Which Tea Is Best, By Science?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What kind of tea is best for the health?
It’s popular knowledge that tea is a healthful drink, and green tea tends to get the popular credit for “healthiest”.
Is that accurate? It depends on what you’re looking for…
Black
Its strong flavor packs in lots of polyphenols, often more than other kinds of tea. This brings some great benefits:
As well as effects beyond the obvious:
…and its cardioprotective benefits aren’t just about lowering blood pressure; it improves triglyceride levels as well as improving the LDL to HDL ratio:
The effect of black tea on risk factors of cardiovascular disease in a normal population
Finally (we could say more, but we only have so much room), black tea usually has the highest caffeine content, compared to other teas.
That’s good or bad depending on your own physiology and preferences, of course.
White
White tea hasn’t been processed as much as other kinds, so this one keeps more of its antioxidants, but that doesn’t mean it comes out on top; in this study of 30 teas, the white tea options ranked in the mid-to-low 20s:
White tea is also unusual in its relatively high fluoride content, which is consider a good thing:
White tea: A contributor to oral health
In case you were wondering about the safety of that…
Water Fluoridation: Is It Safe, And How Much Is Too Much?
Green
Green tea ranks almost as high as black tea, on average, for polyphenols.
Its antioxidant powers have given it a considerable anti-cancer potential, too:
- Green tea consumption and breast cancer risk or recurrence: a meta-analysis
- Green tea consumption and prostate cancer risk: a prospective study
…and many others, but you get the idea. Notably:
Green Tea Catechins: Nature’s Way of Preventing and Treating Cancer
…or to expand on that:
About green tea’s much higher levels of catechins, they also have a neuroprotective effect:
Green tea of course is also a great source of l-theanine, which we could write a whole main feature about, and we did:
Red
Also called “rooibos” or (literally translated from Afrikaans to English) “redbush”, it’s quite special in that despite being a “true tea” botanically and containing many of the same phytochemicals as the other teas, it has no caffeine.
There’s not nearly as much research for this as green tea, but here’s one that stood out:
However, in the search for the perfect cup of tea (in terms of phytochemical content), another set of researchers found:
❝The optimal cup was identified as sample steeped for 10 min or longer. The rooibos consumers did not consume it sufficiently, nor steeped it long enough. ❞
Read in full: Rooibos herbal tea: an optimal cup and its consumers
Bottom line
Black, white, green, and red teas all have their benefits, and ultimately the best one for you will probably be the one you enjoy drinking, and thus drink more of.
If trying to choose though, we offer the following summary:
- 🖤 Black tea: best for total beneficial phytochemicals
- 🤍 White tea:best for your oral health
- 💚 Green tea: best for your brain
- ❤️ Red tea: best if you want naturally caffeine-free
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Studies of Parkinson’s disease have long overlooked Pacific populations – our work shows why that must change
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A form of Parkinson’s disease caused by mutations in a gene known as PINK1 has long been labelled rare. But our research shows it’s anything but – at least for some populations.
Our meta-analysis revealed that people in specific Polynesian communities have a much higher rate of PINK1-linked Parkinson’s than expected. This finding reshapes not only our understanding of who is most at risk, but also how soon symptoms may appear and what that might mean for treatment and testing.
Parkinson’s disease is often thought of as a single condition. In reality, it is better understood as a group of syndromes caused by different factors – genetic, environmental or a combination of both.
These varying causes lead to differences in disease patterns, progression and subsequent diagnosis. Recognising this distinction is crucial as it paves the way for targeted interventions and may even help prevent the disease altogether.
Shutterstock/sfam_photo Why we focus on PINK1-linked Parkinson’s
We became interested in this gene after a 2021 study highlighted five people of Samoan and Tongan descent living in New Zealand who shared the same PINK1 mutation.
Previously, this mutation had been spotted only in a few more distant places –Malaysia, Guam and the Philippines. The fact it appeared in people from Samoan and Tongan backgrounds suggested a historical connection dating back to early Polynesian migrations.
One person in 1,300 West Polynesians carries this mutation. This is a frequency well above what scientists usually classify as rare (below one in 2,200). This discovery means we may be overlooking entire communities in Parkinson’s research if we continue to assume PINK1-linked cases are uncommon.
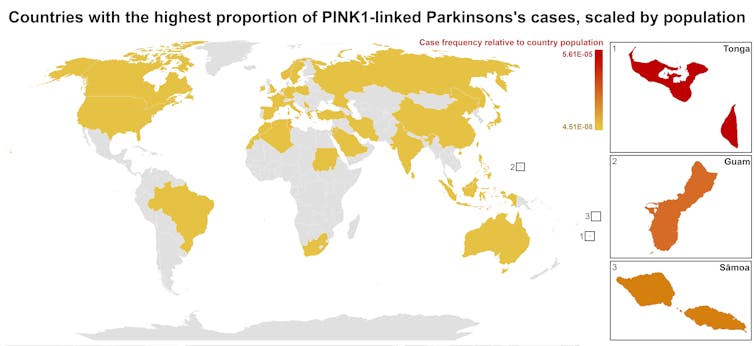
This world map shows people in some Polynesian communities have a much higher rate of PINK1-linked Parkinson’s than the global population. Eden Yin, CC BY-SA Traditional understanding says PINK1-linked Parkinson’s is both rare and typically strikes younger people, mostly in their 30s or 40s, if they inherit two faulty copies of the gene. In other words, it’s considered a recessive condition, needing two matching puzzle pieces before the disease can unfold.
Our work challenges this view. We show that even one defective PINK1 gene can cause Parkinson’s at an average age of 43, much earlier than the typical onset after 65. That’s a significant departure from the standard belief that only people with two defective gene copies are at risk.
Why this matters for people with the disease
It’s not just genetics that challenge long-held views. Historically, PINK1-linked Parkinson’s was thought to lack some of the classic features of the disease, such as toxic clumps of alpha-synuclein protein.
In typical Parkinson’s, alpha-synuclein builds up in the brain, forming sticky clumps known as Lewy bodies. Our results, contrary to prior beliefs, show that alpha-synuclein pathology is present in 87.5% of PINK1 cases. This finding opens up a promising new avenue for future treatment development.
The biggest concern is early onset. PINK1-linked Parkinson’s can begin as early as 11 years old, although a more common starting point is around the mid-30s. This early onset means living longer with the disease, which can profoundly affect education, work opportunities and family life.
Current treatments (such as levodopa, a precursor of dopamine) help manage symptoms, but they’re not designed to address the root cause. If we know someone has a PINK1 mutation, scientists and clinicians can explore therapies for specific genetic pathways, potentially delivering relief beyond symptom management.
Sex differences add a layer of complexity
In Parkinson’s, generally, men are at higher risk and tend to develop symptoms earlier. However, our findings suggest the opposite pattern for PINK1-linked cases. Particularly, women with two defective copies of the gene experience onset earlier than men.
This highlights the need to consider sex-related factors in Parkinson’s research. Overlooking them risks missing key elements of the disease.
Genetic testing could be a game-changer for PINK1-linked Parkinson’s. Because it often appears earlier, doctors may not recognise it immediately, especially if they are more familiar with the common, later-onset form of Parkinson’s.
Early genetic testing could lead to a faster, more accurate diagnosis, allowing treatment to begin when interventions are most effective. It would help families understand how the disease is inherited, enabling relatives to get tested.
In some cases, where appropriate and culturally acceptable, embryo screening may be considered to prevent the passing of the faulty gene.
Knowing you have a PINK1 mutation could also make finding the right treatment more efficient. Instead of a lengthy trial-and-error process with different medications, doctors could use emerging therapies designed to target the underlying PINK1 mutation rather than relying on general Parkinson’s treatments meant for the broader population.
Addressing research gaps
These findings underscore how crucial it is to include diverse populations in health research.
Many communities, such as those in Samoa, Tonga and other Pacific nations, have had little to no involvement in global Parkinson’s genetics studies. This has created gaps in knowledge and real-world consequences for people who may not receive timely or accurate diagnoses.
Researchers, funding bodies and policymakers must prioritise projects beyond the usual focus on European or industrialised countries to ensure research findings and treatments are relevant to all affected populations.
To better diagnose and treat Parkinson’s, we need a more inclusive approach. Recognising that PINK1-linked Parkinson’s is not as rare as previously thought – and that genetics, sex differences and cultural factors all play a role – allows us to improve care for everyone.
By expanding genetic testing, refining treatments and ensuring research reflects the full spectrum of Parkinson’s, we can move closer to more precise diagnoses, targeted therapies and better support systems for all.
Victor Dieriks, Research Fellow in Health Sciences, University of Auckland, Waipapa Taumata Rau and Eden Paige Yin, PhD candidate in Health Sciences, University of Auckland, Waipapa Taumata Rau
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Older, Faster, Stronger – by Margaret Webb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, now in her 60s, made it her mission in her 50s to become the best runner she could. Before that, she’d been a keen runner previously, but let things slip rather in her 40s. But the book’s not about her 40s, it’s about her 50s and onwards, and other female runners in their 50s, 60s, 70s, 80s, and even 90s.
There’s a lot of this book that’s about people’s individual stories, and those should certainly be enough to prompt almost any reader that “if they can do it, I can”.
A lot, meanwhile, is about health and exercise science, training methods, and what has worked for various later-life athletes, including the author. So, it’s also partway instruction manual, with plenty of reference to science and medical considerations too.
Bottom line: sometimes, life throws us challenges. Sometimes, the best response is “Yeah? Bet” and surprise everyone.
Click here to check out Older, Faster, Stronger, and become all those cool things!
Share This Post
-
Can Home Tests Replace Check-Ups?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I recently hit 65 and try to get regular check-ups, but do you think home testing can be as reliable as a doctor visit? I try to keep as informed as I can and am a big believer in taking responsibility for my own health if I can, but I don’t want to miss something important either. Best as a supplemental thing, perhaps?❞
Depends what’s being tested! And your level of technical knowledge, though there’s always something to be said for ongoing learning.
- If you’re talking blood tests, urine tests, etc per at-home test kits that get sent off to a lab, then provided they’re well-sourced (and executed correctly by you), they should be as accurate as what a doctor will give, since they are basically doing the same thing (taking a sample and sending it off to a lab).
- If you’re talking about checking for lumps etc, then a dual approach is best: check yourself at home as often as you feel is reasonable (with once per month being advised at a minimum, especially if you’re aware of an extra risk factor for you) and check-ups with the doctor per their recommendations.
- If you’re talking about general vitals (blood pressure, heart rate, heart rate variability, VO₂ max, etc), then provided you have a reliable way of testing them, then doing them very frequently at home, to get the best “big picture” view. In contrast, getting them done once a year at your doctor’s could result in a misleading result, if you just ate something different that day or had a stressful morning, for example.
Enjoy
Share This Post
Related Posts
-
Can apps and digital resources support your child with autism or ADHD?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Neurodevelopmental conditions such as attention deficit hyperactivity disorder (ADHD) and autism affect about one in ten children. These conditions impact development, behaviour and wellbeing.
But children with these conditions and their caregivers often can’t get the support they need. Families report difficulties accessing health-care providers and experience long wait lists to receive care.
Digital tools, such as apps and websites, are often viewed as a solution to these gaps. With a single click or a download, families might be able to access information to support their child.
There are lots of digital tools available, but it’s hard to know what is and isn’t useful. Our new study evaluated freely available digital resources for child neurodevelopment and mental health to understand their quality and evidence base.
We found many resources were functional and engaging. However, resources often lacked evidence for the information provided and the claimed positive impact on children and families.
This is a common problem in the digital resource field, where the high expectations and claims of impact from digital tools to change health care have not yet been realised.
Fabio Principe/Shutterstock What type of resources?
Our study identified 3,435 separate resources, of which 112 (43 apps and 69 websites) met our criteria for review. These resources all claimed to provide information or supports for child neurodevelopment, mental health or wellbeing.
Resources had to be freely available, in English and have actionable information for children and families.
The most common focus was on autism, representing 17% of all resources. Resources suggested they provided strategies to promote speech, language and social development, and to support challenging behaviours.
Other common areas included language and communication (14%), and ADHD (10%).
Resources had various purposes, including journalling and providing advice, scheduling support, and delivering activities and strategies for parents. Resources delivered information interactively, with some apps organising content into structured modules.
Resources also provided options for alternative and assistive communication for people with language or communication challenges.
Most apps were functional and accessible
Our first question was about how engaging and accessible the information was. Resources that are hard to use aren’t used frequently, regardless of the information quality.
We evaluated aesthetics, including whether digital tools were easy to use and navigate, stylistically consistent, with clean and appealing graphics for users.
Most resources were rated as highly engaging, with strong accessibility and functionality.
Most apps and websites we evaluated were engaging. jamesteohart/Shutterstock But many lacked quality information
We ranked resources on various features from 1 (inadequate) to 5 (excellent), with a ranking of 3 considered acceptable. These ratings looked at how credible the resource was and whether there was evidence supporting it.
Despite their functionality, 37% of reviewed apps did not meet the minimum acceptable standards for information quality. This means many apps could not be recommended. Most websites fared better than apps.
There also wasn’t a lot of scientific evidence to suggest using either apps or digital resources actually helped families. Studies show long-term engagement with digital tools is rare, and downloads don’t correspond to frequent usage or benefits.
Digital tools are often viewed as a panacea to health-care gaps, but the evidence is yet to show they fill such gaps. Digital health is a fast-moving field and resources are often made available before they have been properly evaluated.
What should you look for in digital resources?
We found the highest quality resources were developed in collaboration with institutions, such as health, university or government groups.
One highly rated resource was the Raising Children’s Network and the associated app, Raising Healthy Minds. These are co-developed with a university and hospital, and by people with appropriate qualifications.
This resource provides information to support children’s overall health, development and wellbeing, with dedicated sections addressing neurodevelopmental needs and concerns.
The Raising Children Network provides resources for child health, including neurodevelopmental needs. Raising Children Network screenshot Our research shows parents can assess whether digital resources are high quality by checking they are:
- factually correct. Look for where the app or resource is getting its information. Does the author have the qualifications and training to provide the information? Are they a registered health expert who is accountable to a regulatory body (such as AHPRA, the Australian Health Practitioners Regulation Agency) for providing information that does not cause harm?
- consistent across multiple credible sources, such as health institutions.
- linked to supporting information. Look for reliable links to reputable institutions. Links to peer-reviewed scientific journals are often helpful as those articles will also usually describe the limitations of the research presented.
- up-to-date. Apps should be frequently updated. For websites, dates of update are usually found on the homepage or at the bottom of individual pages.
Check when information was last updated. fizkes/Shutterstock Beware of red flags
Some things to watch out for are:
- testimonials and anecdotes without evidence and scientific links to back the anecdotes up. If it sounds too good to be true, it probably is.
- no information provided about conflicts of interest. Organisations gain when you click on their links or take their advice (financial, reputation and brand development). Think about what they gain when you use their information to help keep a balanced perspective.
Remember, the app’s star rating doesn’t mean it will contain factual information from a reliable source or be helpful for you and your child.
The role of digital tools
Digital tools won’t usually replace a health professional, but they can support care in many different ways. They may be used to help to educate and prepare for meetings, and to collaborate with health providers.
They may also be used to collect information about daily needs. Studies show reporting on sleep in children can be notoriously difficult, for example. But tracking sleep behaviour with actigraphy, where movement and activity patterns are measured using a wearable device, can provide information to support clinical care. With the promise of artificial intelligence, there will also be new opportunities to support daily living.
Our findings reflect a broader problem for digital health, however. Much investment is often made in developing products to drive use, with spurious claims of health benefits.
What’s needed is a system that prioritises the funding, implementation and evaluation of tools to demonstrate benefits for families. Only then may we realise the potential of digital tools to benefit those who use them.
Kelsie Boulton, Senior Research Fellow in Child Neurodevelopment, Brain and Mind Centre, University of Sydney and Adam Guastella, Professor and Clinical Psychologist, Michael Crouch Chair in Child and Youth Mental Health, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy Relationship, Healthy Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Only One Kind Of Relationship Promotes Longevity This Much!
One of the well-established keys of a long healthy life is being in a fulfilling relationship. That’s not to say that one can’t be single and happy and fulfilled—one totally can. But statistically, those who live longest, do so in happy, fulfilling, committed relationships.
Note: happy, fulfilling, committed relationships. Less than that won’t do. Your insurance company might care about your marital status for its own sake, but your actual health doesn’t—it’s about the emotional safety and security that a good, healthy, happy, fulfilling relationship offers.
How to keep the “love coals” warm
When “new relationship energy” subsides and we’ve made our way hand-in-hand through the “honeymoon period”, what next? For many, a life of routine. And that’s not intrinsically bad—routine itself can be comforting! But for love to work, according to relational psychologists, it also needs something a little more.
What things? Let’s break it down…
Bids for connection—and responsiveness to same
There’s an oft-quoted story about a person who knew their marriage was over when their spouse wouldn’t come look at their tomatoes. That may seem overblown, but…
When we care about someone, we want to share our life with them. Not just in the sense of cohabitation and taxes, but in the sense of:
- Little moments of joy
- Things we learned
- Things we saw
- Things we did
…and there’s someone we’re first to go to share these things with. And when we do, that’s a “bid for connection”. It’s important that we:
- Make bids for connection frequently
- Respond appropriately to our partner’s bids for connection
Of course, we cannot always give everything our full attention. But whenever we can, we should show as much genuine interest as we can.
Keep asking the important questions
Not just “what shall we have for dinner?”, but:
- “What’s a life dream that you have at the moment?”
- “What are the most important things in life?”
- “What would you regret not doing, if you never got the chance?”
…and so forth. Even after many years with a partner, the answers can sometimes surprise us. Not because we don’t know our partners, but because the answers can change with time, and sometimes we can even surprise ourselves, if it’s a question we haven’t considered for a while.
It’s good to learn and grow like this together—and to keep doing so!
Express gratitude/appreciation
For the little things as well as the big:
- Thank you for staying by my side during life’s storms
- Thank you for bringing me a coffee
- Thank you for taking on these responsibilities with me
- I really appreciate your DIY skills
- I really appreciate your understanding nature
On which note…
Compliment, often and sincerely
Most importantly, compliment things intrinsic to their character, not just peripheral attributes like appearance, and also not just what they do for you.
- You’re such a patient person; I really admire that
- I really hit the jackpot to get someone I can trust so completely as you
- You are the kindest and sweetest soul I have ever encountered in life
- I love that you have such a blend of strength and compassion
- Your unwavering dedication to your personal values makes me so proud
…whatever goes for your partner and how you see them and what you love about them!
Express your needs, and ask about theirs
We’re none of us mind-readers, and it’s easy to languish in “if they really cared, I wouldn’t have to ask”, or conversely, “if they wanted something, they would surely say so”.
Communicate. Effectively. Life is too short to waste in miscommunication and unsaid things!
We covered much more detailed how-tos of this in a previous issue, but good double-whammy of top tier communication is:
- “I need…” / “Please will you…”
- “What do you need?” / “How can I help?”
Touch. Often.
It takes about 20 seconds of sustained contact for oxytocin to take effect, so remember that when you hug your partner, hold hands when walking, or cuddle up the sofa.
Have regular date nights
It doesn’t have to be fancy. A date night can be cooking together, it can be watching a movie together at home. It can be having a scheduled time to each bring a “big question” or five, from what we talked about above!
Most importantly: it’s a planned shared experience where the intent is to enjoy each other’s romantic company, and have a focus on each other. Having a regularly recurring date night, be it the last day of each month, or every second Saturday, or every Friday night, whatever your schedules allow, makes such a big difference to feel you are indeed “dating” and in the full flushes of love—not merely cohabiting pleasantly.
Want ideas?
Check out these:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The End of Heart Disease – by Dr. Joel Fuhrman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed another of Dr. Fuhrman’s books, “Eat To Live”, and this time, he’s focusing specifically on preventing/reversing heart disease.
Dr. Fuhrman takes the stance that our food can either kill or heal us, and we get to choose which. As such, nutrition is central to his heart-healthy plan; he mostly leaves matters of exercise, sleep, etc to other sources.
His dietary approach is mostly uncontroversial: for example, advices include: enjoy nutritionally dense foods, skip processed foods, eat at least mostly plants, skip the added salt. A slightly more controversial aspect is that he advocates for avoiding cooking oils, including the healthiest oils, including olive and avocado, which are by current scientific consensus considered heart-healthy in moderation. As in, not even just heart-neutral, but rather, they actively improve triglycerides.
He compares different cardioprotective diets, and while he’s not unbiased, he does provide 40 pages of scholarly references, so we may understand that at the very least, his approach is sound.
There are also recipes—94 pages of them—for any who might wonder “how do I cook without…?” and some ingredient he would rather you omit.
The style is information-dense (and this is a 448-page book) but still very readable.
Bottom line: if you’re serious about improving your heart health, this book can help a lot with that.
Click here to check out The End Of Heart Disease, and end heart disease for yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: