Superfood Baked Apples
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods, and super-tasty. This is a healthy twist on a classic; your blood sugars will thank you for choosing this tasty sweet delight. It’s also packed with nutrients!
You will need
- 2 large firm baking apples, cored but not peeled
- 1/2 cup chopped walnuts
- 3 tbsp goji berries, rehydrated (soak them in warm water for 10–15minutes and drain)
- 1 tbsp honey, or maple syrup, per your preference (this writer is also a fan of aged balsamic vinegar for its strong flavor and much milder sweetness. If you don’t like things to be too sweet, this is the option for you)
- 2 tsp ground sweet cinnamon
- 1 tsp ground ginger
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 180℃ / 350℉ / gas mark 4
2) Mix the chopped walnuts with the goji berries and the honey (or whatever you used instead of the honey) as well as the sweet cinnamon and the ginger.
3) Place the apples in shallow baking dish, and use the mixture you just made to stuff their holes.
4) Add 1/2 cup water to the dish, around the apples. Cover gently with foil, and bake until soft.
Tip: check them every 20 minutes; they may be done in 40 or it may take 60; in honesty it depends on your oven. If unsure, cook them for longer at a lower temperature.
5) Serve warm.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- From Apples to Bees, and High-Fructose C’s
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars
- Honey vs Maple Syrup – Which is Healthier?
- A Tale Of Two Cinnamons ← this is important, about why we chose the sweet cinnamon
- Ginger Does A Lot More Than You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Cold Truth About Respiratory Infections
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Pathogens That Came In From The Cold
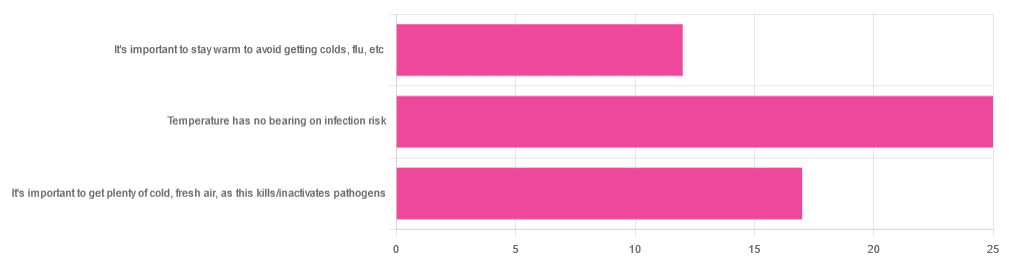
Yesterday, we asked you about your climate-themed policy for avoiding respiratory infections, and got the above-depicted, below-described, set of answers:
- About 46% of respondents said “Temperature has no bearing on infection risk”
- About 31% of respondents said “It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens”
- About 22% of respondents said “It’s important to stay warm to avoid getting colds, flu, etc”
Some gave rationales, including…
For “stay warm”:
❝Childhood lessons❞
For “get cold, fresh air”:
❝I just feel that it’s healthy to get fresh air daily. Whether it kills germs, I don’t know❞
For “temperature has no bearing”:
❝If climate issue affected respiratory infections, would people in the tropics suffer more than those in colder climates? Pollutants may affect respiratory infections, but I doubt just temperature would do so.❞
So, what does the science say?
It’s important to stay warm to avoid getting colds, flu, etc: True or False?
False, simply. Cold weather does increase the infection risk, but for reasons that a hat and scarf won’t protect you from. More on this later, but for now, let’s lay to rest the idea that bodily chilling will promote infection by cold, flu, etc.
In a small-ish but statistically significant study (n=180), it was found that…
❝There was no evidence that chilling caused any acute change in symptom scores❞
Read more: Acute cooling of the feet and the onset of common cold symptoms
Note: they do mention in their conclusion that chilling the feet “causes the onset of cold symptoms in about 10% of subjects who are chilled”, but the data does not support that conclusion, and the only clear indicator is that people who are more prone to colds generally, were more prone to getting a cold after a cold water footbath.
In other words, people who were more prone to colds remained more prone to colds, just the same.
It’s important to get plenty of cold, fresh air, as this kills/inactivates pathogens: True or False?
Broadly False, though most pathogens do have an optimal operating temperature that (for obvious reasons) is around normal human body temperature.
However, given that they don’t generally have to survive outside of a host body for long to get passed on, the fact that the pathogens may be a little sluggish in the great outdoors will not change the fact that they will be delighted by the climate in your respiratory tract as soon as you get back into the warm.
With regard to the cold air not being a reliable killer/inactivator of pathogens, we call to the witness stand…
Polar Bear Dies From Bird Flu As H5N1 Spreads Across Globe
(it was found near Utqiagvik, one of the northernmost communities in Alaska)
Because pathogens like human body temperature, raising the body temperature is a way to kill/inactivate them: True or False?
True! Unfortunately, it’s also a way to kill us. Because we, too, cannot survive for long above our normal body temperature.
So, for example, bundling up warmly and cranking up the heating won’t necessarily help, because:
- if the temperature is comfortable for you, it’s comfortable for the pathogen
- if the temperature is dangerous to the pathogen, it’s dangerous to you too
This is why the fever response evolved, and/but why many people with fevers die anyway. It’s the body’s way of playing chicken with the pathogen, challenging “guess which of us can survive this for longer!”
Temperature has no bearing on infection risk: True or False?
True and/or False, circumstantially. This one’s a little complex, but let’s break it down to the essentials.
- Temperature has no direct effect, for the reasons we outlined above
- Temperature is often related to humidity, which does have an effect
- Temperature does tend to influence human behavior (more time spent in open spaces with good ventilation vs more time spent in closed quarters with poor ventilation and/or recycled air), which has an obvious effect on transmission rates
The first one we covered, and the third one is self-evident, so let’s look at the second one:
Temperature is often related to humidity, which does have an effect
When the environmental temperature is warmer, water droplets in the air will tend to be bigger, and thus drop to the ground much more quickly.
When the environmental temperature is colder, water droplets in the air will tend to be smaller, and thus stay in the air for longer (along with any pathogens those water droplets may be carrying).
Some papers on the impact of this:
- Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections
- A Decrease in Temperature and Humidity Precedes Human Rhinovirus Infections in a Cold Climate
So whatever temperature you like to keep your environment, humidity is a protective factor against respiratory infections, and dry air is a risk factor.
So, for example:
- If the weather doesn’t suit having good ventilation, a humidifier is a good option
- Being in an airplane is one of the worst places to be for this, outside of a hospital
Don’t have a humidifier? Here’s an example product on Amazon, but by all means shop around.
A crock pot with hot water in and the lid off is also a very workable workaround too
Take care!
Share This Post
-
8 Pillars of Weight Loss Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Surprise, diet is #6 and exercise is #7:
How many do you do?
If your body is a temple, these are its eight pillars:
- Emotional freedom and resilience: understanding how the mind works and using techniques such as CBT, neurolinguistic programming, and meditation to reduce psychological stress and improve self-awareness.
- Vagal tone improvement: techniques to get the body out of fight-or-flight mode, improving blood flow, digestion, and reducing chronic pain.
- Lymphatic system support: to enhance your body’s internal cleanup system, boost energy, and alleviate pain.
- Gut health optimization: supporting digestion and gut health, so that your gut can work efficiently.
- Hormonal balance: addressing hormone imbalances to improve overall health, as well as supporting a healthy metabolism and weight loss.
- Dietary choices: choosing a sustainable diet that balances blood sugar, boosts metabolism, and suits your personal needs.
- Exercise and mobility: developing a sustainable workout plan that promotes fat loss, joint health, and muscle building.
- Habit formation: developing routines and habits to maintain progress and prevent relapse into old patterns.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Lose Weight (Healthily!) ← our own main feature on the topic, detailing the best kinds of diet and exercise adjustments, as well as how to go about tending to some of the other factors mentioned above
Take care!
Share This Post
-
International Women’s Day (and what it can mean for you, really)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How to not just #EmbraceEquity, but actually grow it, this International Women’s Day!
It’s International Women’s Day, and there’s a lot going on beyond the hashtagging! So, what’s happening, and how could you get involved in more than a “token” way in your workplace, business, or general life?
Well, that depends on your own environment and circumstances, but for example…
A feminist policy for productivity in the food sector?
We tend to think that in this modern world, we all have equal standing when it comes to productivity, food, and health. And yet…
❝If women do 70 per cent of the work in agriculture worldwide, but the land is mainly owned by men, then we don’t have equity yet. If in Germany, only one-tenth of female farmers manage the farm on which they work on, while they also manage the household, then there is no equity yet❞
~ Lea Leimann, Germany
What to do about it, though? It turns out there’s a worldwide organization dedicated to fixing this! It’s called Slow Food.
Their mission is to make food…
- GOOD: quality, flavorsome and healthy food
- CLEAN: production that does not harm the environment
- FAIR: accessible prices for consumers and fair conditions and pay for producers
…and yes, that explicitly includes feminism-attentive food policy:
Read all about it: Slow Food women forge change in the food system
Do you work in the food system?
If so, you can have an impact. Your knee-jerk reaction might be “I don’t”, but there are a LOT of steps from farm-to-table, so, are you sure?
Story time: me, I’m a writer (you’d never have guessed, right?) and wouldn’t immediately think of myself as working “in the food system”.
But! Not long back I (a woman) was contracted by a marketing agent (a woman) to write marketing materials for a small business (owned by a woman) selling pickles and chutneys across the Australian market, based on the recipes she learned from her mother, in India. The result?
I made an impact in the food chain the other side of the planet from me, without leaving my desk.
Furthermore, the way I went about my work empowered—at the very least—myself and the end client (the lady making and selling the pickles and chutneys).
Sometimes we can’t change the world by ourselves… but we don’t have to.
If we all just nudge things in the right direction, we’ll end up with a healthier, better-fed, more productive system for all!
Share This Post
Related Posts
-
The Core Program: – by Peggy Brill
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a specialist women’s physiotherapist, has produced not only an exercise program, but also an explanation of various body-related matters can be easily neglected—but also, with the right knowledge and a small daily commitment of practice, easily addressed.
Thus, thus subtitular claim of “15 minutes a day that can change your life” is referring to a daily 15-minute exercise session, that’s very Pilates-like in its functional strength and mobility focus with little or no equipment, without actually being Pilates.
After some introductory chapters discussing the things we need to know in order to implement the program with full understanding, she gets into the program itself, which consists of three progressive parts:
- a foundation to get going
- an intermediate level to get things truly into good shape, and
- an advanced level for if one wants to take things further.
She also provides extra advice on maintaining what one gained, taking the program forwards for life.
The program is optimized for women, but there’s nothing truly exclusive to women here, just, occasional “this affects women more” things to include.
The style is a little dated (the book being published in 2003), but this does not meaningfully affect the content, as the information itself is timeless.
Bottom line: if you’d like to get into good condition without overcomplicating things and without needing a lot of resources, this book is quite a comprehensive course!
Click here to check out The Core Program, and get into shape sustainably!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Exhausted To Energized – by Dr. Libby Weaver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are very many possible causes of low energy; some are obvious; some are not.
Dr. Weaver goes through a comprehensive list that goes beyond the common, to encompass also the “not rare” options—how to test for them where appropriate, and how to improve/fix them where appropriate.
Thus, she talks us through the marvels of mitochondria (including how to keep them happy and healthy and how to promote the generation of new ones), antioxidant defense mechanisms, coenzyme Q10 and friends, B vitamins of various kinds, macronutrients, the autonomic nervous system, sleep and its many factors, blood oxygenation, digestive issues, what’s going on in the spleen, the gallbladder, the liver, the kidneys, the adrenal glands, our thyroid goings-on in all its multifarious wonders, minerals like iodine, iron, magnesium, zinc, our epigenetic factors, and even psychological considerations ranging from stress to grief. In short—and we have shortened the list to pick out particularly salient points—quite a comprehensive rundown of the human body to make your human body less run-down.
The style is on the very readable pop-science, and/but she does bring her professional knowledge to bear on topic (her doctorate is a PhD in biochemistry, and it shows; a lot of explanations come from that angle).
Bottom line: if you are often exhausted and would rather be energized, this this book almost certainly address at least a couple of things you probably haven’t considered—and even just one would make it worthwhile.
Click here to check out Exhausted To Energized, go from exhausted to energized!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Best Mobility Exercises For Each Joint
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Stiff joints and tight muscles limit movement, performance, and daily activities. They also increase the risk of injury, and increase recovery time if the injury happens. So, it’s pretty important to take care of that!
Here’s how
Key to joint health involves understanding mobility, flexibility, and stability:
- Mobility: active joint movement through a range of motion.
- Flexibility: muscle lengthening passively through a range of motion.
- Stability: body’s ability to return to position after disturbance.
Different body parts have different needs when it comes to prioritizing mobility, flexibility, and stability exercises. So, with that in mind, here’s what to do for your…
- Wrists: flexibility and stability (e.g., wrist circles, loaded flexions/extensions).
- Elbows: Stability is key; exercises like wrist and shoulder movements benefit elbows indirectly.
- Shoulders: mobility and stability; exercises include prone arm circles, passive hangs, active prone raises, easy bridges, and stick-supported movements.
- Spine: mobility and stability; recommended exercises include cat-cow and quadruped reach.
- Hips: mobility and flexibility through deep squat hip rotations; beginners can use hands for support.
- Knees: stability; exercises include elevated pistols, Bulgarian split squats, lunges, and single-leg balancing.
- Ankles: flexibility and stability; exercises include lunges, prying goblet squats, and deep squats with support if necessary.
For more on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Building & Maintaining Mobility
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: