The Mind-Gut Connection – by Dr. Emeran Mayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about the mind-gut connection before, so what makes this one stand out?
Firstly, it’s a lot more comprehensive than the usual “please, we’re begging you, eat some fiber”.
And yes, of course that’s part of it. Prebiotics, probiotics, reduce fried and processed foods, reduce sugar/alcohol, reduce meat, and again, eat some greenery.
But where this book really comes into its own is looking more thoroughly at the gut microbiota and their function. Dr. Mayer goes well beyond “there are good and bad bacteria” and looks at the relationship each of them have with the body’s many hormones, and especially neurotransmitters like serotonin and dopamine.
He also looks at the two-way connection between brain and gut. Yes, our gut gives us “gut feelings”, but 10% of communication between the brain and gut is in the other direction; he explores what that means for us, too.
Finally, he does give a lot of practical advice, not just dietary but also behavioral, to make the most of our mind-gut connection and make it work for our health, rather than against it.
Bottom line: this is the best book on the brain-gut connection that this reviewer has read so far, and certainly the most useful if you already know about gut-healthy nutrition, and are looking to take your understanding to the next level.
Click here to check out The Mind-Gut Connection, and start making yours work for your benefit!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Get Past Executive Dysfunction
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In mathematics, there is a thing called the “travelling salesman problem”, and it is hard. Not just subjectively; it is classified in mathematical terms as an “NP-hard problem”, wherein NP stands for “nondeterministic polynomial”.
The problem is: a travelling salesman must visit a certain list of cities, order undetermined, by the shortest possible route that visits them all.
To work out what the shortest route is involves either very advanced mathematics, or else solving it by brute force, which means measuring every possible combination order (which number gets exponentially larger very quickly after the first few cities) and then selecting the shortest.
Why are we telling you this?
Executive dysfunction’s analysis paralysis
Executive dysfunction is the state of knowing you have things to do, wanting to do them, intending to do them, and then simply not doing them.
Colloquially, this can be called “analysis paralysis” and is considered a problem of planning and organizing, as much as it is a problem of initiating tasks.
Let’s give a simple example:
You wake up in the morning, and you need to go to the bathroom. But the bathroom will be cold, so you’ll want to get dressed first. However, it will be uncomfortable to get dressed while you still need to use the bathroom, so you contemplate doing that first. Those two items are already a closed loop now. You’re thirsty, so you want to have a drink, but the bathroom is calling to you. Sitting up, it’s colder than under the covers, so you think about getting dressed. Maybe you should have just a sip of water first. What else do you need to do today anyway? You grab your phone to check, drink untouched, clothes unselected, bathroom unvisited.
That was a simple example; now apply that to other parts of your day that have much more complex planning possible.
This is like the travelling salesman problem, except that now, some things are better if done before or after certain other things. Sometimes, possibly, they are outright required to be done before or after certain other things.
So you have four options:
- Solve the problem of your travelling-salesman-like tasklist using advanced mathematics (good luck if you don’t have advanced mathematics)
- Solve the problem by brute force, calculating all possible variations and selecting the shortest (good luck getting that done the same day)
- Go with a gut feeling and stick to it (people without executive dysfunction do this)
- Go towards the nearest item, notice another item on the way, go towards that, notice a different item on the way there, and another one, get stuck for a while choosing between those two, head towards one, notice another one, and so on until you’ve done a very long scenic curly route that has narrowly missed all of your targetted items (this is the executive dysfunction approach).
So instead, just pick one, do it, pick another one, do it, and so forth.
That may seem “easier said than done”, but there are tools available…
Task zero
We’ve mentioned this before in the little section at the top of our daily newsletter that we often use for tips.
One of the problems that leads to executive function is a shortage of “working memory”, like the RAM of a computer, so it’s easy to get overwhelmed with lists of things to do.
So instead, hold only two items in your mind:
- Task zero: the thing you are doing right now
- Task one: the thing you plan to do next
When you’ve completed task zero, move on to task one, renaming it task zero, and select a new task one.
With this approach, you will never:
- Think “what did I come into this room for?”
- Get distracted by alluring side-quests
Do not get corrupted by the cursed artefact
In fantasy, and occasionally science fiction, there is a trope: an item that people are drawn towards, but which corrupts them, changes their motivations and behaviors for the worse, as well as making them resistant to giving the item up.
An archetypal example of this would be the One Ring from The Lord of the Rings.
It’s easy to read/watch and think “well I would simply not be corrupted by the cursed artefact”.
And then pick up one’s phone to open the same three apps in a cycle for the next 40 minutes.
This is because technology that is designed to be addictive hijacks our dopamine processing, and takes advantage of executive dysfunction, while worsening it.
There are some ways to mitigate this:
Rebalancing Dopamine (Without “Dopamine Fasting”)
…but one way to avoid it entirely is to mentally narrate your choices. It’s a lot harder to make bad choices with an internal narrator going:
- “She picked up her phone absent-mindedly, certain that this time it really would be only a few seconds”
- “She picked up her phone for the eleventy-third time”
- “Despite her plan to put her shoes on, she headed instead for the kitchen”
This method also helps against other bad choices aside from those pertaining to executive dysfunction, too:
- “Abandoning her plan to eat healthily, she lingered in the confectionary aisle, scanning the shelves for sugary treats”
- “Monday morning will be the best time to start my new exercise regime”, she thought, for the 35th week so far this year
Get pharmaceutical or nutraceutical help
While it’s not for everyone, many people with executive dysfunction benefit from ADHD meds. However, they have their pros and cons (perhaps we’ll do a run-down one of these days).
There are also gentler options that can significantly ameliorate executive dysfunction, for example:
Bacopa Monnieri: A Well-Evidenced Cognitive Enhancer For Focus & More
Enjoy!
Share This Post
-
Homeopathy: Evidence So Tiny That It’s Not there?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Homeopathy: Evidence So Tiny That It’s Not There?
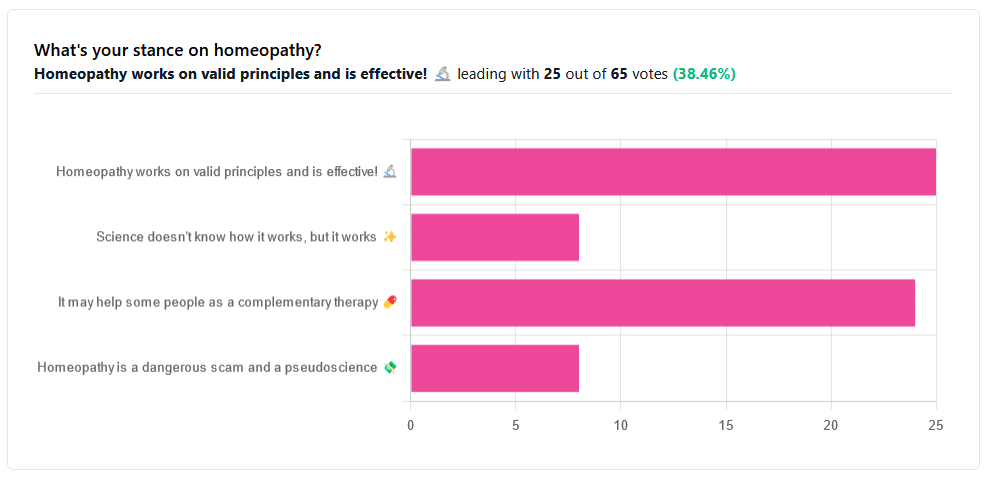
Yesterday, we asked you your opinions on homeopathy. The sample size of responses was a little lower than we usually get, but of those who did reply, there was a clear trend:
- A lot of enthusiasm for “Homeopathy works on valid principles and is effective”
- Near equal support for “It may help some people as a complementary therapy”
- Very few people voted for “Science doesn’t know how it works, but it works”; this is probably because people who considered voting for this, voted for the more flexible “It may help some people as a complementary therapy” instead.
- Very few people considered it a dangerous scam and a pseudoscience.
So, what does the science say?
Well, let us start our investigation by checking out the position of the UK’s National Health Service, an organization with a strong focus on providing the least expensive treatments that are effective.
Since homeopathy is very inexpensive to arrange, they will surely want to put it atop their list of treatments, right?
❝Homeopathy is a “treatment” based on the use of highly diluted substances, which practitioners claim can cause the body to heal itself.
There’s been extensive investigation of the effectiveness of homeopathy. There’s no good-quality evidence that homeopathy is effective as a treatment for any health condition.❞
The NHS actually has a lot more to say about that, and you can read their full statement here.
But that’s just one institution. Here’s what Australia’s National Health and Medical Research Council had to say:
❝There was no reliable evidence from research in humans that homeopathy was effective for treating the range of health conditions considered: no good-quality, well-designed studies with enough participants for a meaningful result reported either that homeopathy caused greater health improvements than placebo, or caused health improvements equal to those of another treatment❞
You can read their full statement here.
The American FDA, meanwhile, have a stronger statement:
❝Homeopathic drug products are made from a wide range of substances, including ingredients derived from plants, healthy or diseased animal or human sources, minerals and chemicals, including known poisons. These products have the potential to cause significant and even permanent harm if they are poorly manufactured, since that could lead to contaminated products or products that have potentially toxic ingredients at higher levels than are labeled and/or safe, or if they are marketed as substitute treatments for serious or life-threatening diseases and conditions, or to vulnerable populations.❞
You can read their full statement here.
Homeopathy is a dangerous scam and a pseudoscience: True or False?
False and True, respectively, mostly.
That may be a confusing answer, so let’s elaborate:
- Is it dangerous? Mostly not; it’s mostly just water. However, two possibilities for harm exist:
- Careless preparation could result in a harmful ingredient still being present in the water—and because of the “like cures like” principle, many of the ingredients used in homeopathy are harmful, ranging from heavy metals to plant-based neurotoxins. However, the process of “ultra-dilution” usually removes these so thoroughly that they are absent or otherwise scientifically undetectable.
- Placebo treatment has its place, but could result in “real” treatment going undelivered. This can cause harm if the “real” treatment was critically needed, especially if it was needed on a short timescale.
- Is it a scam? Probably mostly not; to be a scam requires malintent. Most practitioners probably believe in what they are practising.
- Is it a pseudoscience? With the exception that placebo effect has been highly studied and is a very valid complementary therapy… Yes, aside from that it is a pseudoscience. There is no scientific evidence to support homeopathy’s “like cures like” principle, and there is no scientific evidence to support homeopathy’s “water memory” idea. On the contrary, they go against the commonly understood physics of our world.
It may help some people as a complementary therapy: True or False?
True! Not only is placebo effect very well-studied, but best of all, it can still work as a placebo even if you know that you’re taking a placebo… Provided you also believe that!
Science doesn’t know how it works, but it works: True or False?
False, simply. At best, it performs as a placebo.
Placebo is most effective when it’s a remedy against subjective symptoms, like pain.
However, psychosomatic effect (the effect that our brain has on the rest of our body, to which it is very well-connected) can mean that placebo can also help against objective symptoms, like inflammation.
After all, our body, directed primarily by the brain, can “decide” what immunological defenses to deploy or hold back, for example. This is why placebo can help with conditions as diverse as arthritis (an inflammatory condition) or diabetes (an autoimmune condition, and/or a metabolic condition, depending on type).
Here’s how homeopathy measures up, for those conditions:
(the short answer is “no better than placebo”)
Homeopathy works on valid principles and is effective: True or False?
False, except insofar as placebo is a valid principle and can be effective.
The stated principles of homeopathy—”like cures like” and “water memory”—have no scientific basis.
We’d love to show the science for this, but we cannot prove a negative.
However, the ideas were conceived in 1796, and are tantamount to alchemy. A good scientific attitude means being open-minded to new ideas and testing them. In homeopathy’s case, this has been done, extensively, and more than 200 years of testing later, homeopathy has consistently performed equal to placebo.
In summary…
- If you’re enjoying homeopathic treatment and that’s working for you, great, keep at it.
- If you’re open-minded to enjoying a placebo treatment that may benefit you, be careful, but don’t let us stop you.
- If your condition is serious, please do not delay seeking evidence-based medical treatment.
Share This Post
-
Apple vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing apple to pineapple, we picked the pineapple.
Why?
An apple a day may keep the doctor away, but pineapples are heavier and armored and spiky and generally much more intimidating.
More seriously, apples are great but we say pineapples have the better nutritional and phytochemical properties overall:
In terms of macros, actually apples win this first round, albeit marginally; the two fruits are equal on carbs, while apple has a little more fiber and pineapple has a (very) little more protein. This makes the fiber content the deciding factor, so apples do win this one, even if by just 1g/100g difference.
When it comes to vitamins, however, apples have more of vitamins E and K, while pineapple has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline. The margins of difference are equally generous on both sides, so this is a clear and overwhelming win for pineapple (including 10x more vitamin C than apples, which are themselves considered a good source of vitamin C)
In the category of minerals, apples have slightly more phosphorus, and pineapple has a lot more calcium, copper, iron, magnesium, manganese, potassium, selenium, and zinc. Another easy win for pineapple.
Pineapples are not only also higher in polyphenols, but also contain bromelain, a powerful anti-inflammatory group of enzymes that are unique to pineapple—you can read about it in the link below!
Meanwhile, pineapple wins the day in our head-to-head here, but as ever when it comes to a plurality of healthy things, do enjoy either or both! Diversity is good.
Want to learn more?
You might like to read:
Bromelain vs Inflammation & Much More
Enjoy!
Share This Post
Related Posts
-
Topping Up Testosterone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Testosterone Drop
Testosterone levels decline amongst men over a certain age. Exactly when depends on the individual and also how we measure it, but the age of 45 is a commonly-given waypoint for the start of this decline.
(the actual start is usually more like 20, but it’s a very small decline then, and speeds up a couple of decades later)
This has been called “the male menopause”, or “the andropause”.
Both terms are a little misleading, but for lack of a better term, “andropause” is perhaps not terrible.
Why “the male menopause” is misleading:
To call it “the male menopause” suggests that this is when men’s menstruation stops. Which for cis men at the very least, is simply not a thing they ever had in the first place, to stop (and for trans men it’s complicated, depending on age, hormones, surgeries, etc).
Why “the andropause” is misleading:
It’s not a pause, and unlike the menopause, it’s not even a stop. It’s just a decline. It’s more of an andro-pitter-patter-puttering-petering-out.
Is there a better clinical term?
Objectively, there is “late-onset hypogonadism” but that is unlikely to be taken up for cultural reasons—people stigmatize what they see as a loss of virility.
Terms aside, what are the symptoms?
❝Andropause or late-onset hypogonadism is a common disorder which increases in prevalence with advancing age. Diagnosis of late-onset of hypogonadism is based on presence of symptoms suggestive of testosterone deficiency – prominent among them are sexual symptoms like…❞
…and there we’d like to continue the quotation, but if we list the symptoms here, it won’t get past a lot of filters because of the words used. So instead, please feel free to click through:
Source: Andropause: Current concepts
Can it be safely ignored?
If you don’t mind the sexual symptoms, then mostly, yes!
However, there are a few symptoms we can mention here that are not so subjective in their potential for harm:
- Depression
- Loss of muscle mass
- Increased body fat
Depression kills, so this does need to be taken seriously. See also:
The Mental Health First-Aid That You’ll Hopefully Never Need
(the above is a guide to managing depression, in yourself or a loved one)
Loss of muscle mass means being less robust against knocks and falls later in life
Loss of muscle mass also means weaker bones (because the body won’t make bones stronger than it thinks they need to be, so bone will follow muscle in this regard—in either direction)
See also:
- Resistance Is Useful! (Especially As We Get Older)
- Protein vs Sarcopenia
- Fall Special (How to Proof Yourself Against Falls)
Increased body fat means increased risk of diabetes and heart disease, as a general rule of thumb, amongst other problems.
Will testosterone therapy help?
That’s something to discuss with your endocrinologist, but for most men whose testosterone levels are lower than is ideal for them, then yes, taking testosterone to bring them [back] to “normal” levels can make you happier and healthier (though it’s certainly not a cure-all).
See for example:
Testosterone Therapy Improves […] and […] in Hypogonadal Men
(Sorry, we’re not trying to be clickbaity, there are just some words we can’t use without encountering software problems)
Here’s a more comprehensive study that looked at 790 men aged 65 or older, with testosterone levels below a certain level. It looked at the things we can’t mention here, as well as physical function and general vitality:
❝The increase in testosterone levels was associated with significantly increased […] activity, as assessed by the Psychosexual Daily Questionnaire (P<0.001), as well as significantly increased […] desire and […] function.
The percentage of men who had an increase of at least 50 m in the 6-minute walking distance did not differ significantly between the two study groups in the Physical Function Trial but did differ significantly when men in all three trials were included (20.5% of men who received testosterone vs. 12.6% of men who received placebo, P=0.003).
Testosterone had no significant benefit with respect to vitality, as assessed by the Functional Assessment of Chronic Illness Therapy–Fatigue scale, but men who received testosterone reported slightly better mood and lower severity of depressive symptoms than those who received placebo❞
Source: Effects of Testosterone Treatment in Older Men
We strongly recommend, by the way, when a topic is of interest to you to read the paper itself, because even the extract above contains some subjectivity, for example what is “slightly better”, and what is “no significant benefit”.
That “slightly better mood and lower severity of depressive symptoms”, for example, has a P value of 0.004 in their data, which is an order of magnitude more significant than the usual baseline for significance (P<0.05).
And furthermore, that “no significant benefit with respect to vitality” is only looking at either the primary outcome aggregated goal or the secondary FACIT score whose secondary outcome had a P value of 0.06, which just missed the cut-off for significance, and neglects to mention that all the other secondary outcome metrics for men involved in the vitality trial were very significant (ranging from P=0.04 to P=0.001)
Click here to see the results table for the vitality trial
Will it turn me into a musclebound angry ragey ‘roidmonster?
Were you that kind of person before your testosterone levels declined? If not, then no.
Testosterone therapy seeks only to return your testosterone levels to where they were, and this is done through careful monitoring and adjustment. It’d take a lot more than (responsible) endocrinologist-guided hormonal therapy to turn you into Marvel’s “Wolverine”.
Is testosterone therapy safe?
A question to take to your endocrinologist because everyone’s physiology is different, but a lot of studies do support its general safety for most people who are prescribed it.
As with anything, there are risks to be aware of, though. Perhaps the most critical risk is prostate cancer, and…
❝In a large meta-analysis of 18 prospective studies that included over 3500 men, there was no association between serum androgen levels and the risk of prostate cancer development
For men with untreated prostate cancer on active surveillance, TRT remains controversial. However, several studies have shown that TRT is not associated with progression of prostate cancer as evidenced by either PSA progression or gleason grade upstaging on repeat biopsy.
Men on TRT should have frequent PSA monitoring; any major change in PSA (>1 ng/mL) within the first 3-6 months may reflect the presence of a pre-existing cancer and warrants cessation of therapy❞
Those are some select extracts, but any of this may apply to you or your loved one, we recommend to read in full about this and other risks:
Risks of testosterone replacement therapy in men
See also: Prostate Health: What You Should Know
Beyond that… If you are prone to baldness, then taking testosterone will increase that tendency. If that’s a problem for you, then it’s something to know about. There are other things you can take/use for that in turn, so maybe we’ll do a feature on those one of these days!
For now, take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
100 Hikes of a Lifetime – by Kate Siber
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is published by National Geographic, so you can imagine the quality of the photos throughout.
Inside, and after a general introduction and guide to gear and packing appropriately, it’s divided into continents, with a diverse array of “trips of a lifetime” for anyone who enjoys hiking.
It’s not a narrative book, rather, it is a guide, a little in the style of “Lonely Planet”, with many “know before you go” tips, information about the best time to go, difficult level, alternative routes if you want to get most of the enjoyment while having an easier time of it (or, conversely, if you want to see some extra sights along the way), and what to expect at all points.
Where the book really excels is in balancing inspiration with information. There are some books that make you imagine being in a place, but you’ll never actually go there. There are other books that are technical manuals but not very encouraging. This one does both; it provides the motivation and the “yes, you really can, here’s how” information that, between them, can actually get you packing and on your way.
Bottom line: if you yearn for breathtaking views and time in the great outdoors, but aren’t sure where to start, this will give you an incredible menu to choose from, and give you the tools to go about doing it.
Click here to check out 100 Hikes Of A Lifetime, and live it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Long-Covid Patients Are Frustrated That Federal Research Hasn’t Found New Treatments
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Erica Hayes, 40, has not felt healthy since November 2020 when she first fell ill with covid.
Hayes is too sick to work, so she has spent much of the last four years sitting on her beige couch, often curled up under an electric blanket.
“My blood flow now sucks, so my hands and my feet are freezing. Even if I’m sweating, my toes are cold,” said Hayes, who lives in Western Pennsylvania. She misses feeling well enough to play with her 9-year-old son or attend her 17-year-old son’s baseball games.
Along with claiming the lives of 1.2 million Americans, the covid-19 pandemic has been described as a mass disabling event. Hayes is one of millions of Americans who suffer from long covid. Depending on the patient, the condition can rob someone of energy, scramble the autonomic nervous system, or fog their memory, among many other http://symptoms.in/ addition to the brain fog and chronic fatigue, Hayes’ constellation of symptoms includes frequent hives and migraines. Also, her tongue is constantly swollen and dry.
“I’ve had multiple doctors look at it and tell me they don’t know what’s going on,” Hayes said about her tongue.
Estimates of prevalence range considerably, depending on how researchers define long covid in a given study, but the Centers for Disease Control and Prevention puts it at 17 million adults.
Despite long covid’s vast reach, the federal government’s investment in researching the disease — to the tune of $1.15 billion as of December — has so far failed to bring any new treatments to market.
This disappoints and angers the patient community, who say the National Institutes of Health should focus on ways to stop their suffering instead of simply trying to understand why they’re suffering.
“It’s unconscionable that more than four years since this began, we still don’t have one FDA-approved drug,” said Meighan Stone, executive director of the Long COVID Campaign, a patient-led advocacy organization. Stone was among several people with long covid who spoke at a workshop hosted by the NIH in September where patients, clinicians, and researchers discussed their priorities and frustrations around the agency’s approach to long-covid research.
Some doctors and researchers are also critical of the agency’s research initiative, called RECOVER, or Researching COVID to Enhance Recovery. Without clinical trials, physicians specializing in treating long covid must rely on hunches to guide their clinical decisions, said Ziyad Al-Aly, chief of research and development with the VA St Louis Healthcare System.
“What [RECOVER] lacks, really, is clarity of vision and clarity of purpose,” said Al-Aly, saying he agrees that the NIH has had enough time and money to produce more meaningful progress.
Now the NIH is starting to determine how to allocate an additional $662 million of funding for long-covid research, $300 million of which is earmarked for clinical trials. These funds will be allocated over the next four http://years.at/ the end of October, RECOVER issued a request for clinical trial ideas that look at potential therapies, including medications, saying its goal is “to work rapidly, collaboratively, and transparently to advance treatments for Long COVID.”
This turn suggests the NIH has begun to respond to patients. This has stirred cautious optimism among those who say that the agency’s approach to long covid has lacked urgency in the search for effective treatments.Stone calls this $300 million a down payment. She warns it’s going to take a lot more money to help people like Hayes regain some degree of health.“There really is a burden to make up this lost time now,” Stone said.
The NIH told KFF Health News and NPR via email that it recognizes the urgency in finding treatments. But to do that, there needs to be an understanding of the biological mechanisms that are making people sick, which is difficult to do with post-infectious conditions.
That’s why it has funded research into how long covid affects lung function, or trying to understand why only some people are afflicted with the condition.
Good Science Takes Time
In December 2020, Congress appropriated $1.15 billion for the NIH to launch RECOVER, raising hopes in the long-covid patient community.
Then-NIH Director Francis Collins explained that RECOVER’s goal was to better understand long covid as a disease and that clinical trials of potential treatments would come later.
According to RECOVER’s website, it has funded eight clinical trials to test the safety and effectiveness of an experimental treatment or intervention. Just one of those trials has published results.
On the other hand, RECOVER has supported more than 200 observational studies, such as research on how long covid affects pulmonary function and on which symptoms are most common. And the initiative has funded more than 40 pathobiology studies, which focus on the basic cellular and molecular mechanisms of long covid.
RECOVER’s website says this research has led to crucial insights on the risk factors for developing long covid and on understanding how the disease interacts with preexisting conditions.
It notes that observational studies are important in helping scientists to design and launch evidence-based clinical trials.
Good science takes time, said Leora Horwitz, the co-principal investigator for the RECOVER-Adult Observational Cohort at New York University. And long covid is an “exceedingly complicated” illness that appears to affect nearly every organ system, she said.
This makes it more difficult to study than many other diseases. Because long covid harms the body in so many ways, with widely variable symptoms, it’s harder to identify precise targets for treatment.
“I also will remind you that we’re only three, four years into this pandemic for most people,” Horwitz said. “We’ve been spending much more money than this, yearly, for 30, 40 years on other conditions.”
NYU received nearly $470 million of RECOVER funds in 2021, which the institution is using to spearhead the collection of data and biospecimens from up to 40,000 patients. Horwitz said nearly 30,000 are enrolled so far.
This vast repository, Horwitz said, supports ongoing observational research, allowing scientists to understand what is happening biologically to people who don’t recover after an initial infection — and that will help determine which clinical trials for treatments are worth undertaking.
“Simply trying treatments because they are available without any evidence about whether or why they may be effective reduces the likelihood of successful trials and may put patients at risk of harm,” she said.
Delayed Hopes or Incremental Progress?
The NIH told KFF Health News and NPR that patients and caregivers have been central to RECOVER from the beginning, “playing critical roles in designing studies and clinical trials, responding to surveys, serving on governance and publication groups, and guiding the initiative.”But the consensus from patient advocacy groups is that RECOVER should have done more to prioritize clinical trials from the outset. Patients also say RECOVER leadership ignored their priorities and experiences when determining which studies to fund.
RECOVER has scored some gains, said JD Davids, co-director of Long COVID Justice. This includes findings on differences in long covid between adults and kids.But Davids said the NIH shouldn’t have named the initiative “RECOVER,” since it wasn’t designed as a streamlined effort to develop treatments.
“The name’s a little cruel and misleading,” he said.
RECOVER’s initial allocation of $1.15 billion probably wasn’t enough to develop a new medication to treat long covid, said Ezekiel J. Emanuel, co-director of the University of Pennsylvania’s Healthcare Transformation Institute.
But, he said, the results of preliminary clinical trials could have spurred pharmaceutical companies to fund more studies on drug development and test how existing drugs influence a patient’s immune response.
Emanuel is one of the authors of a March 2022 covid roadmap report. He notes that RECOVER’s lack of focus on new treatments was a problem. “Only 15% of the budget is for clinical studies. That is a failure in itself — a failure of having the right priorities,” he told KFF Health News and NPR via email.
And though the NYU biobank has been impactful, Emanuel said there needs to be more focus on how existing drugs influence immune response.
He said some clinical trials that RECOVER has funded are “ridiculous,” because they’ve focused on symptom amelioration, for example to study the benefits of over-the-counter medication to improve sleep. Other studies looked at non-pharmacological interventions, such as exercise and “brain training” to help with cognitive fog.
People with long covid say this type of clinical research contributes to what many describe as the “gaslighting” they experience from doctors, who sometimes blame a patient’s symptoms on anxiety or depression, rather than acknowledging long covid as a real illness with a physiological basis.
“I’m just disgusted,” said long-covid patient Hayes. “You wouldn’t tell somebody with diabetes to breathe through it.”
Chimére L. Sweeney, director and founder of the Black Long Covid Experience, said she’s even taken breaks from seeking treatment after getting fed up with being told that her symptoms were due to her diet or mental health.
“You’re at the whim of somebody who may not even understand the spectrum of long covid,” Sweeney said.
Insurance Battles Over Experimental Treatments
Since there are still no long-covid treatments approved by the Food and Drug Administration, anything a physician prescribes is classified as either experimental — for unproven treatments — or an off-label use of a drug approved for other conditions. This means patients can struggle to get insurance to cover prescriptions.
Michael Brode, medical director for UT Health Austin’s Post-COVID-19 Program — said he writes many appeal letters. And some people pay for their own treatment.
For example, intravenous immunoglobulin therapy, low-dose naltrexone, and hyperbaric oxygen therapy are all promising treatments, he said.
For hyperbaric oxygen, two small, randomized controlled studies show improvements for the chronic fatigue and brain fog that often plague long-covid patients. The theory is that higher oxygen concentration and increased air pressure can help heal tissues that were damaged during a covid infection.
However, the out-of-pocket cost for a series of sessions in a hyperbaric chamber can run as much as $8,000, Brode said.
“Am I going to look a patient in the eye and say, ‘You need to spend that money for an unproven treatment’?” he said. “I don’t want to hype up a treatment that is still experimental. But I also don’t want to hide it.”
There’s a host of pharmaceuticals that have promising off-label uses for long covid, said microbiologist Amy Proal, president and chief scientific officer at the Massachusetts-based PolyBio Research Foundation. For instance, she’s collaborating on a clinical study that repurposes two HIV drugs to treat long covid.
Proal said research on treatments can move forward based on what’s already understood about the disease. For instance, she said that scientists have evidence — partly due to RECOVER research — that some patients continue to harbor small amounts of viral material after a covid infection. She has not received RECOVER funds but is researching antivirals.
But to vet a range of possible treatments for the millions suffering now — and to develop new drugs specifically targeting long covid — clinical trials are needed. And that requires money.
Hayes said she would definitely volunteer for an experimental drug trial. For now, though, “in order to not be absolutely miserable,” she said she focuses on what she can do, like having dinner with her http://family.at/ the same time, Hayes doesn’t want to spend the rest of her life on a beige couch.
RECOVER’s deadline to submit research proposals for potential long-covid treatments is Feb. 1.
This article is from a partnership that includes NPR and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: