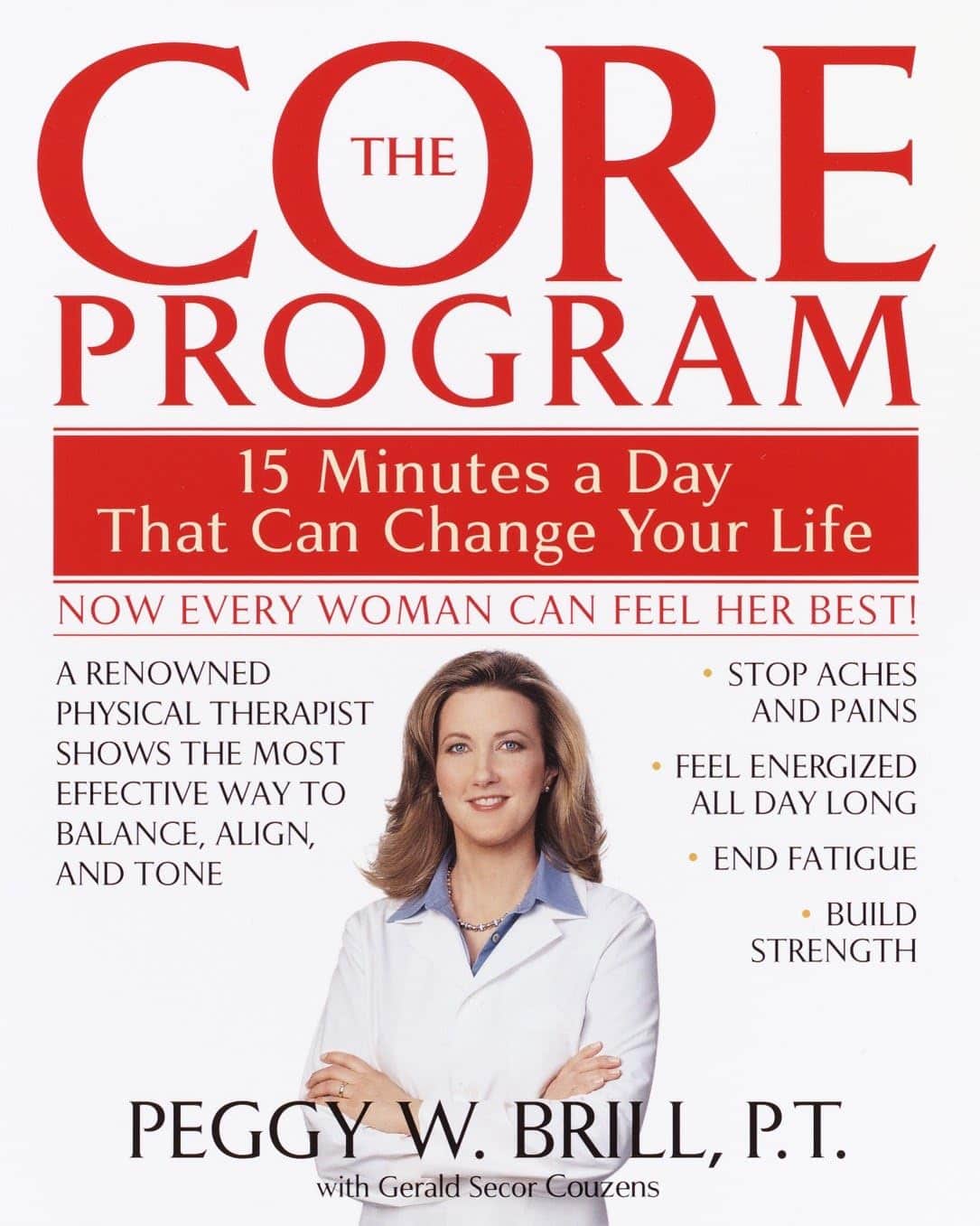
The Core Program: – by Peggy Brill
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a specialist women’s physiotherapist, has produced not only an exercise program, but also an explanation of various body-related matters can be easily neglected—but also, with the right knowledge and a small daily commitment of practice, easily addressed.
Thus, thus subtitular claim of “15 minutes a day that can change your life” is referring to a daily 15-minute exercise session, that’s very Pilates-like in its functional strength and mobility focus with little or no equipment, without actually being Pilates.
After some introductory chapters discussing the things we need to know in order to implement the program with full understanding, she gets into the program itself, which consists of three progressive parts:
- a foundation to get going
- an intermediate level to get things truly into good shape, and
- an advanced level for if one wants to take things further.
She also provides extra advice on maintaining what one gained, taking the program forwards for life.
The program is optimized for women, but there’s nothing truly exclusive to women here, just, occasional “this affects women more” things to include.
The style is a little dated (the book being published in 2003), but this does not meaningfully affect the content, as the information itself is timeless.
Bottom line: if you’d like to get into good condition without overcomplicating things and without needing a lot of resources, this book is quite a comprehensive course!
Click here to check out The Core Program, and get into shape sustainably!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Ghanaian Red Bean & Sweet Potato Groundnut Stew
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a dish popular in principle throughout West Africa. We say “in principle” because that’s a big place, and there is a lot of regional variation. The archetypal peanut stew is from Senegal (as maafe) or Mali (as tigadèguèna), but for its more balanced nutritional profile we’ve chosen one from Ghana—and since there are regional variations within Ghana too, we should specify that this one is from the south.
If you are allergic to nuts, you can substitute a seed butter (or tahini) for the nut butter, and omit the nuts—this will work in culinary terms and be fine healthwise, but we can’t claim it would be the same dish, having lost its defining ingredient. If your allergy is solely to peanuts, then substituting with any oily nut would work. So, not almonds for example, but cashews or even walnuts would be fine.
You will need
- 1½ lbs sweet potatoes, peeled and cut into ½” cubes
- 2 cups low-sodium vegetable stock
- 2 cans kidney beans, drained, cooked, and rinsed (or 2 cups same; cooked, drained, and rinsed)
- 1 can chopped tomatoes
- ½ cup unsalted dry-roasted peanuts
- 1 onion, chopped
- 1 red bell pepper, deseeded and chopped
- ¼ bulb garlic, finely chopped
- 2 heaped tbsp unsalted peanut butter, minimal (ideally: no) additives
- 2 tsp white miso paste
- 2 tsp grated fresh ginger
- 1 tsp ground cumin
- 1 tsp cayenne pepper
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- ½ tsp coarsely ground nigella seeds
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, or other pan suitable for both frying and fitting the entire stew in. Fry the onions until softened, turn the heat down low, and add the garlic, ginger, red bell pepper, cumin, cayenne, black pepper, and MSG/salt.
2) Add ¼ cup of the vegetable stock, and the sweet potato, and turn the heat back up, on high for about 30 seconds to get it to temperature, and then take it down to a simmer.
3) Stir in the miso paste and chopped tomatoes.
4) Add most of the rest of the vegetable stock, keeping ¼ cup aside. Simmer for about 20 minutes.
5) Stir in the kidney beans, and simmer for about 30 minutes more—the sweet potato should be soft now; if it isn’t, let it simmer a while longer until it is.
6) Combine the peanut butter with the remaining ¼ cup vegetable stock, and blend until smooth. Stir it into the stew.
7) If the stew is looking more like a soup than a stew, take out 1 cup and blend this 1 cup to a purée, adding it back in.
8) Add half the peanuts unto the stew. Taste, and adjust the seasonings if necessary.
9) Crush the remaining peanuts using a pestle and mortar; not too much though; you want them broken into bits, not pulverised.
10) Garnish with the crushed nuts and nigella seeds, and serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we used 4/5 today!
Take care!
Share This Post
-
I’m Moving Forward and Facing the Uncertainty of Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It takes a lot of courage to grow old.
I’ve come to appreciate this after conversations with hundreds of older adults over the past eight years for nearly 200 “Navigating Aging” columns.
Time and again, people have described what it’s like to let go of certainties they once lived with and adjust to new circumstances.
These older adults’ lives are filled with change. They don’t know what the future holds except that the end is nearer than it’s ever been.
And yet, they find ways to adapt. To move forward. To find meaning in their lives. And I find myself resolving to follow this path as I ready myself for retirement.
Patricia Estess, 85, of the Brooklyn borough of New York City spoke eloquently about the unpredictability of later life when I reached out to her as I reported a series of columns on older adults who live alone, sometimes known as “solo agers.”
Estess had taken a course on solo aging. “You realize that other people are in the same boat as you are,” she said when I asked what she had learned. “We’re all dealing with uncertainty.”
Consider the questions that older adults — whether living with others or by themselves — deal with year in and out: Will my bones break? Will my thinking skills and memory endure? Will I be able to make it up the stairs of my home, where I’m trying to age in place?
Will beloved friends and family members remain an ongoing source of support? If not, who will be around to provide help when it’s needed?
Will I have enough money to support a long and healthy life, if that’s in the cards? Will community and government resources be available, if needed?
It takes courage to face these uncertainties and advance into the unknown with a measure of equanimity.
“It’s a question of attitude,” Estess told me. “I have honed an attitude of: ‘I am getting older. Things will happen. I will do what I can to plan in advance. I will be more careful. But I will deal with things as they come up.’”
For many people, becoming old alters their sense of identity. They feel like strangers to themselves. Their bodies and minds aren’t working as they used to. They don’t feel the sense of control they once felt.
That requires a different type of courage — the courage to embrace and accept their older selves.
Marna Clarke, a photographer, spent more than a dozen years documenting her changing body and her life with her partner as they grew older. Along the way, she learned to view aging with new eyes.
“Now, I think there’s a beauty that comes out of people when they accept who they are,” she told me in 2022, when she was 70, just before her 93-year-old husband died.
Arthur Kleinman, a Harvard professor who’s now 83, gained a deeper sense of soulfulness after caring for his beloved wife, who had dementia and eventually died, leaving him grief-stricken.
“We endure, we learn how to endure, how to keep going. We’re marked, we’re injured, we’re wounded. We’re changed, in my case for the better,” he told me when I interviewed him in 2019. He was referring to a newfound sense of vulnerability and empathy he gained as a caregiver.
Herbert Brown, 68, who lives in one of Chicago’s poorest neighborhoods, was philosophical when I met him at his apartment building’s annual barbecue in June.
“I was a very wild person in my youth. I’m surprised I’ve lived this long,” he said. “I never planned on being a senior. I thought I’d die before that happened.”
Truthfully, no one is ever prepared to grow old, including me. (I’m turning 70 in February.)
Chalk it up to denial or the limits of imagination. As May Sarton, a writer who thought deeply about aging, put it so well: Old age is “a foreign country with an unknown language.” I, along with all my similarly aged friends, are surprised we’ve arrived at this destination.
For me, 2025 is a turning point. I’m retiring after four decades as a journalist. Most of that time, I’ve written about our nation’s enormously complex health care system. For the past eight years, I’ve focused on the unprecedented growth of the older population — the most significant demographic trend of our time — and its many implications.
In some ways, I’m ready for the challenges that lie ahead. In many ways, I’m not.
The biggest unknown is what will happen to my vision. I have moderate macular degeneration in both eyes. Last year, I lost central vision in my right eye. How long will my left eye pick up the slack? What will happen when that eye deteriorates?
Like many people, I’m hoping scientific advances outpace the progression of my condition. But I’m not counting on it. Realistically, I have to plan for a future in which I might become partially blind.
It’ll take courage to deal with that.
Then, there’s the matter of my four-story Denver house, where I’ve lived for 33 years. Climbing the stairs has helped keep me in shape. But that won’t be possible if my vision becomes worse.
So my husband and I are taking a leap into the unknown. We’re renovating the house, installing an elevator, and inviting our son, daughter-in-law, and grandson to move in with us. Going intergenerational. Giving up privacy. In exchange, we hope our home will be full of mutual assistance and love.
There are no guarantees this will work. But we’re giving it a shot.
Without all the conversations I’ve had over all these years, I might not have been up for it. But I’ve come to see that “no guarantees” isn’t a reason to dig in my heels and resist change.
Thank you to everyone who has taken time to share your experiences and insights about aging. Thank you for your openness, honesty, and courage. These conversations will become even more important in the years ahead, as baby boomers like me make their way through their 70s, 80s, and beyond. May the conversations continue.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Share This Post
-
The Burden of Getting Medical Care Can Exhaust Older Patients
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Susanne Gilliam, 67, was walking down her driveway to get the mail in January when she slipped and fell on a patch of black ice.
Pain shot through her left knee and ankle. After summoning her husband on her phone, with difficulty she made it back to the house.
And then began the run-around that so many people face when they interact with America’s uncoordinated health care system.
Gilliam’s orthopedic surgeon, who managed previous difficulties with her left knee, saw her that afternoon but told her “I don’t do ankles.”
He referred her to an ankle specialist who ordered a new set of X-rays and an MRI. For convenience’s sake, Gilliam asked to get the scans at a hospital near her home in Sudbury, Massachusetts. But the hospital didn’t have the doctor’s order when she called for an appointment. It came through only after several more calls.
Coordinating the care she needs to recover, including physical therapy, became a part-time job for Gilliam. (Therapists work on only one body part per session, so she has needed separate visits for her knee and for her ankle several times a week.)
“The burden of arranging everything I need — it’s huge,” Gilliam told me. “It leaves you with such a sense of mental and physical exhaustion.”
The toll the American health care system extracts is, in some respects, the price of extraordinary progress in medicine. But it’s also evidence of the poor fit between older adults’ capacities and the health care system’s demands.
“The good news is we know so much more and can do so much more for people with various conditions,” said Thomas H. Lee, chief medical officer at Press Ganey, a consulting firm that tracks patients’ experiences with health care. “The bad news is the system has gotten overwhelmingly complex.”
That complexity is compounded by the proliferation of guidelines for separate medical conditions, financial incentives that reward more medical care, and specialization among clinicians, said Ishani Ganguli, an associate professor of medicine at Harvard Medical School.
“It’s not uncommon for older patients to have three or more heart specialists who schedule regular appointments and tests,” she said. If someone has multiple medical problems — say, heart disease, diabetes, and glaucoma — interactions with the health care system multiply.
Ganguli is the author of a new study showing that Medicare patients spend about three weeks a year having medical tests, visiting doctors, undergoing treatments or medical procedures, seeking care in emergency rooms, or spending time in the hospital or rehabilitation facilities. (The data is from 2019, before the covid pandemic disrupted care patterns. If any services were received, that counted as a day of health care contact.)
That study found that slightly more than 1 in 10 seniors, including those recovering from or managing serious illnesses, spent a much larger portion of their lives getting care — at least 50 days a year.
“Some of this may be very beneficial and valuable for people, and some of it may be less essential,” Ganguli said. “We don’t talk enough about what we’re asking older adults to do and whether that’s realistic.”
Victor Montori, a professor of medicine at the Mayo Clinic in Rochester, Minnesota, has for many years raised an alarm about the “treatment burden” that patients experience. In addition to time spent receiving health care, this burden includes arranging appointments, finding transportation to medical visits, getting and taking medications, communicating with insurance companies, paying medical bills, monitoring health at home, and following recommendations such as dietary changes.
Four years ago — in a paper titled “Is My Patient Overwhelmed?” — Montori and several colleagues found that 40% of patients with chronic conditions such as asthma, diabetes, and neurological disorders “considered their treatment burden unsustainable.”
When this happens, people stop following medical advice and report having a poorer quality of life, the researchers found. Especially vulnerable are older adults with multiple medical conditions and low levels of education who are economically insecure and socially isolated.
Older patients’ difficulties are compounded by medical practices’ increased use of digital phone systems and electronic patient portals — both frustrating for many seniors to navigate — and the time pressures afflicting physicians. “It’s harder and harder for patients to gain access to clinicians who can problem-solve with them and answer questions,” Montori said.
Meanwhile, clinicians rarely ask patients about their capacity to perform the work they’re being asked to do. “We often have little sense of the complexity of our patients’ lives and even less insight into how the treatments we provide (to reach goal-directed guidelines) fit within the web of our patients’ daily experiences,” several physicians wrote in a 2022 paper on reducing treatment burden.
Consider what Jean Hartnett, 53, of Omaha, Nebraska, and her eight siblings went through after their 88-year-old mother had a stroke in February 2021 while shopping at Walmart.
At the time, the older woman was looking after Hartnett’s father, who had kidney disease and needed help with daily activities such as showering and going to the bathroom.
During the year after the stroke, both of Hartnett’s parents — fiercely independent farmers who lived in Hubbard, Nebraska — suffered setbacks, and medical crises became common. When a physician changed her mom’s or dad’s plan of care, new medications, supplies, and medical equipment had to be procured, and new rounds of occupational, physical, and speech therapy arranged.
Neither parent could be left alone if the other needed medical attention.
“It wasn’t unusual for me to be bringing one parent home from the hospital or doctor’s visit and passing the ambulance or a family member on the highway taking the other one in,” Hartnett explained. “An incredible amount of coordination needed to happen.”
Hartnett moved in with her parents during the last six weeks of her father’s life, after doctors decided he was too weak to undertake dialysis. He passed away in March 2022. Her mother died months later in July.
So, what can older adults and family caregivers do to ease the burdens of health care?
To start, be candid with your doctor if you think a treatment plan isn’t feasible and explain why you feel that way, said Elizabeth Rogers, an assistant professor of internal medicine at the University of Minnesota Medical School.
“Be sure to discuss your health priorities and trade-offs: what you might gain and what you might lose by forgoing certain tests or treatments,” she said. Ask which interventions are most important in terms of keeping you healthy, and which might be expendable.
Doctors can adjust your treatment plan, discontinue medications that aren’t yielding significant benefits, and arrange virtual visits if you can manage the technological requirements. (Many older adults can’t.)
Ask if a social worker or a patient navigator can help you arrange multiple appointments and tests on the same day to minimize the burden of going to and from medical centers. These professionals can also help you connect with community resources, such as transportation services, that might be of help. (Most medical centers have staff of this kind, but physician practices do not.)
If you don’t understand how to do what your doctor wants you to do, ask questions: What will this involve on my part? How much time will this take? What kind of resources will I need to do this? And ask for written materials, such as self-management plans for asthma or diabetes, that can help you understand what’s expected.
“I would ask a clinician, ‘If I chose this treatment option, what does that mean not only for my cancer or heart disease, but also for the time I’ll spend getting care?’” said Ganguli of Harvard. “If they don’t have an answer, ask if they can come up with an estimate.”
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit http://kffhealthnews.org/columnists to submit your requests or tips.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
Puritans Pride Resveratrol vs Life Extension Resveratrol – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Puritan’s Pride Resveratrol to Life Extension Resveratrol, we picked the Life Extension Resveratrol.
Why?
It contains not only more resveratrol per serving (250mg compared to Puritan’s Pride’s 100mg), but also contains other goodies too. Specifically, each capsule also contains:
- Quercetin (150mg)
- Grape & berry blend (85mg)
- Fisetin (10mg)
Whereas the Puritan’s Pride softgels? The other top ingredients are soybean oil and gelatin.
Want to check out the products for yourself? Here they are:
Puritan’s Pride Resveratrol | Life Extension Resveratrol
Want to know more about these supplements? Check out:
Resveratrol & Healthy Aging
Fight Inflammation & Protect Your Brain, With Quercetin
Berries & Other Polyphenol-rich Foods
Fisetin: The Anti-Aging AssassinEnjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Mushrooms vs Eggplant – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mushrooms to eggplant, we picked the mushrooms.
Why?
First, you may be wondering: which mushrooms? Button mushrooms? White mushrooms? Chestnut mushrooms? Portobello mushrooms? And the answer is yes. Those (and more; it represents most mushrooms that are commonly sold fresh in western supermarkets) are all the same species at different ages; namely, Agaricus bisporus—not to be mistaken for fly agaric, which despite the name, is not even a member of the Agaricus genus, and is in fact Amanita muscari. This is an important distinction, because fly agaric is poisonous, though fatality is rare, and it’s commonly enjoyed recreationally (after some preparation, which reduces its toxicity) for its psychoactive effects. It’s the famous red one with white spots. Anyway, today we will be talking instead about Agaricus bisporus, which is most popular western varieties of “edible mushroom”.
With that in mind, let’s get down to it:
In terms of macros, mushrooms contain more than 3x the protein, while eggplant contains nearly 2x the carbs and 3x the fiber. We’ll call this a tie for macros.
As for vitamins, mushrooms contain more of vitamins B1, B2, B3, B5, B6, B7, B9, B12, D, and choline, while eggplant contains more of vitamins A, E, and K. Most notably for vegans, mushrooms are a good non-animal source of vitamins B12 and D, which nutrients are not generally found in plants. Mushrooms, of course, are not technically plants. In any case, the vitamins category is an easy win for mushrooms.
When it comes to minerals, mushrooms have more copper, iron, phosphorus, potassium, selenium, and zinc, while eggplant has more calcium, magnesium, and manganese. Another easy win for mushrooms.
One final thing worth noting is that mushrooms are a rich source of the amino acid ergothioneine, which has been called a “longevity vitamin” for its healthspan-increasing effects (see our article below).
Meanwhile, in the category of mushrooms vs eggplant, mushrooms don’t leave much room for doubt and are the clear winner here.
Want to learn more?
You might like to read:
The Magic of Mushrooms: “The Longevity Vitamin” (That’s Not A Vitamin)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dealing with Thirst!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Busting The Myth of “Eight Glasses Of Water A Day”
Everyone knows we must drink 8 glasses of water a day, or else we’re going to get a failing grade at being a healthy human—like not flossing, or not using adequate sunscreen.
But… Do we? And does tea count? How about (we dare but whisper it) coffee? And soda drinks are mostly water, right? But aren’t some drinks dehydrating? Are special electrolyte drinks really better? There are so many things to consider, so many differing advices, and it’s easy to give up, or just choose what to believe in as a leap of faith.
A quick brain-teaser for you first, though:
If coffee and soda don’t count because they’re dehydrating, then what if you were to take:
– A concentrated tiny cup of espresso, and then a glass of water, would the glass of water count?
– Or (we don’t relish the thought) what if you took a spoonful of soda syrup, and then a glass of water, would the glass of water count?
If your answer was “yes, it’s a glass of water”, then why would it not count if it were taken all at once (e.g. as an Americano coffee, or a regular soda)?
If your answer was “yes, but that water might only offset the dehydration caused by the coffee/syrup, so I might only be breaking even”, then you were thinking about this the right way:
How much water you need depends on many factors that can be affected by what else you are consuming and what else you are doing. Science loves averages, so eight glasses a day may be great if you are of average health, and average body size, in a temperate climate, doing moderate exercise, and so on and so on.
If you’re not the most average person of all time? You may need to take into account a lot of factors, ranging from what you ate for dinner to how much you perspired during your morning exercises. As you (probably) don’t live in laboratory conditions, this can become an impossible task—and if you missed (or guessed incorrectly) even one factor, the whole calculation will be thrown off. But is there any other way to know?
What of the infamous pee test? Drink enough to make your urine as clear as possible, and if it’s dark, you’re dehydrated, common wisdom says.
In reality, however, that tells you not what’s in your body, but rather, what got ejected from your body. If your urine is dark, it might mean you had too little water, but it also could just mean you had the right amount of water but too much sodium, for instance. A study of this was done on athletes, and found no correlation between urine color and actual bodily hydration when measured directly via a blood test.
So, if we can’t just have an app tell us “drink this many glasses of water”, and we can’t trust urine color, what can we do?
What we can do is trust that our body comes with (for free!) a wonderful homeostatic system and it will try to correct any imbalances. If you are thirsty, you’re dehydrated. Drink something with plenty of water in, if not plain water.
But what about special electrolyte drinks? If you need salts, you will crave them. Craving a salty snack? Go for it! Or if you prefer not to snack, do a salt lick test (just put a little salt on your finger, and taste it; if it tastes good, wait a minute or two, and then have a little more, and repeat until it doesn’t).
Bonus Tip:
- Make sure you always have a source of hydration (that you enjoy!) to hand. Maybe it’s chilled water, maybe it’s a pot of tea, maybe it’s a sports drink, it doesn’t matter too much. Even coffee is actually fine, by the way (but don’t overdo it).
- Make a personal rule: “I will always make time for hydration”. That means, if you’re thirsty, have something with water in it now. Not when you’ve finished what you’re doing (unless you really can’t stop, because you are a racecar driver mid-race, or a surgeon mid-operation, or something), but now. Do not postpone it until after you’ve done some other thing first; you will forget and it will keep getting postponed. Always make time for water.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: