The Midlife Cyclist – by Phil Cavell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether stationary cycling in your living room, or competing in the Tour de France, there’s a lot more to cycling than “push the pedals”—if you want to get good benefits and avoid injury, in any case.
This book explores the benefits of different kinds of cycling, the biomechanics of various body positions, and the physiology of different kinds of performance, and the impact these things have on everything from your joints to your heart to your telomeres.
The style is very much conversational, with science included, and a readiness to acknowledge in cases where the author is guessing or going with a hunch, rather than something being well-evidenced. This kind of honesty is always good to see, and it doesn’t detract from where the science is available and clear.
One downside for some readers will be that while Cavell does endeavour to cover sex differences in various aspects of how they relate to the anatomy and physiology (mostly: the physiology) of cycling, the book is written from a male perspective and the author clearly understands that side of things better. For other readers, of course, this will be a plus.
Bottom line: if you enjoy cycling, or you’re thinking of taking it up but it seems a bit daunting because what if you do it wrong and need a knee replacement in a few years or what if you hurt your spine or something, then this is the book to set your mind at ease, and put you on the right track.
Click here to check out The Midlife Cyclist, and enjoy the cycle of life!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tuna Steak with Protein Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Yes, it’s protein on protein today, and it’s all healthy.
You will need (per person)
- 1 tuna steak
- 1 400g/12oz can mixed beans, drained & rinsed
- 1 tsp capers
- 2 tsp black pepper, coarse ground
- 1 red chili, chopped
- 1 lime, cut into wedges
- ½ tsp white wine vinegar
- Extra virgin olive oil, for cooking
- Garnish: chopped parsley
Method
(we suggest you read everything at least once before doing anything)
1) Put the beans in a bowl, mixing in the capers, vinegar, and 1 tsp of the black pepper
2) Gently rub a little olive oil onto each side of the tuna steak, and season with the remainder of the black pepper (as in, the other tsp, not the rest of what you have in the house).
3) Heat a ridged grill pan until hot, and then cook the tuna for around 3 minutes on each side. Do not jiggle it! Do not slide it, and definitely do not stir it. Just gently turn it over when necessary. The edges should be cooked, and the inside should still be pink (it’s easy to forget when it comes from a can, but remember tuna is usually eaten raw)
4) Serve, sprinkling with the chopped chili and garnishing with the parsley. The lime wedges go on the side for squeezing at the table.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Protein: How Much Do We Need, Really?
- Salmon vs Tuna – Which is Healthier?
- Cilantro vs Parsley – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
Oats vs Pearl Barley – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing oats to pearl barley, we picked the oats.
Why?
In terms of macronutrients first, pearl barley has about three times the carbs for only the same amount of protein and fiber—if it had been regular barley rather than pearl parley, it’d have about twice the fiber, but pearl barley has had the fibrous husk removed.
Vitamins really set the two part, though: oats have a lot more (60x more) vitamin A, and notably more of vitamins B1, B2, B3, B5, B6, and B9, as well as 6x more vitamin E. In contrast, pearl barley has a little more vitamin K and choline. An easy win for oats in this section.
In the category of minerals, oats have over 6x more calcium, 3x more iron, and a little more magnesium, manganese, and phosphorus. Meanwhile, pearl barley boats a little more copper, potassium, selenium, and zinc. So, a more moderate win for oats in this category.
They are both very good for the gut, unless you have a gluten intolerance/allergy, in which case, oats are the only answer here since pearl barley, as per barley in general, has gluten as its main protein (oats, meanwhile, do not contain gluten, unless by cross-contamination).
Adding up all the sections, this one’s a clear win for oats.
Want to learn more?
You might like to read:
- Eat More (Of This) For Lower Blood Pressure
- Making Friends With Your Gut (You Can Thank Us Later)
- Gluten: What’s The Truth?
Take care!
Share This Post
-
For Seniors With Hoarding Disorder, a Support Group Helps Confront Stigma and Isolation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A dozen people seated around folding tables clap heartily for a beaming woman: She’s donated two 13-gallon garbage bags full of clothes, including several Christmas sweaters and a couple of pantsuits, to a Presbyterian church.
A closet cleanout might not seem a significant accomplishment. But as the people in this Sunday-night class can attest, getting rid of stuff is agonizing for those with hoarding disorder.
People with the diagnosis accumulate an excessive volume of things such as household goods, craft supplies, even pets. In extreme cases, their homes become so crammed that moving between rooms is possible only via narrow pathways.
These unsafe conditions can also lead to strained relationships.
“I’ve had a few relatives and friends that have condemned me, and it doesn’t help,” said Bernadette, a Pennsylvania woman in her early 70s who has struggled with hoarding since retiring and no longer allows guests in her home.
People who hoard are often stigmatized as lazy or dirty. NPR, Spotlight PA, and KFF Health News agreed to use only the first names of people with hoarding disorder interviewed for this article because they fear personal and professional repercussions if their condition is made public.
As baby boomers age into the group most affected by hoarding disorder, the psychiatric condition is a growing public health concern. Effective treatments are scarce. And because hoarding can require expensive interventions that drain municipal resources, more funding and expertise is needed to support those with the diagnosis before the issue grows into a crisis.
For Bernadette, the 16-week course is helping her turn over a new leaf.
The program doubles as a support group and is provided through Fight the Blight. The Westmoreland County, Pennsylvania, organization started offering the course at a local Masonic temple after founder Matt Williams realized the area lacked hoarding-specific mental health services.
Fight the Blight uses a curriculum based on cognitive behavioral therapy to help participants build awareness of what fuels their hoarding. People learn to be more thoughtful about what they purchase and save, and they create strategies so that decluttering doesn’t become overwhelming.
Perhaps more importantly, attendees say they’ve formed a community knitted together through the shared experience of a psychiatric illness that comes with high rates of social isolation and depression.
“You get friendship,” said Sanford, a classmate of Bernadette’s.
After a lifetime of judgment, these friendships have become an integral part of the changes that might help participants eventually clear out the clutter.
Clutter Catches Up to Baby Boomers
Studies have estimated that hoarding disorder affects around 2.5% of the general population — a higher rate than schizophrenia.
The mental illness was previously considered a subtype of obsessive-compulsive disorder, but in 2013 it was given its own diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, the DSM-5.
The biological and environmental factors that may drive hoarding are not well understood. Symptoms usually appear during the teenage years and tend to be more severe among older adults with the disorder. That’s partly because they have had more time to acquire things, said Kiara Timpano, a University of Miami psychology professor.
“All of a sudden you have to downsize this huge home with all the stuff and so it puts pressures on individuals,” she said. In Bernadette’s case, her clutter includes a collection of VHS tapes, and spices in her kitchen that she said date back to the Clinton administration.
But it’s more than just having decades to stockpile possessions; the urge to accumulate strengthens with age, according to Catherine Ayers, a psychiatry professor at the University of California-San Diego.
Researchers are working to discern why. Ayers and Timpano theorize that age-related cognitive changes — particularly in the frontal lobe, which regulates impulsivity and problem-solving — might exacerbate the disorder.
“It is the only mental health disorder, besides dementia, that increases in prevalence and severity with age,” Ayers said.
As the U.S. population ages, hoarding presents a growing public health concern: Some 1 in 5 U.S. residents are baby boomers, all of whom will be 65 or older by 2030.
This population shift will require the federal government to address hoarding disorder, among other age-related issues that it has not previously prioritized, according to a July report by the Democratic staff of the U.S. Senate Special Committee on Aging, chaired then by former Sen. Bob Casey (D-Pa.).
Health Hazards of Hoarding
Clutter creates physical risks. A cramped and disorderly home is especially dangerous for older adults because the risk of falling and breaking a bone increases with age. And having too many things in one space can be a fire hazard.
Last year, the National Fallen Firefighters Foundation wrote to the Senate committee’s leadership that “hoarding conditions are among the most dangerous conditions the fire service can encounter.” The group also said that cluttered homes delay emergency care and increase the likelihood of a first responder being injured on a call.
The Bucks County Board of Commissioners in Pennsylvania told Casey that hoarding-related mold and insects can spread to adjacent households, endangering the health of neighbors.
Due to these safety concerns, it might be tempting for a family member or public health agency to quickly empty someone’s home in one fell swoop.
That can backfire, Timpano said, as it fails to address people’s underlying issues and can be traumatic.
“It can really disrupt the trust and make it even less likely that the individual is willing to seek help in the future,” she said.
It’s more effective, Timpano said, to help people build internal motivation to change and help them identify goals to manage their hoarding.
For example, at the Fight the Blight class, a woman named Diane told the group she wanted a cleaner home so she could invite people over and not feel embarrassed.
Sanford said he is learning to keep his documents and record collection more organized.
Bernadette wants to declutter her bedroom so she can start sleeping in it again. Also, she’s glad she cleared enough space on the first floor for her cat to play.
“Because now he’s got all this room,” she said, “he goes after his tail like a crazy person.”
Ultimately, the home of someone with hoarding disorder might always be a bit cluttered, and that’s OK. The goal of treatment is to make the space healthy and safe, Timpano said, not to earn Marie Kondo’s approval.
Lack of Treatment Leaves Few Options
A 2020 study found that hoarding correlates with homelessness, and those with the disorder are more likely to be evicted.
Housing advocates argue that under the Fair Housing Act, tenants with the diagnosis are entitled to reasonable accommodation. This might include allowing someone time to declutter a home and seek therapy before forcing them to leave their home.
But as outlined in the Senate aging committee’s report, a lack of resources limits efforts to carry out these accommodations.
Hoarding is difficult to treat. In a 2018 study led by Ayers, the UCSD psychiatrist, researchers found that people coping with hoarding need to be highly motivated and often require substantial support to remain engaged with their therapy.
The challenge of sticking with a treatment plan is exacerbated by a shortage of clinicians with necessary expertise, said Janet Spinelli, the co-chair of Rhode Island’s hoarding task force.
Could Changes to Federal Policy Help?
Casey, the former Pennsylvania senator, advocated for more education and technical assistance for hoarding disorder.
In September, he called for the Substance Abuse and Mental Health Services Administration to develop training, assistance, and guidance for communities and clinicians. He also said the Centers for Medicare & Medicaid Services should explore ways to cover evidence-based treatments and services for hoarding.
This might include increased Medicare funding for mobile crisis services to go to people’s homes, which is one way to connect someone to therapy, Spinelli said.
Another strategy would involve allowing Medicaid and Medicare to reimburse community health workers who assist patients with light cleaning and organizing; research has found that many who hoard struggle with categorization tasks.
Williams, of Fight the Blight, agrees that in addition to more mental health support, taxpayer-funded services are needed to help people address their clutter.
When someone in the group reaches a point of wanting to declutter their home, Fight the Blight helps them start the process of cleaning, removing, and organizing.
The service is free to those earning less than 150% of the federal poverty level. People making above that threshold can pay for assistance on a sliding scale; the cost varies also depending on the size of a property and severity of the hoarding.
Also, Spinelli thinks Medicaid and Medicare should fund more peer-support specialists for hoarding disorder. These mental health workers draw on their own life experiences to help people with similar diagnoses. For example, peer counselors could lead classes like Fight the Blight’s.
Bernadette and Sanford say courses like the one they enrolled in should be available all over the U.S.
To those just starting to address their own hoarding, Sanford advises patience and persistence.
“Even if it’s a little job here, a little job there,” he said, “that all adds up.”
This article is from a partnership that includes Spotlight PA, NPR, and KFF Health News.
Spotlight PA is an independent, nonpartisan, and nonprofit newsroom producing investigative and public-service journalism that holds power to account and drives positive change in Pennsylvania. Sign up for its free newsletters.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
Related Posts
-
Should You Soak Your Nuts?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝hi. how many almonds should one eat per day? do they need to be soaked? thank you.❞
Within reason, however many you like! Given that protein is an appetite suppressant, you’ll probably find it’s not too many.
Dr. Michael Greger, of “How Not To Die” fame, suggests aiming for 30g of nuts per day. Since almonds typically weigh about 1g each, that means 30 if it’s all almonds.
And if you’re wondering about 10 almonds? The name’s a deliberate reference to an old internet hoax about 10 almonds being the equivalent of an aspirin for treating a headache. It’s a reminder to be open-mindedly skeptical about information circulating wildly, and look into the real, evidence-based, science of things.
- Sometimes, the science validates claims, and we’re excited to share that!
- Sometimes, the science just shoots claims down, and it’s important to acknowledge when that happens too.
On which note, about soaking…
Short version: soaking can improve the absorption of some nutrients, but not much more than simply chewing thoroughly. See:
- A review of the impact of processing on nutrient bioaccessibility and digestion of almonds
- Mastication of almonds: effects of lipid bioaccessibility, appetite, and hormone response
Soaking does reduce certain “antinutrients” (compounds that block absorption of other nutrients), such as phytic acid. However, even a 24-hour soak reduces them only by about 5%:
If you don’t want to take 24-hours to get a 5% benefit, there’s good news! A 12-hour soak can result in 4% less phytic acid in chopped (but not whole) almonds:
The Effect of Soaking Almonds and Hazelnuts on Phytate and Mineral Concentrations
Lest that potentially underwhelming benefit leave a bitter taste in your mouth, one good thing about soaking almonds (if you don’t like bitter tastes, anyway) is that it will reduce their bitterness:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Five Flavors & Five Benefits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Five Flavors Of Good Health
Schisandra chinensis, henceforth Schisandra, is also called the “five flavor fruit”, for covering the culinary bases of sweet, salt, bitter, sour, and pungent.
It can be eaten as a fruit (small red berries), juiced from the fruit, or otherwise extracted into supplements (dried powder of the fruit being a common one).
It has long enjoyed usage in various traditional medicines, especially in China and Siberia.
So, what are its health claims, and how does the science stack up?
Menopause
Most of the studies are mouse studies, and we prefer studies on humans, so here’s a small (n=36) randomized clinical trial that concluded…
❝Schisandra chinensis can be a safe and effective complementary medicine for menopausal symptoms, especially for hot flushes, sweating, and heart palpitations❞
~ Dr. Joon Young Park & Dr. Kye Hyun Kim
Read more: A randomized, double-blind, placebo-controlled trial of Schisandra chinensis for menopausal symptoms
Antioxidant (and perhaps more)
Like many berries, it’s a good source of lignans offering antioxidant effects:
Antioxidant Effects of Schisandra chinensis Fruits and Their Active Constituents
Lignans usually have anticancer effects too (which is reasonably, given what is antioxidant is usually anticancer and anti-inflammatory as well, by the same mechanism) but those have not yet been studied in schisandra specifically.
Antihepatotoxicity
In other words, it’s good for your liver. At least, so animal studies tell us, because human studies haven’t been done yet for this one. The effect is largely due to its antioxidant properties, but it seems especially effective for the liver—which is not surprising, giving the liver’s regeneration mechanism.
Anyway, here’s a fascinating study that didn’t even need to use the fruit itself, just the pollen from the plant, it was that potent:
Athletics enhancer
While it’s not yet filling the shelves of sports nutrition stores, we found a small (n=45) study with healthy post-menopausal women who took either 1g of schisandra (experimental group) or 1g of starch (placebo group), measured quadriceps muscle strength and resting lactate levels over the course of a 12 week intervention period, and found:
❝Supplementation of Schisandra chinensis extract can help to improve quadriceps muscle strength as well as decrease lactate level at rest in adult women ❞
Anti-Alzheimers & Anti-Parkinsons
The studies for this are all in vitro, but that’s because it’s hard to find volunteers willing to have their brains sliced and looked at under a microscope while they’re still alive.
Nevertheless, the results are compelling, and it seems uncontroversial to say that schisandra, or specifically Schisandrin B, a compound it contains, has not only anti-inflammatory properties, but also neuroprotective properties, and specifically blocks the formation of excess amyloid-β peptides in the brain (which are critical for the formation of amyloid plaque, as found in the brains of Alzheimer’s patients):
Is it safe?
For most people, yes! Some caveats:
- As it can stimulate the uterus, it’s not recommended if you’re pregant.
- Taking more than the recommended amount can worsen symptoms of heartburn, GERD, ulcers, or other illnesses like that.
And as ever, do speak with our own doctor/pharmacist if unsure, as your circumstances may vary and we cannot cover all possibilities here.
Where can I get some?
We don’t sell it, but here for your convenience is an example product on Amazon
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
People on Ozempic may have fewer heart attacks, strokes and addictions – but more nausea, vomiting and stomach pain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
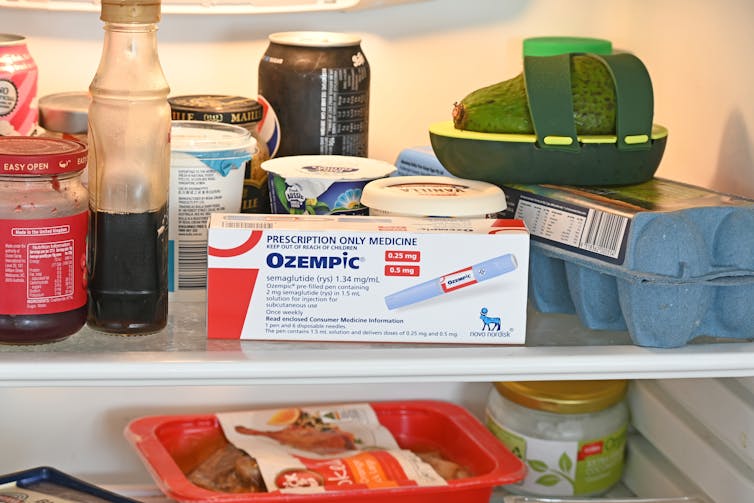
Ozempic and Wegovy are increasingly available in Australia and worldwide to treat type 2 diabetes and obesity.
The dramatic effects of these drugs, known as GLP-1s, on weight loss have sparked huge public interest in this new treatment option.
However, the risks and benefits are still being actively studied.
In a new study in Nature Medicine, researchers from the United States reviewed health data from about 2.4 million people who have type 2 diabetes, including around 216,000 people who used a GLP-1 drug, between 2017 and 2023.
The researchers compared a range of health outcomes when GLP-1s were added to a person’s treatment plan, versus managing their diabetes in other ways, often using glucose-lowering medications.
Overall, they found people who used GLP-1s were less likely to experience 42 health conditions or adverse health events – but more likely to face 19 others.
myskin/Shutterstock What conditions were less common?
Cardiometabolic conditions
GLP-1 use was associated with fewer serious cardiovascular and coagulation disorders. This includes deep vein thrombosis, pulmonary embolism, stroke, cardiac arrest, heart failure and myocardial infarction.
Neurological and psychiatric conditions
GLP-1 use was associated with fewer reported substance use disorders or addictions, psychotic disorders and seizures.
Infectious conditions
GLP-1 use was associated with fewer bacterial infections and pneumonia.
What conditions were more common?
Gastrointestinal conditions
Consistent with prior studies, GLP-1 use was associated with gastrointestinal conditions such as nausea, vomiting, gastritis, diverticulitis and abdominal pain.
Other adverse effects
Increased risks were seen for conditions such as low blood pressure, syncope (fainting) and arthritis.
People who took Ozempic were more likely to experience stomach upsets than those who used other type 2 diabetes treatments. Douglas Cliff/Shutterstock How robust is this study?
The study used a large and reputable dataset from the US Department of Veterans Affairs. It’s an observational study, meaning the researchers tracked health outcomes over time without changing anyone’s treatment plan.
A strength of the study is it captures data from more than 2.4 million people across more than six years. This is much longer than what is typically feasible in an intervention study.
Observational studies like this are also thought to be more reflective of the “real world”, because participants aren’t asked to follow instructions to change their behaviour in unnatural or forced ways, as they are in intervention studies.
However, this study cannot say for sure that GLP-1 use was the cause of the change in risk of different health outcomes. Such conclusions can only be confidently made from tightly controlled intervention studies, where researchers actively change or control the treatment or behaviour.
The authors note the data used in this study comes from predominantly older, white men so the findings may not apply to other groups.
Also, the large number of participants means that even very small effects can be detected, but they might not actually make a real difference in overall population health.
Observational studies track outcomes over time, but can’t say what caused the changes. Jacob Lund/Shutterstock Other possible reasons for these links
Beyond the effect of GLP-1 in the body, other factors may explain some of the findings in this study. For example, it’s possible that:
- people who used GLP-1 could be more informed about treatment options and more motivated to manage their own health
- people who used GLP-1 may have received it because their health-care team were motivated to offer the latest treatment options, which could lead to better care in other areas that impact the risk of various health outcomes
- people who used GLP-1 may have been able to do so because they lived in metropolitan centres and could afford the medication, as well as other health-promoting services and products, such as gyms, mental health care, or healthy food delivery services.
Did the authors have any conflicts of interest?
Two of the study’s authors declared they were “uncompensated consultants” for Pfizer, a global pharmaceutical company known for developing a wide range of medicines and vaccines. While Pfizer does not currently make readily available GLP-1s such as Ozempic or Wegovy, they are attempting to develop their own GLP-1s, so may benefit from greater demand for these drugs.
This research was funded by the US Department of Veterans Affairs, a government agency that provides a wide range of services to military veterans.
No other competing interests were reported.
Diabetes vs weight-loss treatments
Overall, this study shows people with type 2 diabetes using GLP-1 medication generally have more positive health outcomes than negative health outcomes.
However, the study didn’t include people without type 2 diabetes. More research is needed to understand the effects of these medications in people without diabetes who are using them for other reasons, including weight loss.
While the findings highlight the therapeutic benefits of GLP-1 medications, they also raise important questions about how to manage the potential risks for those who choose to use this medication.
The findings of this study can help many people, including:
- policymakers looking at ways to make GLP-1 medications more widely available for people with various health conditions
- health professionals who have regular discussions with patients considering GLP-1 use
- individuals considering whether a GLP-1 medication is right for them.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Accredited Practising Dietitian and Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: