The Gut-Healthiest Yogurt
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not only is this yogurt, so it’s winning from the start with its probiotic goodness, but also it’s full of several kinds of fiber, and gut-healthy polyphenols too. Plus, it’s delicious. The perfect breakfast, but don’t let us stop you from enjoying it at any time of day!
You will need
- 1 cup yogurt with minimal additives. Live Greek yogurt is a top-tier choice, and plant-based varieties are fine too (just watch out, again, for needless additives)
- 7 dried figs, roughly chopped
- 6 fresh figs, thinly sliced
- 5 oz chopped pitted dates
- 4 tbsp mixed seeds (pumpkin, sunflower, and chia are a great combination)
Method
(we suggest you read everything at least once before doing anything)
1) Soak the dried figs, the dates, and half the seeds in hot water for at least 5 minutes. Drain (be careful not to lose the chia seeds) and put in a blender with ¼ cup cold water.
2) Blend the ingredients from the last step into a purée (you can add a little more cold water if it needs it).
3) Mix this purée into the yogurt in a bowl, and add in the remaining seeds, mixing them in thoroughly.
4) Top with the sliced figs, and serve (or refrigerate, up to a few days, until needed).

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Making Friends With Your Gut (You Can Thank Us Later)
- Dates vs Figs – Which is Healthier?
- The Tiniest Seeds With The Most Value
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Which Plant Milk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Plant-based milks—what’s best?
You asked us to look at some popular plant milks and their health properties, and we said we’d do a main feature, so here it is!
We’ll also give a quick nod to environmental considerations at the end too (they might not be quite what you expect!). That said, as a health and productivity newsletter, we’ll be focusing on the health benefits.
While we can give a broad overview, please note that individual brands may vary, especially in two important ways:
- Pro: many (most?) brands of plant milks fortify their products with extra vitamins and minerals, especially vitamin D and calcium.
- Con: some brands also add sugar.
So, by all means use this guide to learn about the different plants’ properties, and/but still do check labels later.
Alternatively, consider making your own!
- Pros: no added sugar + cheaper
- Cons: no added vitamins and minerals + some equipment required
Almond milk
Almond milk is low in carbs and thus good for a carb-controlled diet. It’s also high in vitamin E and a collection of minerals.
Oat milk
Oats are one of the healthiest “staple foods” around, and while drinking oat milk doesn’t convey all the benefits, it does a lot. It also has one of the highest soluble fiber contents of any milk, which is good for reducing LDL (bad) cholesterol levels.
See for example: Consumption of oat milk for 5 weeks lowers serum cholesterol and LDL cholesterol in free-living men with moderate hypercholesterolemia
Coconut milk
Coconut has a higher fat content than most plant milks, but also contains medium-chain triglycerides (MCTs). These raise HDL (good) cholesterol levels.
Read the study: How well do plant based alternatives fare nutritionally compared to cow’s milk?
Hemp milk
Being made from hemp seeds that contain a lot of protein and healthy fats (including omega-3 and omega-6), hemp milk packs a nutritious punch. It’s carb-free. It’s also THC-free, in case you were wondering, which means no, it does not have psychoactive effects.
Pea milk
It’s very high in protein, and contains an array of vitamins and minerals. It’s not very popular yet, so there isn’t as much research about it. This 2021 study found that it had the nutritional profile the closest to cow’s milk (beating soy by a narrow margin) and praised it as a good alternative for those with a soy allergy.
This is Research Review Monday so we try to stick to pure science, but for your interest… here’s an interesting pop-science article (ostensibly in affiliation with the pea milk brand, Ripple) about the nutritional qualities of their pea milk specifically, which uses particularly nutrient-dense yellow peas, plus some extra vitamin and mineral fortifications:
Read: Ripple Milk: 6 Reasons Why You Should Try Pea Milk
Soy milk
Perhaps the most popular plant milk, and certainly usually the cheapest in stores. It’s high in protein, similar to cow’s milk. In fact, nutritionally, it’s one of the closest to cow’s milk without involving cows as a middleman. (Did you know three quarters of all soy in the world is grown to feed to livestock, not humans? Now you do).
And no, gentlemen-readers, it won’t have any feminizing effects. The human body can’t use the plant estrogens in soy for that. It does give some isoflavone benefits though, which are broadly good for everyone’s health. See for example this research review with 439 sources of its own:
Read: Soy and Health Update: Evaluation of the Clinical and Epidemiologic Literature
Quick note on flavor: nut milks have the flavor of the nut they were made from. Coconut milk tastes of coconut. The other milks listed above don’t have much of a flavor—which in many cases may be what you want.
Note on environmental considerations:
A lot of us try to be as socially responsible as reasonably possible in our choices, so this may be an influencing factor. In a nutshell:
- Oats and Soy are generally grown as vast monocrops, and these are bad for the environment
- They are still better for the environment than cow’s milk though, as for example most soy is grown to feed to cows, not humans. So including cows in the process means four times as much monocrop farming, plus adds several other environmental issues that are beyond the scope of this newsletter.
- Almonds are particularly resource-intensive when it comes to water use.
- Still nowhere near as much as cows, though.
- Peas are grown in places that naturally have very high rainfall, so are a good option here. Same generally goes for rice, which didn’t make the cut today. (Nor did hazelnuts, sorry—we can only include so much!)
- Hemp is by far and away the most environmentally friendly, assuming it is grown in a climate naturally conducive to such.
- Making plant milk at home is usually most environmentally friendly, depending on where your ingredients came from.
- Literally any plant milk is much more environmentally friendly than cow’s milk.
See the science for yourself: Reducing food’s environmental impacts through producers and consumers
See also (if you like graphs and charts): Environmental footprints of dairy and plant-based milks
Share This Post
-
Healthy Longevity As A Lifestyle Choice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
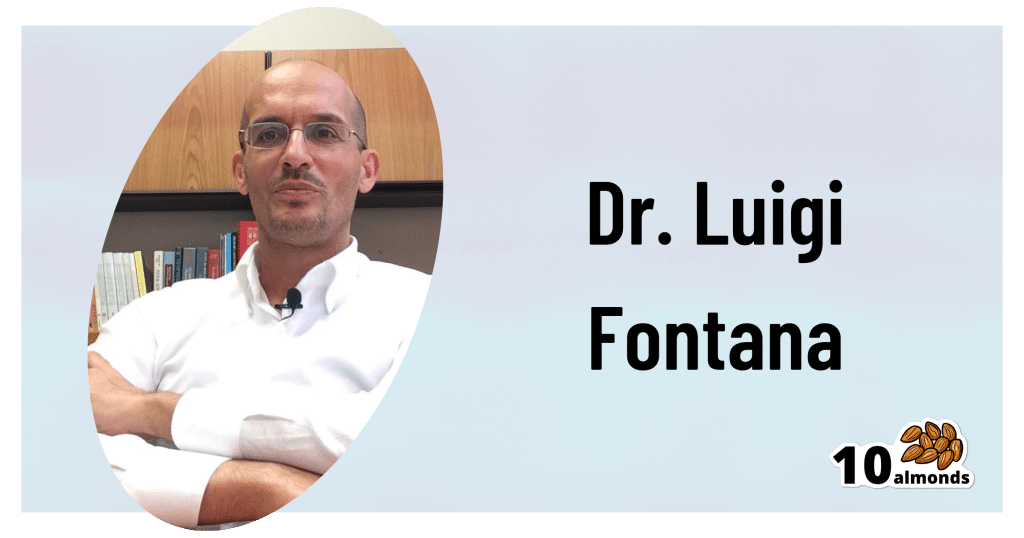
7 Keys To Healthy Longevity
This is Dr. Luigi Fontana. He’s a research professor of Geriatrics & Nutritional Science, and co-director of the Longevity Research Program at Washington University in St. Louis.
What does he want us to know?
He has a many-fold approach to healthy longevity, most of which may not be news to you, but you might want to prioritize some things:
Consider caloric restriction with optimal nutrition (CRON)
This is about reducing the metabolic load on your body, which frees up bodily resources for keeping yourself young.
Keeping your body young and healthy is your body’s favorite thing to do, but it can’t do that if it never gets a chance because of all the urgent metabolic tasks you’re giving it.
If CRON isn’t your thing (isn’t practicable for you, causes undue suffering, etc) then intermittent fasting is a great CR mimetic, and he recommends that too. See also:
- Is Cutting Calories The Key To Healthy Long Life?
- Fasting Without Crashing? We Sort The Science From The Hype
Keep your waistline small
Whichever approach you prefer to use to look after your metabolic health, keeping your waistline down is much more important for health than BMI.
Specifically, he recommends keeping it:
- under 31.5” for women
- under 37” for men
The disparity here is because of hormonal differences that influence both metabolism and fat distribution.
Exercise as part of your lifestyle
For Dr. Fontana, he loves mountain-biking (this writer could never!) and weight-lifting (also not my thing). But what’s key is not the specifics, but what’s going on:
- Some kind of frequent movement
- Some kind of high-intensity interval training
- Some kind of resistance training
Frequent movement because our bodies are evolved to be moving more often than not:
The Doctor Who Wants Us To Exercise Less, & Move More
High-Intensity Interval Training because unlike most forms of exercise (which slow metabolism afterwards to compensate), it boosts metabolism for up to 2 hours after training:
How To Do HIIT (Without Wrecking Your Body)
Resistance training because strength (of muscles and bones) matters too:
Resistance Is Useful! (Especially As We Get Older)
Writer’s examples:
So while I don’t care for mountain-biking or weight-lifting, what I do is:
1) movement: walk (briskly!) everywhere and also use a standing desk
2) HIIT: 2-minute bursts of hindu squats and/or exercise bike sprints
3) resistance: pilates and other calisthenicsModeration is not key
Dr. Fontana advises that we do not smoke, and that we do not drink alcohol, for example. He also notes that just as the only healthy amount of alcohol is zero, less ultra-processed food is always better than more.
Maybe you don’t want to abstain completely, but mindful wilful consumption of something unhealthy is preferable to believing “moderate consumption is good for the health” and an unhealthy habit develops!
Greens and beans
Shocking absolutely nobody, Dr. Fontana advocates for (what has been the most evidence-based gold standard of healthy-aging diets for quite some years now) the Mediterranean diet.
See also: Four Ways To Upgrade The Mediterranean Diet ← this is about tweaking the Mediterranean diet per personal area of focus, e.g. anti-inflammatory bonus, best for gut, heart healthiest, and most neuroprotective.
Take it easy
Dr. Fontana advises us (again, with a wealth of evidence) Mindfulness-Based Stress Reduction, and to get good sleep.
Not shocked?
To quote the good doctor,
❝There are no shortcuts. No magic pills or expensive procedures can replace the beneficial effects of a healthy diet, exercise, mindfulness, or a regenerating night’s sleep.❞
Always a good reminder!
Want to know more?
You might enjoy his book “The Path to Longevity: How to Reach 100 with the Health and Stamina of a 40-Year-Old”, which we reviewed previously
You might also like this video of his, about changing the conversation from “chronic disease” to “chronic health”:
Want to watch it, but not right now? Bookmark it for later
Take care!
Share This Post
-
Wakefulness, Cognitive Enhancement, AND Improved Mood?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Old Drug, New Tricks?
Modafinil (also known by brand names including Modalert and Provigil) is a dopamine uptake inhibitor.
What does that mean? It means it won’t put any extra dopamine in your brain, but it will slow down the rate at which your brain removes naturally-occuring dopamine.
The result is that your brain will get to make more use of the dopamine it does have.
(dopamine is a neutrotransmitter that allows you to feel wakeful and happy, and perform complex cognitive tasks)
Modafinil is prescribed for treatment of excessive daytime sleepiness. Often that’s caused by shift work sleep disorder, sleep apnea, restless leg syndrome, or narcolepsy.
Read: Overview of the Clinical Uses, Pharmacology, and Safety of Modafinil
Many studies done on humans (rather than rats) have been military experiments to reduce the effects of sleep deprivation:
Click Here To See A Military Study On Modafinil!
They’ve found modafinil to be helpful, and more effective and more long-lasting than caffeine, without the same “crash” later. This is for two reasons:
1) while caffeine works by blocking adenosine (so you don’t feel how tired you are) and by constricting blood vessels (so you feel more ready-for-action), modafinil works by allowing your brain to accumulate more dopamine (so you’re genuinely more wakeful, and you get to keep the dopamine)
2) the biological half-life of modafinil is 12–15 hours, as opposed to 4–8 hours* for caffeine.
*Note: a lot of sources quote 5–6 hours for caffeine, but this average is misleading. In reality, we are each genetically predetermined to be either a fast caffeine metabolizer (nearer 4 hours) or a slow caffeine metabolizer (nearer 8 hours).
What’s a biological half-life (also called: elimination half-life)?
A substance’s biological half-life is the time it takes for the amount in the body to be reduced by exactly half.
For example: Let’s say you’re a fast caffeine metabolizer and you have a double-espresso (containing 100mg caffeine) at 8am.
By midday, you’ll have 50mg of caffeine left in your body. So far, so simple.
By 4pm you might expect it to be gone, but instead you have 25mg remaining (because the amount halves every four hours).
By 8pm, you have 12.5mg remaining.
When midnight comes and you’re tucking yourself into bed, you still have 6.25mg of caffeine remaining from your morning coffee!
Use as a nootropic
Many healthy people who are not sleep-deprived use modafinil “off-label” as a nootropic (i.e., a cognitive enhancer).
Read: Modafinil for cognitive neuroenhancement in healthy non-sleep-deprived subjects: A systematic review
Important Note: modafinil is prescription-controlled, and only FDA-approved for sleep disorders.
To get around this, a lot of perfectly healthy biohackers describe the symptoms of sleep pattern disorder to their doctor, to get a prescription.
We do not recommend lying to your healthcare provider, and nor do we recommend turning to the online “grey market”.
Such websites often use anonymized private doctors to prescribe on an “informed consent” basis, rather than making a full examination. Those websites then dispense the prescribed medicines directly to the patient with no further questions asked (i.e. very questionable practices).
Caveat emptor!
A new mood-brightener?
Modafinil was recently tested head-to-head against Citalapram for the treatment of depression, and scored well:
See its head-to-head scores here!
How does it work? Modafinil does for dopamine what a lot of anti-depressants do for serotonin. Both dopamine and serotonin promote happiness and wakefulness.
This is very promising, especially as modafinil (in most people, at least) has fewer unwanted side-effects than a lot of common anti-depressant medications.
Share This Post
Related Posts
-
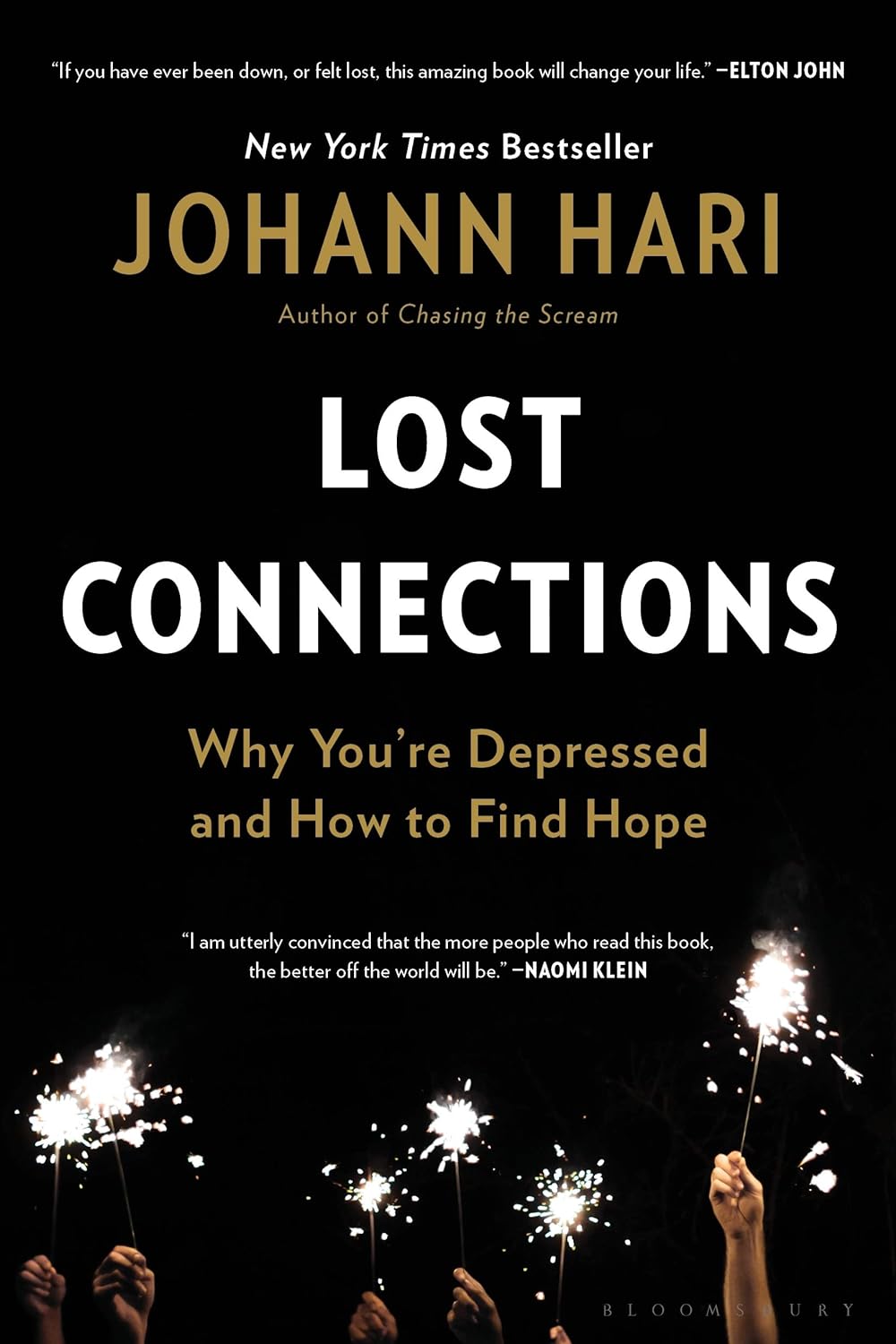
Lost Connections – by Johann Hari
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Johann Hari had a long journey through (and out of!) depression, and shares his personal findings, including his disappointment with medical options, and a focus on the external factors that lead to depression.
And that’s key to this book—while he acknowledges later in the book that there are physiological factors involved in depression, he wants to look past things we can’t change (like genes accounting for 37% of depression) or things that there may be unwanted side-effects to changing (as in the case of antidepressants, for many people), to things we genuinely can choose.
And no, it’s not a “think yourself happy” book either; rather, it looks at nine key external factorsthat a) influence depression b) can mostly be changed.
If the book has a downside, it’s that the author does tend to extrapolate his own experience a lot more than might be ideal. If SSRIs didn’t help him, they are useless, and also the only kind of antidepressant. If getting into a green space helped him, a Londoner, someone who lives in the countryside will not be depressed in the first place. And so forth. It can also be argued that he cherry-picked data to arrive at some of his pre-decided conclusions. He also misinterprets data sometimes; which is understandable; he is after all a journalist, not a scientist.
Nevertheless, he offers a fresh perspective with a lot of ideas, and whether or not we agree with them all, new ideas tend to be worth reading. And if even one of his nine ideas helps you, that’s a win.
Bottom line: if you’d like to explore the treatment of depression from a direction other than medicalization or psychotherapy, then this is will be a good book for you.
Click here to check out Lost Connections, and reforge yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fennel vs Onion – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing fennel to onion, we picked the fennel.
Why?
First note, in case you didn’t see the picture: we are talking about white onions here (also called brown onions, by virtue of their attire).
Looking at the macros, fennel has nearly 2x the fiber and a little more protein, while onion has more carbs. An easy win in this category for the fennel.
In the category of vitamins, fennel has more of vitamins A, B2, B3, B5, B9, C, E, K, and choline (most of them by generous margins and some by especially large margins, we are talking, for example, 480x the vitamin A, 29x the vitamin E, and 157x the vitamin K), while onions have more of vitmains B1 and B6. Another clear win for fennel.
When it comes to minerals, fennel has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while onion is not higher in any minerals. No prizes for guessing: fennel wins this category too.
You may be curious as to how they add up on the polyphenol front, and the answer is, they don’t, much. Wonderful as these two vegetables are, an abundance of polyphenols is not amongst their strengths; fennel has some lignans and onion has some flavonols, but we’re talking tiny numbers here (in contrast, red onion would have aced it with 120mg/100g quercetin, amongst others, but red onion wasn’t on trial today).
Adding up the sections makes a clear win for fennel today.
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Are The “Bright Lines” Of Bright Line Eating?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
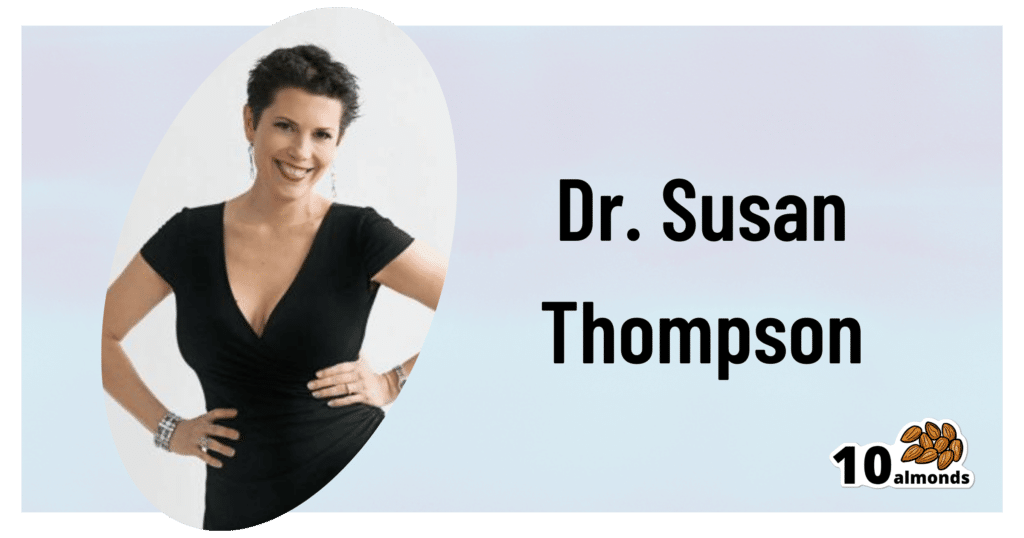
This is Dr. Susan Thompson. She’s a cognitive neuroscientist who has turned her hand to helping people to lose weight and maintain it at a lower level, using psychology to combat overeating. She is the founder of “Bright Line Eating”.
We’ll say up front: it’s not without some controversy, and we’ll address that as we go, but we do believe the ideas are worth examining, and then we can apply them or not as befits our personal lives.
What does she want us to know?
Bright Line Eating’s general goal
Dr. Thompson’s mission statement is to help people be “happy, thin, and free”.
You will note that this presupposes thinness as desirable, and presumes it to be healthy, which frankly, it’s not for everyone. Indeed, for people over a certain age, having a BMI that’s slightly into the “overweight” category is a protective factor against mortality (which is partly a flaw of the BMI system, but is an interesting observation nonetheless):
When BMI Doesn’t Quite Measure Up
Nevertheless, Dr. Thompson makes the case for the three items (happy, thin, free) coming together, which means that any miserable or unhealthy thinness is not what the approach is valuing, since it is important for “thin” to be bookended by “happy” and “free”.
What are these “bright lines”?
Bright Line Eating comes with 4 rules:
- No flour (no, not even wholegrain flour; enjoy whole grains themselves yes, but flour, no)
- No sugar (and as a tag-along to this, no alcohol) (sugars naturally found in whole foods, e.g. the sugar in an apple if eating an apple, is ok, but other kinds are not, e.g. foods with apple juice concentrate as a sweetener; no “natural raw cane sugar” etc is not allowed either; despite the name, it certainly doesn’t grow on the plant like that)
- No snacking, just three meals per day(not even eating the ingredients while cooking—which also means no taste-testing while cooking)
- Weigh all your food (have fun in restaurants—but more seriously, the idea here is to plan each day’s 3 meals to deliver a healthy macronutrient balance and a capped calorie total).
You may be thinking: “that sounds dismal, and not at all bright and cheerful, and certainly not happy and free”
The name comes from the idea that these rules are lines that one does not cross. They are “bright” lines because they should be observed with a bright and cheery demeanour, for they are the rules that, Dr. Thompson says, will make you “happy, thin, and free”.
You will note that this is completely in opposition to the expert opinion we hosted last week:
What Flexible Dieting Really Means
Dr. Thompson’s position on “freedom” is that Bright Line Eating is “very structured and takes a liberating stand against moderation”
Which may sound a bit of an oxymoron—is she really saying that we are going to be made free from freedom?
But there is some logic to it, and it’s about the freedom from having to make many food-related decisions at times when we’re likely to make bad ones:
Where does the psychology come in?
Dr. Thompson’s position is that willpower is a finite, expendable resource, and therefore we should use it judiciously.
So, much like Steve Jobs famously wore the same clothes every day because he had enough decisions to make later in the day that he didn’t want unnecessary extra decisions to make… Bright Line Eating proposes that we make certain clear decisions up front about our eating, so then we don’t have to make so many decisions (and potentially the wrong decisions) later when hungry.
You may be wondering: ”doesn’t sticking to what we decided still require willpower?”
And… Potentially. But the key here is shutting down self-negotiation.
Without clear lines drawn in advance, one must decide, “shall I have this cake or not?”, perhaps reflecting on the pros and cons, the context of the situation, the kind of day we’re having, how hungry we are, what else there is available to eat, what else we have eaten already, etc etc.
In short, there are lots of opportunities to rationalize the decision to eat the cake.
With clear lines drawn in advance, one must decide, “shall I have this cake or not?” and the answer is “no”.
So while sticking to that pre-decided “no” still may require some willpower, it no longer comes with a slew of tempting opportunities to rationalize a “yes”.
Which means a much greater success rate, both in adherence and outcomes. Here’s an 8-week interventional study and 2-year follow-up:
Bright Line Eating | Research Publications
Counterpoint: pick your own “bright lines”
Dr. Thompson is very keen on her 4 rules that have worked for her and many people, but she recognizes that they may not be a perfect fit for everyone.
So, it is possible to pick and choose our own “bright lines”; it is after all a dietary approach, not a religion. Here’s her response to someone who adopted the first 3 rules, but not the 4th:
Bright Lines as Guidelines for Weight Loss
The most important thing for Bright Line Eating, therefore, is perhaps the action of making clear decisions in advance and sticking to them, rather than seat-of-the-pantsing our diet, and with it, our health.
Want to know more from Dr. Thompson?
You might like her book, which we reviewed a while ago:
Bright Line Eating – by Dr. Susan Peirce Thompson
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: