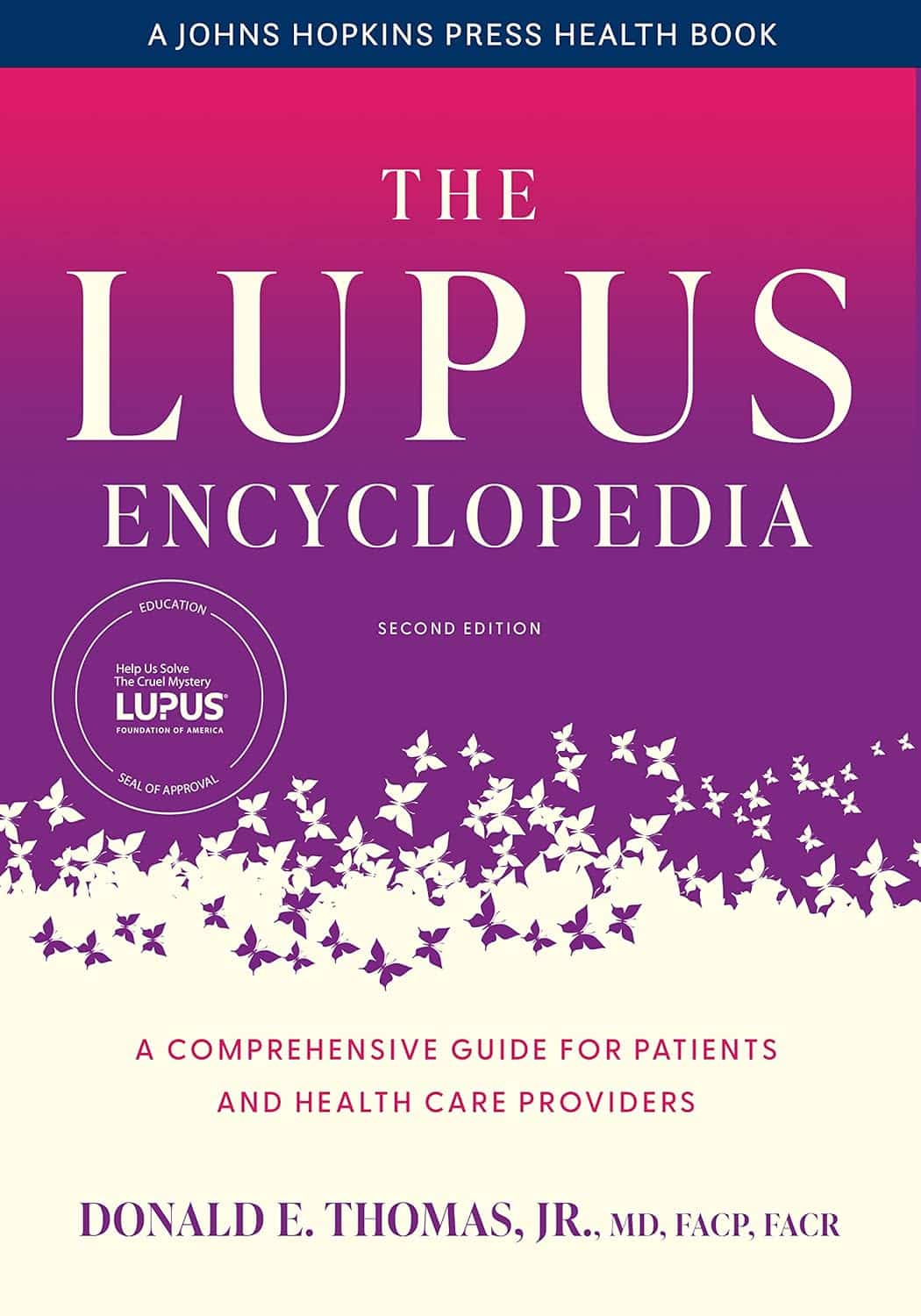
The Lupus Encyclopedia – by Dr. Donald Thomas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a note on the authorship: while this is broadly by Donald E. Thomas Jr. MD FACP FACR, there were more contributors, namely:
Jemima Albayda, MD; Divya Angra, MD; Alan N. Baer, MD; Sasha Bernatsky, MD, PhD; George Bertsias, MD, PhD; Ashira D. Blazer, MD; Ian Bruce, MD; Jill Buyon, MD; Yashaar Chaichian, MD; Maria Chou, MD; Sharon Christie, Esq; Angelique N. Collamer, MD; Ashté Collins, MD; Caitlin O. Cruz, MD; Mark M. Cruz, MD; Dana DiRenzo, MD; Jess D. Edison, MD; Titilola Falasinnu, PhD; Andrea Fava, MD; Cheri Frey, MD; Neda F. Gould, PhD; Nishant Gupta, MD; Sarthak Gupta, MD; Sarfaraz Hasni, MD; David Hunt, MD; Mariana J. Kaplan, MD; Alfred Kim, MD; Deborah Lyu Kim, DO; Rukmini Konatalapalli, MD; Fotios Koumpouras, MD; Vasileios C. Kyttaris, MD; Jerik Leung, MPH; Hector A. Medina, MD; Timothy Niewold, MD; Julie Nusbaum, MD; Ginette Okoye, MD; Sarah L. Patterson, MD; Ziv Paz, MD; Darryn Potosky, MD; Rachel C. Robbins, MD; Neha S. Shah, MD; Matthew A. Sherman, MD; Yevgeniy Sheyn, MD; Julia F. Simard, ScD; Jonathan Solomon, MD; Rodger Stitt, MD; George Stojan, MD; Sangeeta Sule, MD; Barbara Taylor, CPPM, CRHC; George Tsokos, MD; Ian Ward, MD; Emma Weeding, MD; Arthur Weinstein, MD; Sean A. Whelton, MD
The reason we mention this is to render it clear that this isn’t one man’s opinions (as happens with many books about certain topics), but rather, a panel of that many doctors all agreeing that this is correct and good, evidence-based, up-to-date (as of the publication of this latest revised edition last year) information.
And if you have lupus, you’ll be aware there are a lot of doctors who don’t know a tremendous amount about it, hence the value of this “…for patients and healthcare providers” tome.
It is what it claims to be: a very comprehensive guide. It’s not light reading, and it is 848 pages of information-dense text and diagrams. If you want to know something, anything, about lupus, then if science knows it, then chances are it is in this book, or this book will at least point you directly to a paper you can read about your specific query.
The style is, nevertheless, about as readable for the layperson as possible, which is quite an achievement for a book with this amount of dense scientific information. For that, the author thanks his husband, for being the non-doctor beta-reader to screen it for readability—quite a service, with all those doctors writing!
Bottom line: if you or someone you love has lupus, this book should absolutely be in your collection.
Click here to check out The Lupus Encyclopedia, and have everything at your fingertips!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Peas vs Green Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peas to green beans, we picked the peas.
Why?
Looking at macros first, peas have nearly 6x the protein, nearly 2x the fiber, and nearly 2x the carbs, making them the “more food per food” choice.
In terms of vitamins, peas have more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, and choline, while green beans have more of vitamins E and K. An easy win for peas.
In the category of minerals, peas have more copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while green beans have more calcium. Another overwhelming win for peas.
In short, enjoy both (diversity is good), but there’s a clear winner here and it’s peas.
Want to learn more?
You might like to read:
Peas vs Broad Beans – Which is Healthier?
Take care!
Share This Post
-
10 Simple Japanese Habits For Healthier & Longer Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You don’t have to be Japanese or live in Okinawa to enjoy the benefits of healthy longevity. A lot of it comes down to simple habits:
Easy to implement
We’ll not keep the 10 habits a mystery; they are:
- Start the day with hot water: drinking hot water in the morning helps with hydration, warming the body, and aiding digestion.
- Enjoy a hearty breakfast: Japanese breakfasts are traditionally filling, nutritious, and help promote energy and longevity. Typical components include rice, miso soup, fish, and pickles.
- Take balanced meals: Japanese education emphasizes nutrition from a young age, promoting balanced meals with proteins, fiber, and vitamins & minerals.
- Enjoy fermented foods: fermented foods, such as nattō and soy-based condiments, support digestion, heart health, and the immune system.
- Drink green tea and matcha: both are rich in health benefits; preparing matcha mindfully adds a peaceful ritual to daily life too.
- Keep the “80% full” rule: “hara hachi bu” encourages eating until 80% full, which can improve longevity and, of course, prevent overeating.
- Use multiple small dishes: small servings and a variety of dishes help prevent overeating and ensure a diverse intake of nutrients.
- Gratitude before and after meals: saying “itadakimasu” and “gochisousama” promotes mindful eating, and afterwards, good digestion. Speaking Japanese is of course not the key factor here, but rather, do give yourself a moment of reflection before and after meals.
- Use vinegar in cooking: vinegar, often used in sushi rice and sauces like ponzu, adds flavor and offers health benefits, mostly pertaining to blood sugar balance.
- Eat slowly: Eating at a slower pace will improve digestion, and can enhance satiety and prevent accidentally overeating.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Get More Out Of What’s On Your Plate
Take care!
Share This Post
-
It’s OK That You’re Not OK – by Megan Devine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Firstly, be aware: this is not a cheerful book. If you’re looking for something to life your mood after a loss, it will not be this.
What, then, will you find? A reminder that grief is also the final translation of love, and not necessarily something to be put aside as quickly as possible—or even ever, if we don’t want to.
Too often, society (and even therapists) will correctly note that no two instances of grief are the same (after all, no two people are, so definitely no two relationships are, so how could two instances of grief be?), but will still expect that if most people can move on quickly from most losses, that you should too, and that if you don’t then there is something pathological at hand that needs fixing.
Part one of the book covers this (and more) in a lot of detail; critics have called it a diatribe against the current status quo in the field of grief.
Part two of the book is about “what to do with your grief”, and addresses the reality of grief, how (and why) to stay alive when not doing so feels like a compelling option, dealing with grief’s physical side effects, and calming your mind in ways that actually work (without trying to sweep your grief under a rug).
Parts three and four are more about community—how to navigate the likely unhelpful efforts a lot of people may make in the early days, and when it comes to those people who can and will actually be a support, how to help them to help you.
In the category of criticism, she also plugs her own (paid, subscription-based) online community, which feels a little mercenary, especially as while community definitely can indeed help, the prospect of being promptly exiled from it if you stop paying, doesn’t.
Bottom line: if you have experienced grief and felt like moving on was the right thing to do, then this book isn’t the one for you. If, on the other hand, your grief feels more like something you will carry just as you carry the love you feel for them, then you’ll find a lot about that here.
Share This Post
Related Posts
-
How To Escape From A Despairing Mood
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When we are in a despairing mood, that’s when it can feel hardest to actually implement anything we know about getting out of one. That’s why sometimes, the simplest solutions are the best:
Imagination Is Key
Despairing moods occur when it’s hard to envision a better life. Imagination is the power to envision alternatives, such as new jobs, relationships, or lifestyle, but sadness can cloud our ability to imagine solutions like changing careers, moving house, or starting fresh. With enough imagination, most problems can be worked around—and new opportunities can always be found.
Importantly: we are not bound by our past or present circumstances; we have the freedom and flexibility to choose new paths. That doesn’t mean it’ll always be a walk in the park, but “this too shall pass”.
You may be thinking: “sometimes the hardship does pass, but can last many years”, and that is true. All the more reason to check if there’s a freer lane you can slip into to speed ahead. Even if there isn’t, the mere act of imagining such lanes is already respite from the hardships—and having envisioned such will make it much easier for you to recognise when opportunities for change do come along.
To foster imagination, we are advised to expose ourselves to different narratives, preparing ourselves for alternative ways of living. Thus, we can reframe life’s challenges as intellectual puzzles, urging us to rebuild creatively and find new solutions!
For more on all this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Behavioral Activation Against Depression & Anxiety
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Managing Your Mortality
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Planning Is a Matter of Life and Death
Barring medical marvels as yet unrevealed, we are all going to die. We try to keep ourselves and our loved ones in good health, but it’s important to be prepared for the eventuality of death.
While this is not a cheerful topic, considering these things in advance can help us manage a very difficult thing, when the time comes.
We’ve put this under “Psychology Sunday” as it pertains to processing our own mortality, and managing our own experiences and the subsequent grief that our death may invoke in our loved ones.
We’ll also be looking at some of the medical considerations around end-of-life care, though.
Organizational considerations
It’s generally considered good to make preparations in advance. Write (or update) a Will, tie up any loose ends, decide on funerary preferences, perhaps even make arrangements with pre-funding. Life insurance, something difficult to get at a good rate towards the likely end of one’s life, is better sorted out sooner rather than later, too.
Beyond bureaucracy
What’s important to you, to have done before you die? It could be a bucket list, or it could just be to finish writing that book. It could be to heal a family rift, or to tell someone how you feel.
It could be more general, less concrete: perhaps to spend more time with your family, or to engage more with a spiritual practice that’s important to you.
Perhaps you want to do what you can to offset the grief of those you’ll leave behind; to make sure there are happy memories, or to make any requests of how they might remember you.
Lest this latter seem selfish: after a loved one dies, those who are left behind are often given to wonder: what would they have wanted? If you tell them now, they’ll know, and can be comforted and reassured by that.
This could range from “bright colors at my funeral, please” to “you have my blessing to remarry if you want to” to “I will now tell you the secret recipe for my famous bouillabaisse, for you to pass down in turn”.
End-of-life care
Increasingly few people die at home.
- Sometimes it will be a matter of fighting tooth-and-nail to beat a said-to-be-terminal illness, and thus expiring in hospital after a long battle.
- Sometimes it will be a matter of gradually winding down in a nursing home, receiving medical support to the end.
- Sometimes, on the other hand, people will prefer to return home, and do so.
Whatever your preferences, planning for them in advance is sensible—especially as money may be a factor later.
Not to go too much back to bureaucracy, but you might also want to consider a Living Will, to be enacted in the case that cognitive decline means you cannot advocate for yourself later.
Laws vary from place to place, so you’ll want to discuss this with a lawyer, but to give an idea of the kinds of things to consider:
National Institute on Aging: Preparing A Living Will
Palliative care
Palliative care is a subcategory of end-of-life care, and is what occurs when no further attempts are made to extend life, and instead, the only remaining goal is to reduce suffering.
In the case of some diseases including cancer, this may mean coming off treatments that have unpleasant side-effects, and retaining—or commencing—pain-relief treatments that may, as a side-effect, shorten life.
Euthanasia
Legality of euthanasia varies from place to place, and in some times and places, palliative care itself has been considered a form of “passive euthanasia”, that is to say, not taking an active step to end life, but abstaining from a treatment that prolongs it.
Clearer forms of passive euthanasia include stopping taking a medication without which one categorically will die, or turning off a life support machine.
Active euthanasia, taking a positive action to end life, is legal in some places and the means varies, but an overdose of barbiturates is an example; one goes to sleep and does not wake up.
It’s not the only method, though; options include benzodiazepines, and opioids, amongst others:
Efficacy and safety of drugs used for assisted dying
Unspoken euthanasia
An important thing to be aware of (whatever your views on euthanasia) is the principle of double-effect… And how it comes to play in palliative care more often than most people think.
Say a person is dying of cancer. They opt for palliative care; they desist in any further cancer treatments, and take medication for the pain. Morphine is common. Morphine also shortens life.
It’s common for such a patient to have a degree of control over their own medication, however, after a certain point, they will no longer be in sufficient condition to do so.
After this point, it is very common for caregivers (be they medical professionals or family members) to give more morphine—for the purpose of reducing suffering, of course, not to kill them.
In practical terms, this often means that the patient will die quite promptly afterwards. This is one of the reasons why, after sometimes a long-drawn-out period of “this person is dying”, healthcare workers can be very accurate about “it’s going to be in the next couple of days”.
The take-away from this section is: if you would like for this to not happen to you or your loved one, you need to be aware of this practice in advance, because while it’s not the kind of thing that tends to make its way into written hospital/hospice policies, it is very widespread and normalized in the industry on a human level.
Further reading: Goods, causes and intentions: problems with applying the doctrine of double effect to palliative sedation
One last thing…
Planning around our own mortality is never a task that seems pressing, until it’s too late. We recommend doing it anyway, without putting it off, because we can never know what’s around the corner.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is alcohol good or bad for you? Yes.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This article originally appeared in Harvard Public Health magazine.
It’s hard to escape the message these days that every sip of wine, every swig of beer is bad for your health. The truth, however, is far more nuanced.
We have been researching the health effects of alcohol for a combined 60 years. Our work, and that of others, has shown that even modest alcohol consumption likely raises the risk for certain diseases, such as breast and esophageal cancer. And heavy drinking is unequivocally harmful to health. But after countless studies, the data do not justify sweeping statements about the effects of moderate alcohol consumption on human health.
Yet we continue to see reductive narratives, in the media and even in science journals, that alcohol in any amount is dangerous. Earlier this month, for instance, the media reported on a new study that found even small amounts of alcohol might be harmful. But the stories failed to give enough context or probe deeply enough to understand the study’s limitations—including that it cherry-picked subgroups of a larger study previously used by researchers, including one of us, who concluded that limited drinking in a recommended pattern correlated with lower mortality risk.
“We need more high-quality evidence to assess the health impacts of moderate alcohol consumption. And we need the media to treat the subject with the nuance it requires. Newer studies are not necessarily better than older research.”
Those who try to correct this simplistic view are disparaged as pawns of the industry, even when no financial conflicts of interest exist. Meanwhile, some authors of studies suggesting alcohol is unhealthy have received money from anti-alcohol organizations.
We believe it’s worth trying, again, to set the record straight. We need more high-quality evidence to assess the health impacts of moderate alcohol consumption. And we need the media to treat the subject with the nuance it requires. Newer studies are not necessarily better than older research.
It’s important to keep in mind that alcohol affects many body systems—not just the liver and the brain, as many people imagine. That means how alcohol affects health is not a single question but the sum of many individual questions: How does it affect the heart? The immune system? The gut? The bones?
As an example, a highly cited study of one million women in the United Kingdom found that moderate alcohol consumption—calculated as no more than one drink a day for a woman—increased overall cancer rates. That was an important finding. But the increase was driven nearly entirely by breast cancer. The same study showed that greater alcohol consumption was associated with lower rates of thyroid cancer, non-Hodgkin lymphoma, and renal cell carcinoma. That doesn’t mean drinking a lot of alcohol is good for you—but it does suggest that the science around alcohol and health is complex.
One major challenge in this field is the lack of large, long-term, high-quality studies. Moderate alcohol consumption has been studied in dozens of randomized controlled trials, but those trials have never tracked more than about 200 people for more than two years. Longer and larger experimental trials have been used to test full diets, like the Mediterranean diet, and are routinely conducted to test new pharmaceuticals (or new uses for existing medications), but they’ve never been done to analyze alcohol consumption.
Instead, much alcohol research is observational, meaning it follows large groups of drinkers and abstainers over time. But observational studies cannot prove cause-and-effect because moderate drinkers differ in many ways from non-drinkers and heavy drinkers—in diet, exercise, and smoking habits, for instance. Observational studies can still yield useful information, but they also require researchers to gather data about when and how the alcohol is consumed, since alcohol’s effect on health depends heavily on drinking patterns.
For example, in an analysis of over 300,000 drinkers in the U.K., one of us found that the same total amount of alcohol appeared to increase the chances of dying prematurely if consumed on fewer occasions during the week and outside of meals, but to decrease mortality if spaced out across the week and consumed with meals. Such nuance is rarely captured in broader conversations about alcohol research—or even in observational studies, as researchers don’t always ask about drinking patterns, focusing instead on total consumption. To get a clearer picture of the health effects of alcohol, researchers and journalists must be far more attuned to the nuances of this highly complex issue.
One way to improve our collective understanding of the issue is to look at both observational and experimental data together whenever possible. When the data from both types of studies point in the same direction, we can have more confidence in the conclusion. For example, randomized controlled trials show that alcohol consumption raises levels of sex steroid hormones in the blood. Observational trials suggest that alcohol consumption also raises the risk of specific subtypes of breast cancer that respond to these hormones. Together, that evidence is highly persuasive that alcohol increases the chances of breast cancer.
Similarly, in randomized trials, alcohol consumption lowers average blood sugar levels. In observational trials, it also appears to lower the risk of diabetes. Again, that evidence is persuasive in combination.
As these examples illustrate, drinking alcohol may raise the risk of some conditions but not others. What does that mean for individuals? Patients should work with their clinicians to understand their personal risks and make informed decisions about drinking.
Medicine and public health would benefit greatly if better data were available to offer more conclusive guidance about alcohol. But that would require a major investment. Large, long-term, gold-standard studies are expensive. To date, federal agencies like the National Institutes of Health have shown no interest in exclusively funding these studies on alcohol.
Alcohol manufacturers have previously expressed some willingness to finance the studies—similar to the way pharmaceutical companies finance most drug testing—but that has often led to criticism. This happened to us, even though external experts found our proposal scientifically sound. In 2018, the National Institutes of Health ended our trial to study the health effects of alcohol. The NIH found that officials at one of its institutes had solicited funding from alcohol manufacturers, violating federal policy.
It’s tempting to assume that because heavy alcohol consumption is very bad, lesser amounts must be at least a little bad. But the science isn’t there, in part because critics of the alcohol industry have deliberately engineered a state of ignorance. They have preemptively discredited any research, even indirectly, by the alcohol industry—even though medicine relies on industry financing to support the large, gold-standard studies that provide conclusive data about drugs and devices that hundreds of millions of Americans take or use daily.
Scientific evidence about drinking alcohol goes back nearly 100 years—and includes plenty of variability in alcohol’s health effects. In the 1980s and 1990s, for instance, alcohol in moderation, and especially red wine, was touted as healthful. Now the pendulum has swung so far in the opposite direction that contemporary narratives suggest every ounce of alcohol is dangerous. Until gold-standard experiments are performed, we won’t truly know. In the meantime, we must acknowledge the complexity of existing evidence—and take care not to reduce it to a single, misleading conclusion.
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: