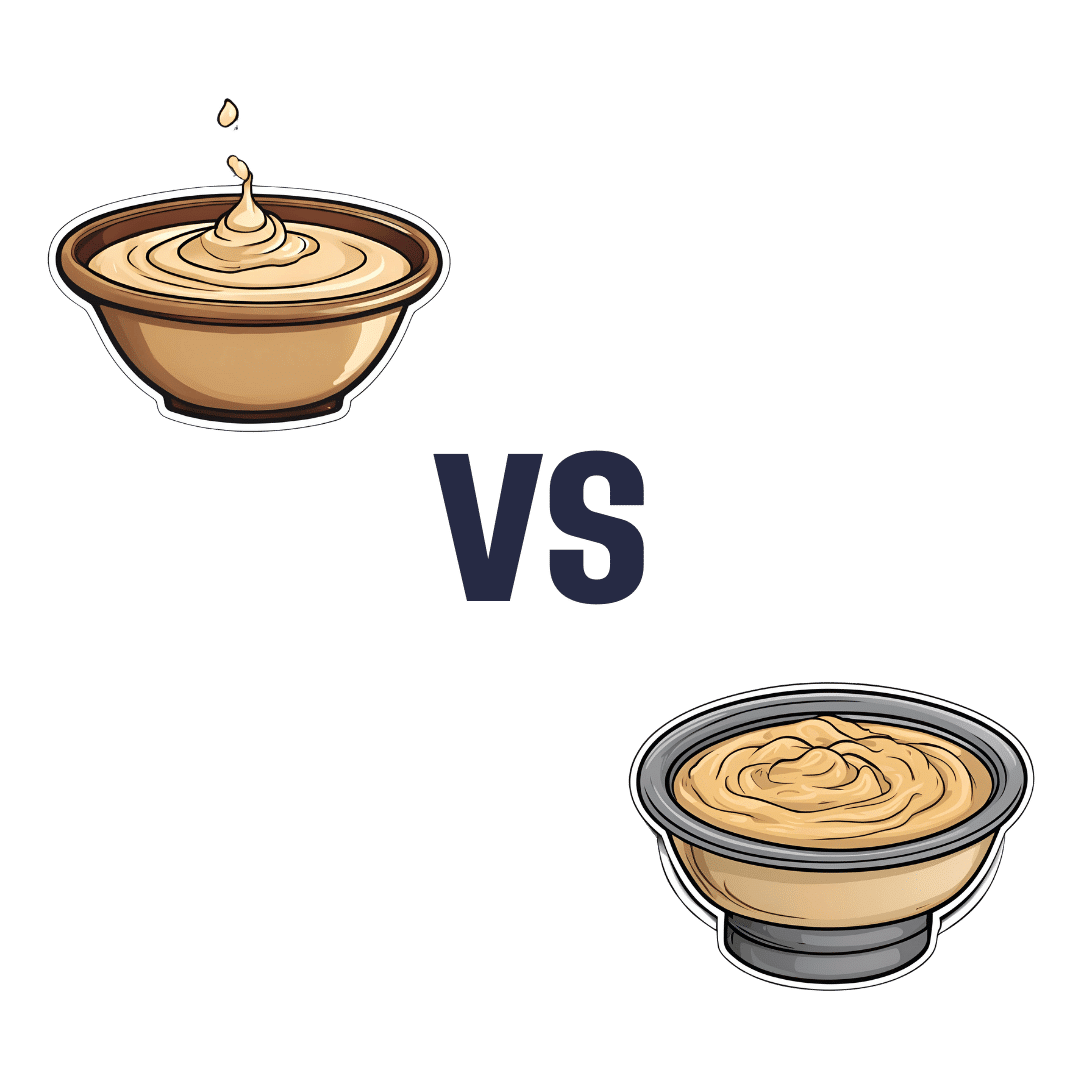
Tahini vs Hummus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tahini to hummus, we picked the tahini.
Why?
Both are great! But tahini is so nutritionally dense, that it makes even the wonder food that is hummus look bad next to it.
In terms of macros, tahini is higher in everything except water. So, higher in protein, carbs, fats, and fiber. In terms of those fats, the fat breakdown is similar for both, being mostly polyunsaturated and monounsaturated, with a small percentage of saturated. Tahini has the lower glycemic index, but both are so low that it makes no practical difference.
In terms of vitamins, tahini has more of vitamins A, B1, B2, B3, B5, B9, E, and choline, while hummus is higher in vitamin B6.
This is a good reason to embellish hummus with some red pepper (vitamin A), a dash of lemon (vitamin C), etc, but we’re judging these foods in their most simple states, for fairness.
When it comes to minerals, tahini has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Meanwhile, hummus is higher in sodium.
Note: hummus is a good source of all those minerals too! Tahini just has more.
In short… Enjoy both, but tahini is the more nutritionally dense by far. On the other hand, if for whatever reason you’re looking for something lower in carbs, fats, and calories, then hummus is where it’s at.
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Broccoli Sprouts & Sulforaphane
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝How much science is there behind sulforaphane / broccoli spirits and its health claims??❞
So, first of all, what it is: sulforaphane is a compound found in Brassica oleracea, of which species broccoli is a cultivar. It’s found in the other Brassica oleracea cultivars too (e.g. cauliflower, various cabbages, Brussels sprouts, kale, etc), but for whatever reason*, most research has been on broccoli and broccoli sprouts.
*Likely the reason is: research begets research—it’s easier to get funding to expand upon previous research, than it is to break ground on researching a different plant, where for the first third of your paper you have almost no existing scientific literature to cite. So once they got started on broccoli sprouts, everything else has been broccoli sprouts too.
And for clarity on what broccoli sprouts are: this means that when broccoli seeds have been germinated and just begun to sprout, they are harvested and eaten. That’s the one-line explanation, anyway; there’s a little more to it than that, so anyone interested should check out our previous main feature:
Good Things Come In Small Packages: Sprout Your Seeds, Grains, Beans, Etc
…and for more depth than we have room for in a one-page article, check out this book we reviewed:
The Sprout Book: Tap Into The Power Of The Planet’s Most Nutritious Food – by Doug Evans
One thing that the science is clear on: sprouts of a given plant indeed have much higher general nutritional density than their “adult” siblings. And in the case of sulforaphane specifically, it’s about 100x higher in broccoli sprouts than in adult broccoli:
Broccoli or Sulforaphane: Is It the Source or Dose That Matters? ← we suggest skipping down to the section “broccoli-based clinical trials”
So, that prompts the next question: do we care?
In other words: is sulforaphane really particularly important?
Sulforaphane vs cancer
The most well-evidenced health-giving property of sulforaphane is its anticancer activity:
Brassicaceae-Derived Anticancer Agents: Towards a Green Approach to Beat Cancer
A lot of the research there is epidemiological rather than RCTs, and where there are RCTs, they are mostly small ones, like this 10-person broccoli soup study about bioavailability (rather than the effects themselves):
Bioavailability of Glucoraphanin and Sulforaphane from High-Glucoraphanin Broccoli
To get into sulforaphane’s anticancer potential in seriousness, we have to look at a lot of in-vitro studies trialling it to limit carcinogenesis, or to shrink tumors with it, or specifically targetting cancer stem cells with it, which make for quite compelling reading:
A quick aside: if you’re reading that and thinking “Why is sonic the hedgehog in here?” it’s because after the observation of the influence of certain genes that influence cuticular denticles (the growth of spikes) on fruit fly larvae (bearing in mind the fruit fly Drosophila melanogaster is used for so much first- or second-line genetic research, being either the go-to or the go-to after the nematode C. elegans) caused the whole group of genes to get called “hedgehog genes” and then it became scientific convention to name each newly researched gene in that set after a different kind of hedgehog. One of them, instead of being named after a real-world hedgehog species like the others, got named after the videogame character.
Unfortunately, this now means that because the gene is associated with a certain congenital brain disorder, sometimes a doctor has to explain to a family that the reason their baby has a brain defect is because of a mutated sonic hedgehog.
Ok, back to talking about cancer. Let’s just quickly drop a few more papers so it’s clear that this is well-established:
- Multi-targeted prevention of cancer by sulforaphane ← this shows how it works on the cellular level
- Cruciferous vegetables: dietary phytochemicals for cancer prevention ← this shows how it works on the population level
However, that’s not the only established benefit:
❝SFN has other beneficial effects in addition to cancer protection. SFN exhibits neuroprotective effects and is implemented in treating conditions such as traumatic brain injury, Alzheimer’s disease and Parkinson’s disease.❞
Source: Sulforaphane in broccoli: The green chemoprevention!! Role in cancer prevention and therapy
Now, after the extract we quoted above, the rest of the section “other health benefits of sulforaphane” includes a lot of speculation, weak science, and/or things attributable to other phytochemicals in broccoli, including various polyphenols, vitamins, and minerals.
About those broccoli spirits
Ok, we know it was a typo, but… Actually, there is something worth mentioning here, and that’s that sulforaphane is only activated when glucoraphanin (its inactive form) comes into contact with myrosinase (an enzyme that’s only released when the plant is damaged).
In other words, it’s necessary to injure the broccoli before consuming it, in order to release the
spiritsmyrosinase. Now, while very few people are out there swallowing adult broccoli plants whole, it could well happen that people might wolf down uncut broccoli sprouts, since they are only small, after all.For this reason, it’s best that broccoli, even if it’s broccoli sprouts, be cut while raw before consumption.
In terms of cooking, heat in excess of 140℃ / 284℉ will destroy the glucoraphanin, and less/no glucoraphanin means less/no sulforaphane.
So, enjoying them raw or lightly steaming them seems to be best for this purpose:
Impact of thermal processing on sulforaphane yield from broccoli (Brassica oleracea L. ssp. italica)
Just want a supplement?
Many studies (including some cited by the research reviews we cited above) deal with sulforaphane in extract form, rather than whole plants, so there’s no shame in taking it that way if you’re not a fan of broccoli.
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
Cynthia’s Thoughts on Intermittent Fasting
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Myth of Breakfast and Snacking
Here at 10almonds we love addressing misconceptions in the health world.
When it comes to eating habits and fasting, we’ve written our own pieces on how to break your fast (otherwise known as break-fast, or breakfast), alongside a general breakdown of intermittent fasting, and a much-requested piece on fasting specifically for women.
Cynthia Thurlow, though, instead of just writing a few articles, has dedicated the majority of her working years to intermittent fasting and, in her TEDx talk (below), makes a strong argument challenging the long-held belief that breakfast is the most important meal of the day.
Cynthia Thurlow’s Two Main Points
Thurlow argues that it’s not what you eat but when you eat that has a more profound impact on health and aging. And she argues this is crucial regardless of your age.
Complementing her views on fasting are her views on snacking; she argues that snacking all day long is outdated advice and can overtax the digestive system, leading to various health issues.
Practical Tips for Starting Intermittent Fasting
To begin intermittent fasting, Thurlow suggests starting with a 12-13 hour fasting window and gradually increasing it to 16 hours.
In terms of food choice, she recommends eating whole, unprocessed foods during eating periods as well as staying well-hydrated with water, coffee, or tea.
But you won’t see results immediately; Thurlow advises giving the strategy a solid 30 days to see results and consulting a healthcare provider if there are any existing health conditions.
You can dive deeper and join the 15 million other people who have listened to her thoughts on fasting by watching her TEDx talk below:
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Languishing – by Prof. Corey Keyes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written before about depression and “flourishing” but what about when one isn’t exactly flourishing, but is not necessarily in the depths of depression either? That’s what this book is about.
Prof. Keyes offers, from his extensive research, hope for those who do not check enough of the boxes to be considered depressed, but who are also definitely more in the lane of “surviving” than “thriving”.
Specifically, he outlines five key ways to make the step from languishing to flourishing, based not on motivational rhetoric, but actual data-based science:
- Learn (creating your personal story of self-growth)
- Connect (building relationships, on the individual level and especially on the community level)
- Transcend (developing psychological resilience to the unexpected)
- Help (others! This is about finding your purpose, and then actively living it)
- Play (this is a necessary “recharge” element that many people miss, especially as we get older)
With regard to finding one’s purpose being given the one-word summary of “help”, this is a callback to our tribal origins, and how we thrive and flourish best and feel happiest when we have a role to fulfil and provide value to those around us)
Bottom line: if you’re not at the point of struggling to get out of bed each day, but you’re also not exactly leaping out of bed with a smile, this book can help get you from one place to the other.
Share This Post
Related Posts
-
Here’s the latest you need to know about bird flu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- Although bird flu continues to spread in wild birds, livestock, and humans, the risk to the public remains low.
- The majority of U.S. bird flu cases have been reported in farm workers who had direct contact with infected birds and cattle. Health officials are working to monitor the spread of the virus and improve protections for those most at risk.
- Recent data suggests that mutations in bird flu viruses could make them more dangerous to humans and potentially increase the risk of a pandemic.
- On January 6, Louisiana health officials confirmed the first U.S. death from bird flu.
Throughout 2024, dozens of human cases of H5N1 bird flu were detected as the virus spreads rapidly in livestock. The current risk to humans is low but not nonexistent. Here’s everything you need to know about the current status and future outlook of H5 bird flu in the United States.
Current U.S. bird flu status (as of January 6, 2025)
As of January 6, 66 human bird flu cases have been reported in eight states. Over half of all cases are in California. The state’s governor declared a state of emergency as a “proactive” action against bird flu on December 18.
On January 6, the Louisiana Department of Health reported the first U.S. bird flu death. The patient, a man over age 65, was previously confirmed to be the first severe bird flu case in the U.S. and the first case linked to backyard flocks. The department emphasized that the risk to the public is low and that no new cases or evidence of human transmission have been detected in the state.
All but two human bird flu cases this year were in farm workers who were exposed to infected livestock. The exposure source of the remaining cases—one in California and one in Missouri—is unknown.
The CDC reported on November 22 that a child in California tested positive for bird flu, the first known pediatric bird flu case in the U.S. However, it is unclear how the child contracted the virus, as they had no known contact with infected animals.
To date, there have been no reports of human transmission of bird flu during the current outbreak. Additionally, most human cases have not been severe, and no deaths have been reported. For these reasons, experts are confident that the bird flu risk to humans remains low.
“In the short term, there is very little threat,” Dr. Scott Roberts, an infectious diseases specialist with Yale Medicine said. “The risk for the general public is so low,” he emphasized to Yale Medicine.
How the U.S. is monitoring bird flu
The CDC continues to monitor the circulation of bird flu in humans as part of its year-round flu monitoring. The agency is also working to improve protections for farm workers, who are at the highest risk of contracting bird flu.
In November 2024, the CDC also announced expanded actions and updated guidance for farm workers, including improved access to and training for using personal protective equipment (such as N95 face masks), more rigorous testing procedures, and increased outreach. These updates followed a CDC report finding that 7 percent of participating dairy workers had signs of a recent bird flu infection. A second CDC study, also released in November, found inadequate use of personal protective equipment among dairy workers on farms with bird flu outbreaks.
After the H5N1 virus was found in raw milk being sold in California, the U.S. Department of Agriculture announced on December 6 that unpasteurized milk must be tested for bird flu. The USDA order also requires dairy farms with positive bird flu cases to cooperate with health officials in disease surveillance.
Is a bird flu pandemic possible?
In early November, a Canadian teen was hospitalized with bird flu caused by a virus that’s closely related to the H5N1 virus circulating in the U.S. The case has troubled experts for a few reasons.
First, it is Canada’s first human bird flu case where the patient was not infected while traveling, and the source of exposure is unknown. Second, the teen experienced severe symptoms and developed a lung infection requiring critical care, raising concern that bird flu infections may be more severe in younger people.
The final and biggest concern about the case is that genetic analysis revealed several changes in the virus’s DNA sequence, called mutations, that could potentially make the virus better able to infect humans. Researchers say that two of those mutations could make it easier for the virus to infect humans, and another one may make it easier for the virus to replicate after infecting a human. However, it’s unclear if the changes occurred before or after the teen was infected.
Scott Hensley, a professor of microbiology at the University of Pennsylvania, told Nature that “this should serve as a warning: this virus has the capacity to switch very quickly into a form that can cause severe disease.”
Notably, even in this more severe case, there is still no evidence of human transmission, which is necessary for a potential bird flu pandemic. However, the case underscores the risk of new and potentially dangerous mutations emerging as the H5N1 virus continues to spread and multiply.
A study published in Science on December 5 found that a genetic change on a protein on the surface of the virus could make it easier for the virus to attach to and infect human cells. But none of the mutations observed in the Canadian case are those identified in the study.
Importantly, the researchers stressed that the ability of the virus to attach to a specific part of human cells “is not the only [factor] required for human-to-human transmission of influenza viruses.”
How to stay safe
Most people are not at high risk of being exposed to bird flu. The virus is spreading between animals and from animals to humans through direct contact. The CDC recommends avoiding the consumption of raw milk products and direct contact with wild birds and potentially infected livestock.
“Pasteurization kills the bird flu virus and other harmful germs that can be found in raw milk,” says a November 24 California Department of Public Health press release. “CDPH advises consumers not to drink raw milk or eat raw milk products due to the risk of foodborne illnesses.”
Additionally, although the annual flu shot does not protect against bird flu, getting vaccinated helps prevent infection with seasonal flu and bird flu at the same time. In very rare instances, getting infected by two influenza viruses at the same time can result in a combination of genetic material that produces a new virus.
This phenomenon, known as antigenic shift, triggered the 2009 swine flu pandemic.
Learn more about how to protect yourself and your loved ones against bird flu.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthy sex drive In Our Fifties
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
Q: What’s a healthy sex drive for someone in their 50s?
A: If you’re happy with it, it’s healthy! If you’re not, it’s not.
This means… If you’re not (happy) and thus it’s not (healthy), you have two main options:
- Find a way to be happier without changing it (i.e., change your perspective)
- Find a way to change your sex drive (presumably: “increase it”, but we don’t like to assume)
There are hormonal and pharmaceutical remedies that may help (whatever your sex), so do speak with your doctor/pharmacist.
Additionally, if a boost to sex drive is what’s wanted, then almost anything that is good for your heart will help.
We wrote about heart health yesterday:
What Matters Most For Your Heart?
That was specifically about dietary considerations, so you might also want to check out:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Severe Complications for Pregnant Veterans Nearly Doubled in the Last Decade, a GAO Report Finds
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Series: Post-Roe America:Abortion Access Divides the Nation
After the Supreme Court overturned Roe v. Wade, ending nearly 50 years of federal protection for abortion, some states began enforcing strict abortion bans while others became new havens for the procedure. ProPublica is investigating how sweeping changes to reproductive health care access in America are affecting people, institutions and governments.
Over the past decade, the rate of veterans suffering severe pregnancy complications has risen dramatically, a new federal report found.
Veterans have raced to the hospital with dangerous infections, kidney failure, aneurysms or blood loss. They’ve required hysterectomies, breathing machines and blood transfusions to save their lives. Between 2011 and 2020, 13 veterans died after such complications.
The report found that among people getting health care benefits through the Department of Veterans Affairs, the rate of severe complications nearly doubled during that time, from about 93 per 10,000 hospitalizations in 2011 to just over 184 per 10,000 hospitalizations in 2020. Black veterans had the highest rates.
The report, which was put together by the Government Accountability Office, also made recommendations for reducing the problem, which focus on conducting more routine screenings throughout pregnancy and in the postpartum period.
“It is imperative that the VA help ensure veterans have the healthiest pregnancy outcomes possible,” the report said, highlighting the increasing number of veterans using the agency’s maternity benefits as well as the troublesome complication rates faced by Black women.
The report’s findings are an unfortunate trend, said Alyssa Hundrup, director of health care at the GAO. The office analyzed data on 40,000 hospitalizations related to deliveries paid for by the VA. It captures a time period before 21 states banned or greatly restricted abortion and the military was thrust into a political battle over whether it would pay for active service members to travel for abortion care if a pregnancy was a risk to their health.
Hundrup, who led the review, said the analysis included hospital records from days after delivery to a year postpartum. The report was mandated after Congress passed a law in 2021 that aimed to address the maternal health crisis among veterans. The law led to a $15 million investment in maternity care coordination programs for veterans.
The report recommended that the VA analyze and collect more data on severe complications as well as data on the mental health, race and ethnicity of veterans who experience complications to understand the causes behind the increase and the reasons for the disparity. The report also states that oversight is needed to ensure screenings are being completed.
Studies show there’s a connection between mental health conditions and pregnancy-related complications, VA officials said.
The report recommended expanding the screening questions that providers ask patients at appointments to glean more information about their mental health, including anxiety and PTSD symptoms. It urged the VA to review the data more regularly.
“You don’t know what you don’t measure,” Hundrup said in an interview with ProPublica.
The VA health system, which historically served a male population, does not provide maternity care at its facilities. Instead, the agency has outsourced maternity care. But when patients were treated by those providers, the VA failed to track whether they were getting screened for other health issues and mental health problems.
Officials hope the improved data collection will help the VA study underlying issues that may lead to complications. For example, do higher rates of anxiety have a connection to rates of high blood pressure in pregnant people?
VA officials are working with a maternal health review committee to monitor the data as it is gathered. The agency recently conducted its first review of data going back five years about pregnancy-related complications, said Dr. Amanda Johnson, acting head of the VA’s Office of Women’s Health, who is overseeing the implementation of the report’s recommendations.
The VA has created a dashboard to monitor pregnant veterans’ health outcomes. The VA’s data analysis team will also examine the impact of veterans’ ages on complications and whether they differ for people who live in urban and rural areas.
VA officials will begin to review mental health screenings conducted by maternal care coordinators in March. The coordinators advocate for veterans, helping them between health care visits, whether their providers are inside or outside the VA.
Johnson said that reducing racial and ethnic disparities is a priority for the agency. In 2018, ProPublica published “Lost Mothers,” a series that shed light on the country’s maternal health crisis. Studies have shown that in the general population, Black women are three times more likely than white women to die from pregnancy-related complications. While deaths made up only a small portion of the bad outcomes for Black veterans cited in the report, VA care could not spare them from elevated rates of severe complications. Johnson said the maternal health crisis also persists within the VA.
“There is a disparity,” Johnson said. “We are not immune to that.”
Research shows pregnant people who have used the VA’s coverage have higher rates of trauma and mental conditions that can increase their risks of complications and bad outcomes.
This may be because many people who join the military enter it having already faced trauma, said Dr. Laura Miller, a psychiatrist and the medical director of reproductive mental health at the VA.
She said veterans with PTSD have higher rates of complications such as preeclampsia, a potentially fatal condition related to high blood pressure, gestational diabetes and postpartum depression. If untreated during pregnancy, depression also increases the likelihood of preterm birth and lingering problems for babies.
Hundrup said she hopes this proactive work will improve maternal health.
“We want these numbers trending in the other direction,” Hundrup said.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: