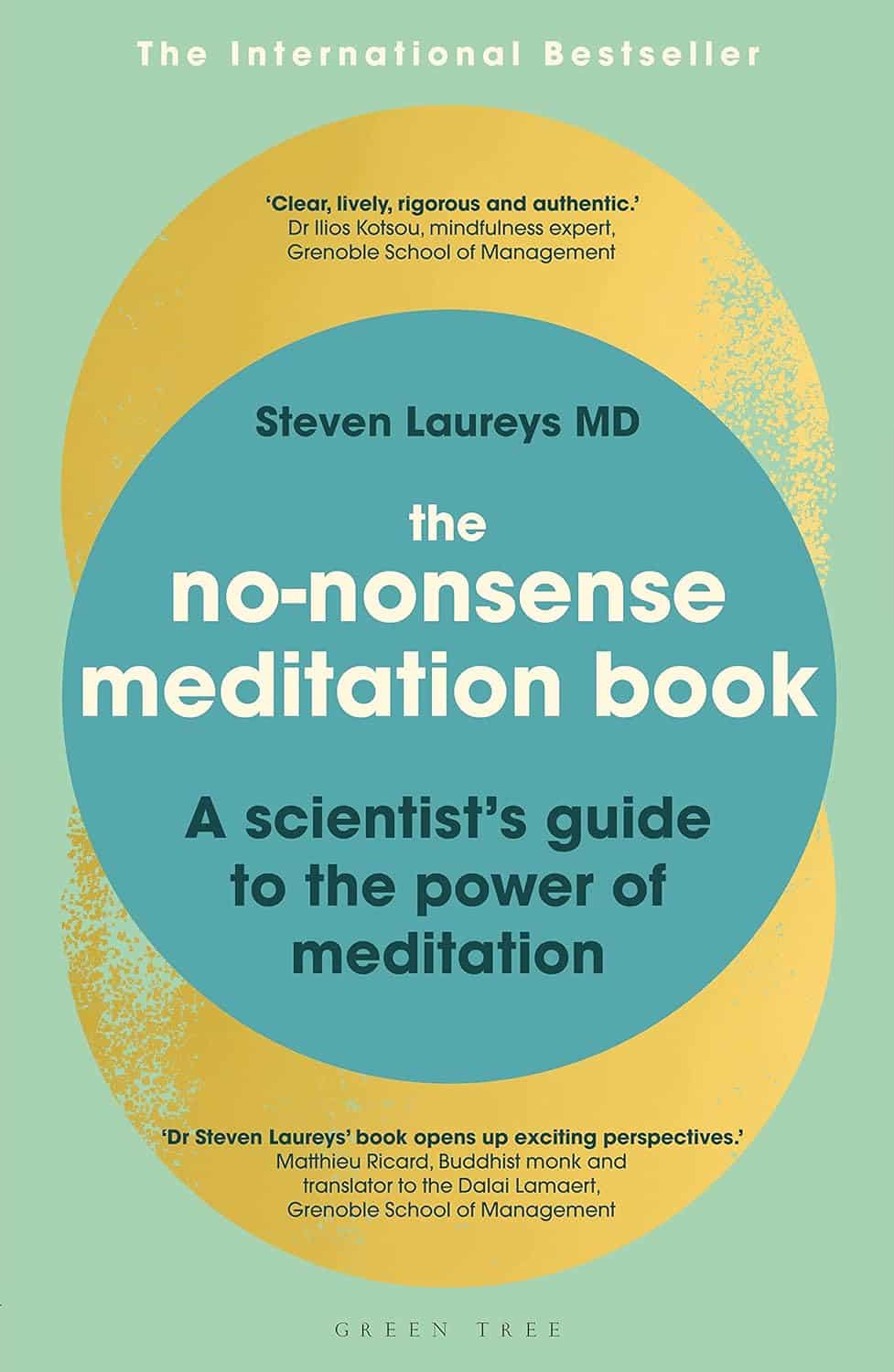
The No-Nonsense Meditation Book – by Dr. Steven Laureys
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about meditation before, and when we review books, we try to pick ones that have something that make them stand out from the others. So, what stands out in this case?
The author is a medical doctor and neurologist, with decades of experience focusing on neuronal plasticity and multimodel neural imaging. So, a little beyond “think happy thoughts”-style woo.
The style of the book is pop-science in tone, but with a lot of hard clinical science underpinning it and referenced throughout, as one would expect of a scientist of Dr. Laurey’s stature (with hundreds of peer-reviewed papers in top-level journals).
You may be wondering: is this a “how-to” book or a “why-to” book or a “what-happens” book? It’s all three.
The “how-to” is also, as the title suggests, no-nonsense. We are talking maximum results for minimum mystery here.
Bottom line: if you’d like to be able to take up a meditative practice and know exactly what it’s doing to your brain (quietening these parts, stimulating and physically growing those parts, etc) then this is the book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Running or yoga can help beat depression, research shows – even if exercise is the last thing you feel like
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At least one in ten people have depression at some point in their lives, with some estimates closer to one in four. It’s one of the worst things for someone’s wellbeing – worse than debt, divorce or diabetes.
One in seven Australians take antidepressants. Psychologists are in high demand. Still, only half of people with depression in high-income countries get treatment.
Our new research shows that exercise should be considered alongside therapy and antidepressants. It can be just as impactful in treating depression as therapy, but it matters what type of exercise you do and how you do it.
Walk, run, lift, or dance away depression
We found 218 randomised trials on exercise for depression, with 14,170 participants. We analysed them using a method called a network meta-analysis. This allowed us to see how different types of exercise compared, instead of lumping all types together.
We found walking, running, strength training, yoga and mixed aerobic exercise were about as effective as cognitive behaviour therapy – one of the gold-standard treatments for depression. The effects of dancing were also powerful. However, this came from analysing just five studies, mostly involving young women. Other exercise types had more evidence to back them.
Walking, running, strength training, yoga and mixed aerobic exercise seemed more effective than antidepressant medication alone, and were about as effective as exercise alongside antidepressants.
But of these exercises, people were most likely to stick with strength training and yoga.
Antidepressants certainly help some people. And of course, anyone getting treatment for depression should talk to their doctor before changing what they are doing.
Still, our evidence shows that if you have depression, you should get a psychologist and an exercise plan, whether or not you’re taking antidepressants.
Join a program and go hard (with support)
Before we analysed the data, we thought people with depression might need to “ease into it” with generic advice, such as “some physical activity is better than doing none.”
But we found it was far better to have a clear program that aimed to push you, at least a little. Programs with clear structure worked better, compared with those that gave people lots of freedom. Exercising by yourself might also make it hard to set the bar at the right level, given low self-esteem is a symptom of depression.
We also found it didn’t matter how much people exercised, in terms of sessions or minutes a week. It also didn’t really matter how long the exercise program lasted. What mattered was the intensity of the exercise: the higher the intensity, the better the results.
Yes, it’s hard to keep motivated
We should exercise caution in interpreting the findings. Unlike drug trials, participants in exercise trials know which “treatment” they’ve been randomised to receive, so this may skew the results.
Many people with depression have physical, psychological or social barriers to participating in formal exercise programs. And getting support to exercise isn’t free.
We also still don’t know the best way to stay motivated to exercise, which can be even harder if you have depression.
Our study tried to find out whether things like setting exercise goals helped, but we couldn’t get a clear result.
Other reviews found it’s important to have a clear action plan (for example, putting exercise in your calendar) and to track your progress (for example, using an app or smartwatch). But predicting which of these interventions work is notoriously difficult.
A 2021 mega-study of more than 60,000 gym-goers found experts struggled to predict which strategies might get people into the gym more often. Even making workouts fun didn’t seem to motivate people. However, listening to audiobooks while exercising helped a lot, which no experts predicted.
Still, we can be confident that people benefit from personalised support and accountability. The support helps overcome the hurdles they’re sure to hit. The accountability keeps people going even when their brains are telling them to avoid it.
So, when starting out, it seems wise to avoid going it alone. Instead:
- join a fitness group or yoga studio
get a trainer or an exercise physiologist
- ask a friend or family member to go for a walk with you.
Taking a few steps towards getting that support makes it more likely you’ll keep exercising.
Let’s make this official
Some countries see exercise as a backup plan for treating depression. For example, the American Psychological Association only conditionally recommends exercise as a “complementary and alternative treatment” when “psychotherapy or pharmacotherapy is either ineffective or unacceptable”.
Based on our research, this recommendation is withholding a potent treatment from many people who need it.
In contrast, The Royal Australian and New Zealand College of Psychiatrists recommends vigorous aerobic activity at least two to three times a week for all people with depression.
Given how common depression is, and the number failing to receive care, other countries should follow suit and recommend exercise alongside front-line treatments for depression.
I would like to acknowledge my colleagues Taren Sanders, Chris Lonsdale and the rest of the coauthors of the paper on which this article is based.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.

Michael Noetel, Senior Lecturer in Psychology, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post

Reduce Your Skin Tag Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝As I get older, I seem to be increasingly prone to skin tags, which appear, seemingly out of nowhere, on my face, chest and back. My dermatologist happily burns them off – but is there anything I can do to prevent them?!❞
Not a lot! But, potentially something.
The main risk factor for skin tags is genetic, and you can’t change that in any easy way.
The other main risk factors are connected to each other:
Skin folds, and chafing
Skin tags mostly appear where chafing happens. This can be, for example:
- Inside joint articulations (especially groin and armpits)
- Between fat rolls (if you have them)
So, if you have fat rolls, then losing weight will also reduce the risk of skin tags.
Additionally, obesity and some often-related problems such as diabetes, hypertension, and an atherogenic lipid profile also increase the risk of skin tags (amongst other more serious things):
See: Association of Skin Tag with Metabolic Syndrome and its Components
As for the chafing, this can be reduced in various ways, including:
- losing weight if (and only if) you are carrying excess weight
- dressing against chafing (consider your underwear choices, for example)
- keeping hair in the armpits and groin (it’s part of what it’s there for)
See also: Simply The Pits: These Underarm Myths!
Take care!
Share This Post

Wheat Belly, Revised & Expanded Edition – by Dr. William Davis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This review pertains to the 2019 edition of the book, not the 2011 original, which will not have had all of the same research.
We are told, by scientific consensus, to enjoy plenty of whole grains as part of our diet. So, what does cardiologist Dr. William Davis have against wheat?
Firstly, not all grains are interchangeable, and wheat—in particular, modern strains of wheat—cannot be described as the same as the wheat of times past.
While this book does touch on the gluten aspect (and Celiac disease), and notes that modern wheat has a much higher gluten content than older strains, most of this book is about other harms that wheat can do to us.
Dr. Davis explores and explains the metabolic implications of wheat’s unique properties on organs such as our pancreas, liver, heart, and brain.
The book does also have recipes and meal plans, though in this reviewer’s opinion they were a little superfluous. Wheat is not hard to cut out unless you are living in a food desert or are experiencing food poverty, in which case, those recipes and meal plans would also not help.
Bottom line: this book, filled with plenty of actual science, makes a strong case against wheat, and again, mostly for reasons other than its gluten content. You might want to cut yours down!
Click here to check out Wheat Belly, and see if skipping the wheat could be good for you!
Share This Post
Related Posts

How To Triple Your Breast Cancer Survival Chances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping Abreast Of Your Cancer Risk
It’s the kind of thing that most people think won’t happen to them. And hopefully, it won’t!
But…
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
- *and even this depends on the type of double mastectomy and other circumstances, and technically there will always be a non-zero risk, because of complicating factors.
- Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
- That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
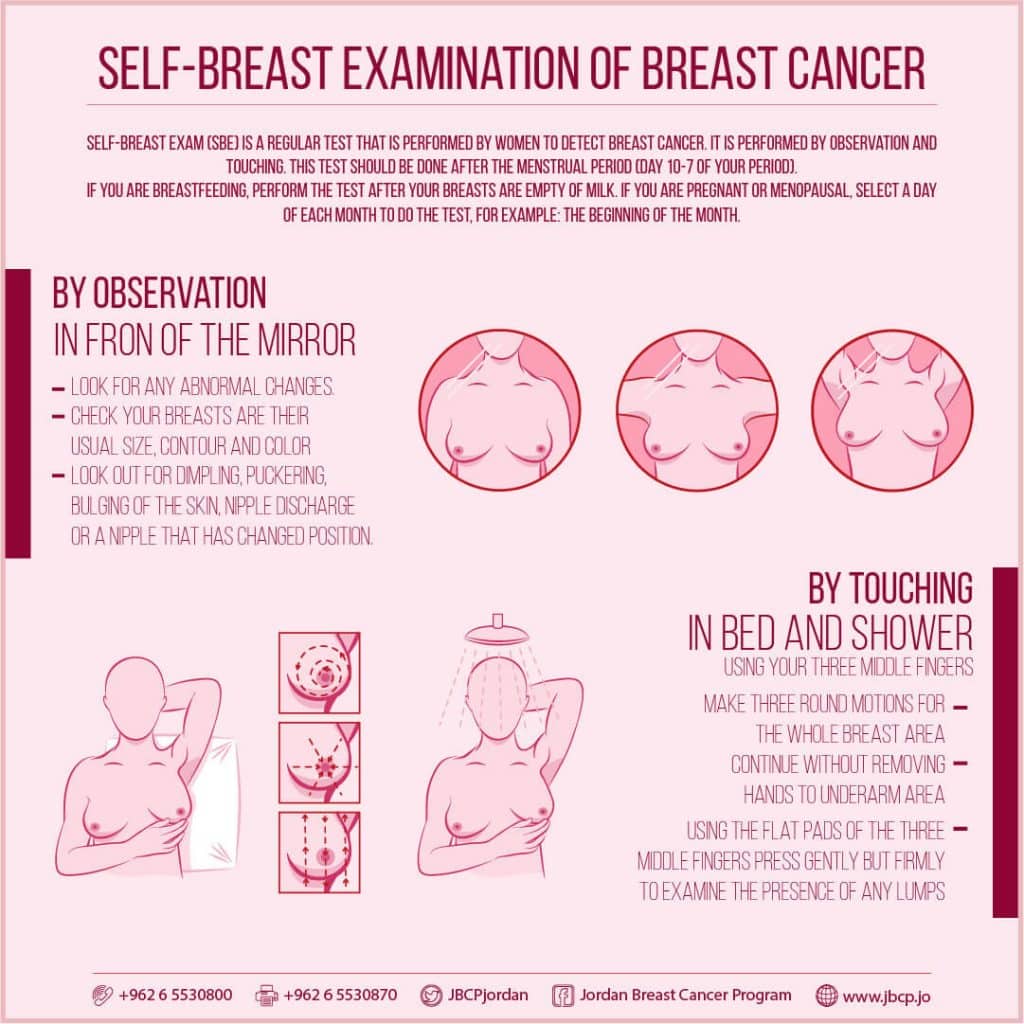
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:

(This graphic was created by the Jordan Breast Cancer Program—check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it:
Click Here To Take The Free 4-Minute Breast Health Assessment!
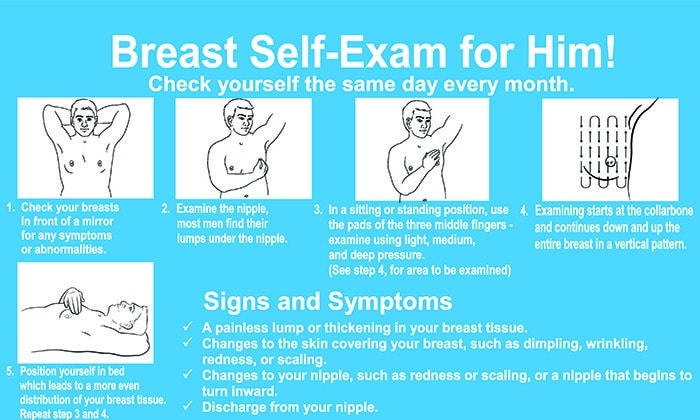
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?

So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to!
Take care of yourself; you’re important.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.

How Useful Are Our Dreams
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s In A Dream?
We were recently asked:
❝I have a question or a suggestion for coverage in your “Psychology Sunday”. Dreams: their relevance, meanings ( if any) interpretations? I just wondered what the modern psychological opinions are about dreams in general.❞
~ 10almonds subscriber
There are two main schools of thought, and one main effort to reconcile those two. The third one hasn’t quite caught on so far as to be considered a “school of thought” yet though.
The Top-Down Model (Psychoanalysts)
Psychoanalysts broadly follow the theories of Freud, or at least evolved from there. Freud was demonstrably wrong about very many things. Most of his theories have been debunked and ditched—hence the charitable “or at least evolved from there” phrasing when it comes to modern psychoanalytic schools of thought. Perhaps another day, we’ll go into all the ways Freud went wrong. However, for today, one thing he wasn’t bad at…
According to Freud, our dreams reveal our subconscious desires and fears, sometimes directly and sometimes dressed in metaphor.
Examples of literal representations might be:
- sex dreams (revealing our subconscious desires; perhaps consciously we had not thought about that person that way, or had not considered that sex act desirable)
- getting killed and dying (revealing our subconscious fear of death, not something most people give a lot of conscious thought to most of the time)
Examples of metaphorical representations might be:
- dreams of childhood (revealing our subconscious desires to feel safe and nurtured, or perhaps something else depending on the nature of the dream; maybe a return to innocence, or a clean slate)
- dreams of being pursued (revealing our subconscious fear of bad consequences of our actions/inactions, for example, responsibilities to which we have not attended, debts are a good example for many people; or social contact where the ball was left in our court and we dropped it, that kind of thing)
One can read all kinds of guides to dream symbology, and learn such arcane lore as “if you dream of your teeth crumbling, you have financial worries”, but the truth is that “this thing means that other thing” symbolic equations are not only highly personal, but also incredibly culture-bound.
For example:
- To one person, bees could be a symbol of feeling plagued by uncountable small threats; to another, they could be a symbol of abundance, or of teamwork
- One culture’s “crow as an omen of death” is another culture’s “crow as a symbol of wisdom”
- For that matter, in some cultures, white means purity; in others, it means death.
Even such classically Freudian things as dreaming of one’s mother and/or father (in whatever context) will be strongly informed by one’s own waking-world relationship (or lack thereof) with same. Even in Freud’s own psychoanalysis, the “mother” for the sake of such analysis was the person who nurtured, and the “father” was the person who drew the nurturer’s attention away, so they could be switched gender roles, or even different people entirely than one’s parents.
The only real way to know what, if anything, your dreams are trying to tell you, is to ask yourself. You can do that…
- by reflection and personal interrogation (see for example: The Easiest Way To Take Up Journaling)
- or by externalising parts of your subconscious (as in Internal Family Systems therapy)
- or by talking directly to your subconscious where it is, by means of lucid dreaming.
The idea with lucid dreaming is that since any dream character is a facet of your subconscious generated by your own mind, by talking to that character you can ask questions directly of your subconscious (the popular 2010 movie “Inception” was actually quite accurate in this regard, by the way).
To read more about how to do this kind of self-therapy through lucid dreaming, you might want to check out this book we reviewed previously; it is the go-to book of lucid dreaming enthusiasts, and will honestly give you everything you need in one go:
Lucid Dreaming: A Concise Guide to Awakening in Your Dreams and in Your Life – by Dr. Stephen LaBerge
The Bottom-Up Model (Neuroscientists)
This will take a lot less writing, because it’s practically a null hypothesis (i.e., the simplest default assumption before considering any additional evidence that might support or refute it; usually some variant of “nothing unusual going on here”).
The Bottom-Up model holds that our brains run regular maintenance cycles during REM sleep (a biological equivalent of defragging a computer), and the brain interprets these pieces of information flying by and, because of the mind’s tendency to look for patterns, fills in the rest (much like how modern generative AI can “expand” a source image to create more of the same and fill in the blanks), resulting in the often narratively wacky, but ultimately random, vivid hallucinations that we call dreams.
The Hybrid Model (per Cartwright, 2012)
This is really just one woman’s vision, but it’s an incredibly compelling one, that takes the Bottom-Up model and asks “what if we did all that bio-stuff, and then our subconscious mind influenced the interpretation of the random patterns, to create dreams that are subjectively meaningful, and thus do indeed represent our subconscious?
It’s best explained in her own words, though, so it’s time for another book recommendation (we’ve reviewed this one before, too):
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

I have a stuffy nose, how can I tell if it’s hay fever, COVID or something else?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hay fever (also called allergic rhinitis) affects 24% of Australians. Symptoms include sneezing, a runny nose (which may feel blocked or stuffy) and itchy eyes. People can also experience an itchy nose, throat or ears.
But COVID is still spreading, and other viruses can cause cold-like symptoms. So how do you know which one you’ve got?

Lysenko Andrii/Shutterstock Remind me, how does hay fever cause symptoms?
Hay fever happens when a person has become “sensitised” to an allergen trigger. This means a person’s body is always primed to react to this trigger.
Triggers can include allergens in the air (such as pollen from trees, grasses and flowers), mould spores, animals or house dust mites which mostly live in people’s mattresses and bedding, and feed on shed skin.
When the body is exposed to the trigger, it produces IgE (immunoglobulin E) antibodies. These cause the release of many of the body’s own chemicals, including histamine, which result in hay fever symptoms.
People who have asthma may find their asthma symptoms (cough, wheeze, tight chest or trouble breathing) worsen when exposed to airborne allergens. Spring and sometimes into summer can be the worst time for people with grass, tree or flower allergies.
However, animal and house dust mite symptoms usually happen year-round.

Ryegrass pollen is a common culprit. bangku ceria/Shutterstock What else might be causing my symptoms?
Hay fever does not cause a fever, sore throat, muscle aches and pains, weakness, loss of taste or smell, nor does it cause you to cough up mucus.
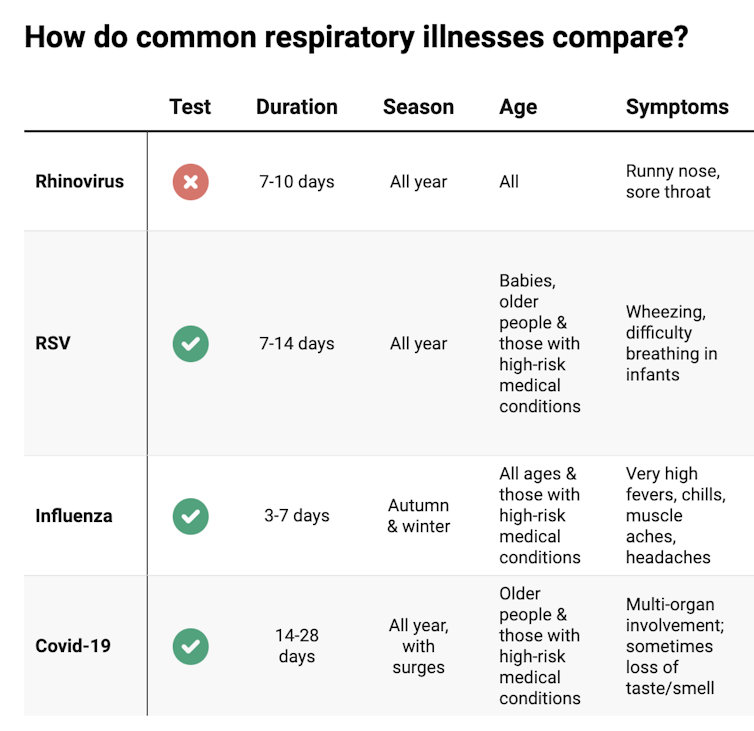
These symptoms are likely to be caused by a virus, such as COVID, influenza, respiratory syncytial virus (RSV) or a “cold” (often caused by rhinoviruses). These conditions can occur all year round, with some overlap of symptoms:

Natasha Yates/The Conversation COVID still surrounds us. RSV and influenza rates appear higher than before the COVID pandemic, but it may be due to more testing.
So if you have a fever, sore throat, muscle aches/pains, weakness, fatigue, or are coughing up mucus, stay home and avoid mixing with others to limit transmission.
People with COVID symptoms can take a rapid antigen test (RAT), ideally when symptoms start, then isolate until symptoms disappear. One negative RAT alone can’t rule out COVID if symptoms are still present, so test again 24–48 hours after your initial test if symptoms persist.
You can now test yourself for COVID, RSV and influenza in a combined RAT. But again, a negative test doesn’t rule out the virus. If your symptoms continue, test again 24–48 hours after the previous test.
If it’s hay fever, how do I treat it?
Treatment involves blocking the body’s histamine release, by taking antihistamine medication which helps reduce the symptoms.
Doctors, nurse practitioners and pharmacists can develop a hay fever care plan. This may include using a nasal spray containing a topical corticosteroid to help reduce the swelling inside the nose, which causes stuffiness or blockage.
Nasal sprays need to delivered using correct technique and used over several weeks to work properly. Often these sprays can also help lessen the itchy eyes of hay fever.
Drying bed linen and pyjamas inside during spring can lessen symptoms, as can putting a smear of Vaseline in the nostrils when going outside. Pollen sticks to the Vaseline, and gently blowing your nose later removes it.
People with asthma should also have an asthma plan, created by their doctor or nurse practitioner, explaining how to adjust their asthma reliever and preventer medications in hay fever seasons or on allergen exposure.
People with asthma also need to be alert for thunderstorms, where pollens can burst into tinier particles, be inhaled deeper in the lungs and cause a severe asthma attack, and even death.
What if it’s COVID, RSV or the flu?
Australians aged 70 and over and others with underlying health conditions who test positive for COVID are eligible for antivirals to reduce their chance of severe illness.
Most other people with COVID, RSV and influenza will recover at home with rest, fluids and paracetamol to relieve symptoms. However some groups are at greater risk of serious illness and may require additional treatment or hospitalisation.
For RSV, this includes premature infants, babies 12 months and younger, children under two who have other medical conditions, adults over 75, people with heart and lung conditions, or health conditions that lessens the immune system response.
For influenza, people at higher risk of severe illness are pregnant women, Aboriginal people, people under five or over 65 years, or people with long-term medical conditions, such as kidney, heart, lung or liver disease, diabetes and decreased immunity.
If you’re concerned about severe symptoms of COVID, RSV or influenza, consult your doctor or call 000 in an emergency.
If your symptoms are mild but persist, and you’re not sure what’s causing them, book an appointment with your doctor or nurse practitioner. Although hay fever season is here, we need to avoid spreading other serious infectious.
For more information, you can call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria); use the online Symptom Checker; or visit healthdirect.gov.au or the Australian Society of Clinical Immunology and Allergy.
Deryn Thompson, Eczema and Allergy Nurse; Lecturer, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: