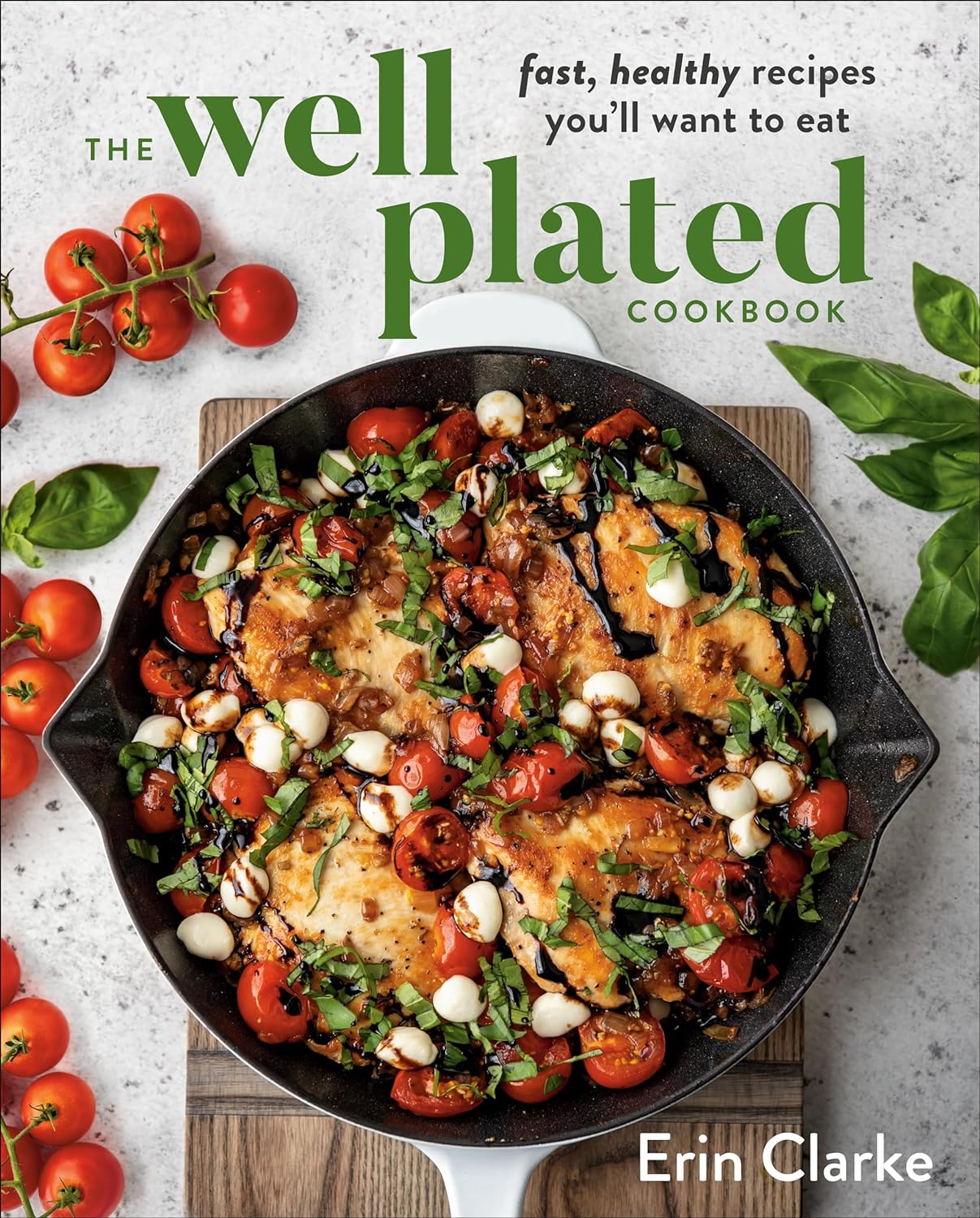
The Well Plated Cookbook – by Erin Clarke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Clarke’s focus here is on what she calls “stealthy healthy”, with the idea of dishes that feel indulgent while being great for the health.
The recipes, of which there are well over 100, are indeed delicious and easy to make without being oversimplified, and since she encourages the use of in-season ingredients, many recipes come with a “market swaps” substitution guide, to make each recipe seasonal.
The book is largely not vegetarian, let alone vegan, but the required substitutions will be second-nature to any seasoned vegetarian or vegan. Indeed, “skip the meat sometimes” is one of the advices she offers near the beginning of the book, in the category of tips to make things even healthier.
Bottom line: if you want to add dishes to your repertoire that are great for entertaining and still super-healthy, this book will be a fine addition to your collection.
Click here to check out The Well Plated Cookbook, and get cooking!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Cancer Journey – by Dr. Chadi Nabhan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After a brief introduction of what cancer actually is and what causes it, the layout of the rest of the book is in chronological order of patient experience, that is to say, what to expect during the journey from screening and diagnosis, to one’s first oncology visit (the author being an oncologist himself), how cancer staging works, getting second opinions, and a chapter-by-chapter review of many different treatment options, ranging from surgery and chemotherapy, to radiation and hormonal therapies, and even more modern targeted therapies, immunotherapy, cellular therapies, and yes, complementary and alternative therapies, amongst others we haven’t listed for the sake of brevity.
He doesn’t leave it there though; he also talks managing side effects, monitoring for recurrence, and even caring for the caregiver(s), along with eventual survivorship and that emotional journey, or if it comes down to it, palliative and hospice care.
Finishing on a hopeful note, he also brings attention to novel approaches that are being trialled presently, and the prospects for the near future of cancer care.
The style is very human and readable, notwithstanding that the author has hundreds of peer-reviewed publications to his name, the content here is presented in a much more approachable, less clinical way, while still conveying all the information that needs to be conveyed.
Bottom line: if you or a loved one is facing cancer, this book will be an invaluable resource.
Click here to check out The Cancer Journey, and understand each part of it!
Share This Post
-
Planning Festivities Your Body Won’t Regret
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Festive Dilemma
For many, Christmas is approaching. Other holidays abound too, and even for the non-observant, it’d be hard to escape seasonal jollities entirely.
So, what’s the plan?
- Eat, drink, and be merry, and have New Year’s Resolutions for the first few days of January before collapsing in a heap?
- Approach the Yuletide with Spartan abstemiousness and miss all the fun while simultaneously annoying your relatives?
Let’s try to find a third approach instead…
What’s festive and healthy?
We’re doing this article this week, because many people will be shopping already, making plans, and so forth. So here are some things to bear in mind:
Make your own mindful choices
Coca-Cola company really did a number on Christmas, but it doesn’t mean their product is truly integral to the season. Same goes for many other things that flood the stores around this time of year. So much sugary confectionary! But remember, they’re not the boss of you. If you wouldn’t buy it ordinarily, why are you buying it now? Do you actually even want it?
If you really do, then you do you, but mindful choices will invariably be healthier than “because there were three additional aisles of confectionary now so I stopped and looked and picked some things”.
Pick your battles
If you’re having a big family gathering, likely there will be occasions with few healthy options available. But you can decide what’s most important for you to avoid, perhaps picking a theme, e.g:
- No alcohol this year, or
- No processed sugary foods, or
- Eat/drink whatever, but practice intermittent fasting
Some resources:
Fight inflammation
This is a big one so it deserves its own category. In the season of sugar and alcohol and fatty meat, inflammation can be a big problem to come around and bite us in the behind. We’ve written on this previously:
Positive dieting
In other words, less of a focus on what to exclude, and more of a focus on what to include in your diet. Fruity drinks and sweets are common at this time of year, but you know what’s also fruity? Fruit!
And it can be festive, too! Berries are great, and those tiny orange-like fruits that may be called clementines or tangerines or satsumas or, as Aldi would have it, “easy peelers”. Apple and cinnamon are also a great combination that both bring sweetness without needing added sugar.
And as for mains? Make your salads that bit fancier, get plenty of greens with your main, have hearty soups and strews with lentils and beams!
See also: Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
Your gut will thank us later!
Get moving!
That doesn’t mean you have to beat the New Year rush to the gym (unless you want to!). But it could mean, for example, more time in your walking shoes (or dancing shoes! With a nod to today’s sponsor) and less time in the armchair.
See also: The doctor who wants us to exercise less; move more
Lastly…
Remember it’s supposed to be fun! And being healthy can be a lot more fun than suffering because of unfortunate choices that we come to regret.
Take care!
Share This Post
-
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Any idea about the latest research on the most effective exercises for osteoporosis?❞
While there isn’t much new of late in this regard, there is plenty of research!
First, what you might want to avoid:
- Sit-ups, and other exercises with a lot of repeated spinal flexion
- Running, and other high-impact exercises
- Skiing, horse-riding, and other activities with a high risk of falling
- Golf and tennis (both disproportionately likely to result in injuries to wrists, elbows, and knees)
Next, what you might want to bear in mind:
While in principle resistance training is good for building strong bones, good form becomes all the more important if you have osteoporosis, so consider working with a trainer if you’re not 100% certain you know what you’re doing:
Some of the best exercises for osteoporosis are isometric exercises:
5 Isometric Exercises for Osteoporosis (with textual explanations and illustrative GIFs)
You might also like this bone-strengthening exercise routine from corrective exercise specialist Kendra Fitzgerald:
Enjoy!
Share This Post
Related Posts
-
The Mediterranean Diet: What Is It Good For?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More to the point: what isn’t it good for?
- It’s been found to reduce all-cause mortality, which is about the best thing one can say of any diet.
- It’s especially good for heart health and against cancer.
- It’s particularly recommended for the prevention or management of diabetes.
- It’s also been found, societally, to reduce general healthcare costs—basically, people get sick less and so have fewer healthcare costs.
What brought it to the attention of the world’s scientific community?
Back in the 1950s, physiologist Ancel Keys wondered why poor people in Italian villages were healthier than wealthy New Yorkers. Upon undertaking studies, he narrowed it down to the Mediterranean diet—something he’d then take on as a public health cause for the rest of his career.
Keys himself lived to the ripe old age of 100, by the way.
When we say “Mediterranean Diet”, what image comes to mind?
We’re willing to bet that tomatoes feature (great source of lycopene, by the way), but what else?
- Salads, perhaps? Vegetables, olives? Olive oil, yea or nay?
- Bread? Pasta? Prosciutto, salami? Cheese?
- Pizza but only if it’s Romana style, not Chicago?
- Pan-seared liver, with some fava beans and a nice Chianti?
In reality, the diet is based on what was historically eaten specifically by Italian peasants. If the word “peasants” conjures an image of medieval paupers in smocks and cowls, and that’s not necessarily wrong, further back historically… but the relevant part here is that they were people who lived and worked in the countryside.
They didn’t have money for meat, which was expensive, nor the industrial setting for refined grain products to be affordable. They didn’t have big monocrops either, which meant no canola oil, for example… Olives produce much more easily extractable oil per plant, so olive oil was easier to get. Nor, of course, did they have the money (or infrastructure) for much in the way of imports.
So what foods are part of “the” Mediterranean Diet?
- Fruits. These would be fruits grown locally, but no need to sweat that, dietwise. It’s hard to go wrong with fruit.
- Tomatoes yes. So many tomatoes. (Knowledge is knowing tomato is a fruit. Wisdom is not putting it in a fruit salad)
- Non-starchy vegetables (e.g. eggplant yes, potatoes no)
- Greens (spinach, kale, lettuce, all those sorts of things)
- Beans and other legumes (whatever was grown nearby)
- Whole grain products in moderation (wholegrain bread, wholewheat pasta)
- Olives and olive oil. Special category, single largest source of fat in the Mediterranean diet, but don’t overdo it.
- Dairy products in moderation (usually hard cheeses, as these keep well)
- Fish, in moderation. Typically grilled, baked, steamed even. Not fried.
- Other meats as a rarer luxury in considerable moderation. There’s more than one reason prosciutto is so thinly sliced!
Want to super-power this already super diet?
Try: A Pesco-Mediterranean Diet With Intermittent Fasting: JACC Review Topic of the Week
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Type 2 Diabetic Foot Problems
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: I’d like to know more about type 2 diabetic foot problems
You probably know that the “foot problems” thing has less to do with the feet and more to do with blood and nerves. So, why the feet?
The reason feet often get something like the worst of it, is because they are extremities, and in the case of blood sugars being too high for too long too often, they’re getting more damage as blood has to fight its way back up your body. Diabetic neuropathy happens when nerves are malnourished because the blood that should be keeping them healthy, is instead syrupy and sluggish.
We’ll definitely do a main feature sometime soon on keeping blood sugars healthy, for both types of diabetes plus pre-diabetes and just general advice for all.
In the meantime, here’s some very good advice on keeping your feet healthy in the context of diabetes. This one’s focussed on Type 1 Diabetes, but the advice goes for both:
! Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
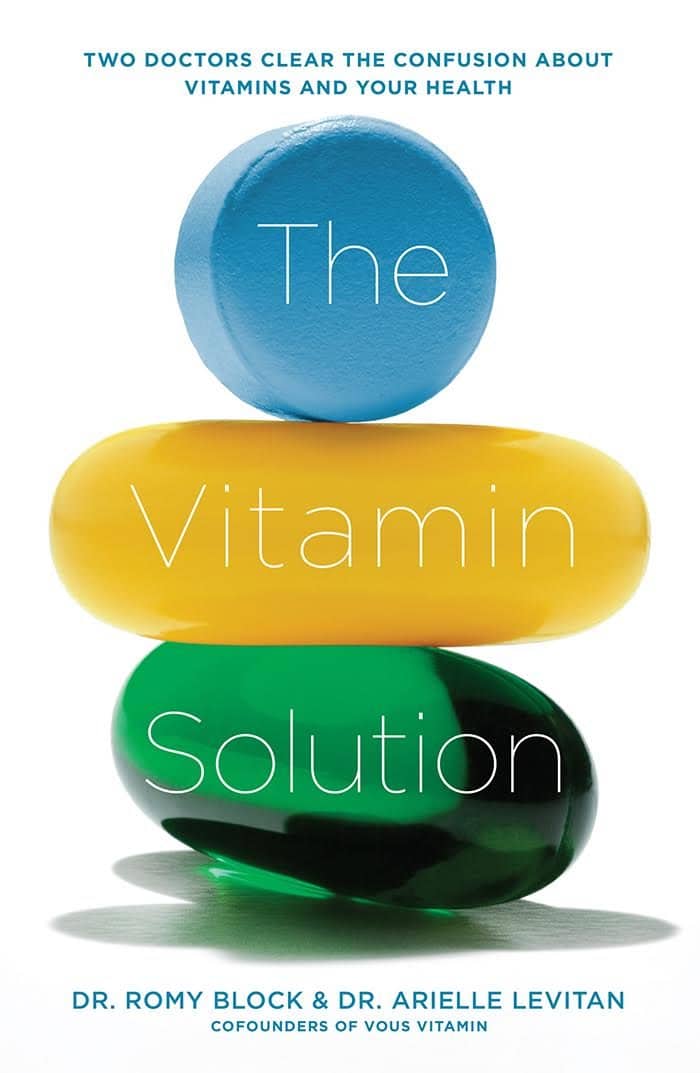
The Vitamin Solution – by Dr. Romy Block & Dr. Arielle Levitan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note: it would be remiss of us not to mention that the authors of this book are also the founders of a vitamin company, thus presenting a potential conflict of interest.
That said… In this reviewer’s opinion, the book does seem balanced and objective, regardless.
We talk a lot about supplements here at 10almonds, especially in our Monday Research Review editions. And yesterday, we featured a book by a doctor who hates supplements. Today, we feature a book by two doctors who have made them their business.
The authors cover all the most common vitamins and minerals popularly enjoyed as supplements, and examine:
- why people take them
- factors affecting whether they help
- problems that can arise
- complicating factors
The “complicating factors” include, for example, the way many vitamins and/or minerals interplay with each other, either by requiring the presence of another, or else competing for resources for absorption, or needing to be delicately balanced on pain of diverse woes.
This is the greatest value of the book, perhaps; it’s where most people go wrong with supplementation, if they go wrong.
While both authors are medical doctors, Dr. Romy Block is an endocrinologist specifically, and she clearly brought a lot of extra attention to relevant metabolic/thyroid issues, and how vitamins and minerals (such as thiamin and iron) can improve or sabotage such, depending on various factors that she explains. Informative, and so far as this reviewer could see, objective and well-balanced.
Bottom line: supplementation is a vast and complex topic, but this book does a fine job of demystifying and simplifying it in a clear and objective fashion, without resorting to either scaremongering or hype.
Click here to check out The Vitamin Solution, and upgrade your knowledge!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: