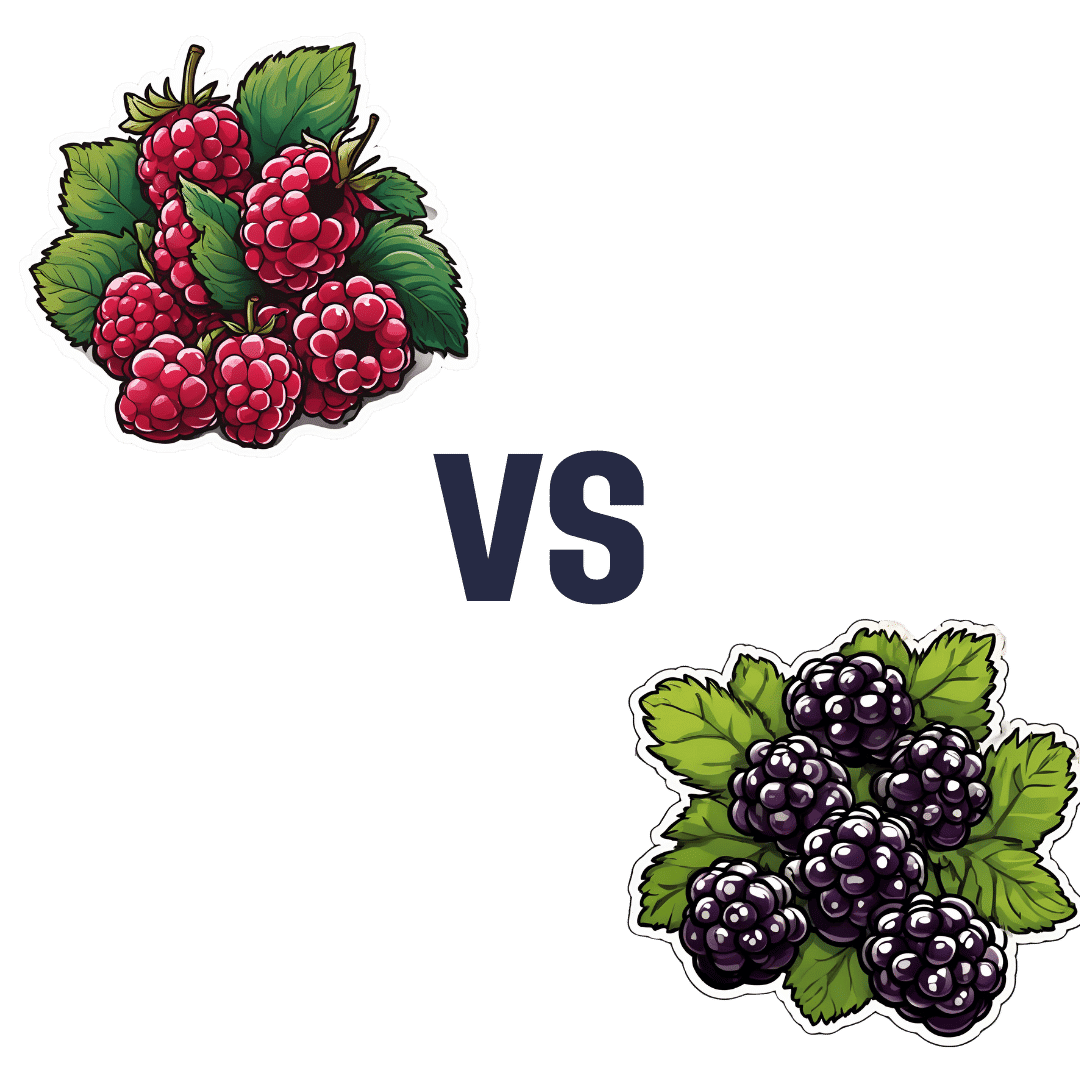
Raspberries vs Blackberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing raspberries to blackberries, we picked the blackberries.
Why?
It was very close! Raspberries most certainly also have their merits. But blackberries do just a little bit better in a few categories:
In terms of macros, raspberries have a tiny bit more carbs and fiber, while blackberries have a even tinier bit more protein, and the two berries have an equal glycemic index. We’ll call this category a tie, or else the meanest of nominal wins for raspberry.
In the category of vitamins, raspberries have more of vitamins B1, B2, B5, B6, and choline, while blackberries have more of vitamins A, B3, B9, C, E, and K. This would be a very marginal win for blackberries, except that blackberries have more than 6x the vitamin A, a much larger margin than any of the other differences in vitamins (which were usually small differences), which gives blackberry a more convincing win here.
When it comes to minerals, things are closer: raspberries have more iron, magnesium, manganese, and phosphorus, while blackberries have more calcium, copper, potassium, selenium, and zinc. None of the differences are outstanding, so this is a simple marginal victory for blackberries.
It would be rude to look at berries without noting their polyphenols; we’re not list them all (or this article will get very long, because each has very many polyphenols with names like “pelargonidin 3-O-glucosyl-rutinoside” and so forth), but suffice it to say: raspberries are great for polyphenols and blackberries are even better for polyphenols.
That said… In the category of specific polyphenols we’ve written about before at 10almonds, it’s worth noting a high point of each berry, for the sake of fairness: raspberries have more quercetin (but blackberries have lots too) and blackberries have more ellagic acid (of which, raspberries have some, but not nearly as much). Anyway, just going off total polyphenol content, blackberries are the clear winner here.
Adding up the sections makes for an overall win for blackberries, but by all means, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
21 Most Beneficial Polyphenols & What Foods Have Them
Enjoy!
Share This Post
Related Posts
-
Brain Power – by Michael Gelb & Kelly Howell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s most important when it comes to brain health? Is it the right diet? Supplements? Brain-training? Attitude? Sleep? Physical exercise? Social connections? Something else?
This book covers a lot of bases, including all of the above and more. The authors are not scientists by training and this is not a book of science, so much as a book of aggregated science-based advice from other sources. The authors did consult with many scientists, and their input is shown throughout.
In the category of criticism, nothing here goes very deeply into the science, and there’s also nothing you wouldn’t find we’ve previously written about in a 10almonds article somewhere. But all the same, it’s good to have a wide variety of brain-healthy advices all in one place.
Bottom line: if you’re looking for a one-stop-shop “look after your brain as you age” guide, then this is a good one.
Click here to check out Brain Power, and improve your mind as you age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tell Yourself a Better Lie – by Marissa Peer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As humans, we generally lie to ourselves constantly. Or perhaps we really believe some of the things we tell ourselves, even if they’re not objectively necessarily true:
- I’ll always be poor
- I’m destined to be alone
- I don’t deserve good things
- Etc.
Superficially, it’s easy to flip those, and choose to tell oneself the opposite. But it feels hollow and fake, doesn’t it? That’s where Marissa Peer comes in.
Our stories that we tell ourselves don’t start where we are—they’re generally informed by things we learned along the way. Sometimes good lessons, sometimes bad ones. Sometimes things that were absolutely wrong and/or counterproductive.
Peer invites the reader to ask “What if…”, unravel how the unhelpful lessons got wired into our brains in the first place, and then set about untangling them.
“Tell yourself a better lie” does not mean self-deceit. It means that we’re the authors of our own stories, so we might as well make them work for us. Many things in life are genuinely fixed; others are open to interpretation.
Sorting one from the other, and then treating them correctly in a way that’s helpful to us? That’s how we can stop hurting ourselves, and instead bring our own stories around to uplift and fortify us.
Get Your Copy of “Tell Yourself A Better Lie” on Amazon Today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mediterranean Air Fryer Cookbook – by Naomi Lane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are Mediterranean Diet cookbooks, and there are air fryer cookbooks. And then there are (a surprisingly large intersection of!) Mediterranean Diet air fryer cookbooks. We wanted to feature one of them in today’s newsletter… And as part of the selection process, looked through quite a stack of them, and honestly, were quite disappointed with many. This one, however, was one of the ones that stood out for its quality of both content and clarity, and after a more thorough reading, we now present it to you:
Naomi Lane is a professional dietician, chef, recipe developer, and food writer… And it shows, on all counts.
She covers what the Mediterranean diet is, and she covers far more than this reviewer knew it was even possible to know about the use of an air fryer. That alone would make the book a worthy purchase already.
The bulk of the book is the promised 200 recipes. They cover assorted dietary requirements (gluten-free, dairy-free, etc) while keeping to the Mediterranean Diet.
The recipes are super clear, just what you need to know, no reading through a nostalgic storytime first to find things. Also no pictures, which will be a plus for some readers and a minus for others. The recipes also come complete with nutritional information for each meal (including sodium), so you don’t have to do your own calculations!
Bottom line: this is the Mediterranean Diet air fryer cook book. Get it, thank us later!
Get your copy of “Mediterranean Air Fryer Cookbook” on Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: